|
K.P. Sanghvi
Peter Steer
From
the Department of Neonatology, Mater Misericordiae Public Hospital, South Brisbane, Queensland, Australia.
Reprint requests: Dr. K.P. Sanghvi, Siddhachal Darshan, Sheth Motisha Lane, Byculla,
Mumbai 400 027, India.
Manuscript received: December 19,1997; Initial review completed: March 4, 1998;
Revision accepted: May 6, 1998
Blood pressure (BP) is an important parameter regularly
monitored in critically ill neonates. Noninvasive techniques
estimate blood pressure by analyzing changes in flow produced by
compressing an artery in an extremity, and monitoring an effect related to the compression, either. palpation or auscultation assessment, or with some externally placed transducer. Pulse oximetry with sphygmomanometry is another non-invasive method used to measure blood pressure in adults(1-5) and more recently in neonates(6j. With this technique there is a loss of the plethysmographic wave form on the pulse oximeter, as the pulsatile blood flow is obliterated with increase in cuff pressure.
Intra-arterial blood pressure measurement though the most accurate
method is expensive and not readily available. Cost constraints in
developing countries make BP measurements using this technique unfeasible. An accurate, inexpensive and user friendly alternative would be valuable. The aim of this study was to assess the accuracy of blood pressure measurement using a combination of a mercury sphygmomanometer and a pulse oximeter in newborn infants.
Subjects and Methods
This prospective study was performed over a two month period in the Neonatal Intensive Care Unit (NICU)
of the Mater Mothers' Hospital, Brisbane. Only those babies
irrespective of gestational age and birth weight and managed with
an arterial line (umbilical or peripheral) as a component of their usual clinical care, were included in the study. The intra-arterial blood' pressure was measured using a Baxter "Uniflow" disposable transducer and an Athena monitor and blood pressure module (Simonsen and Weel)
the signal in which was band filtered to 70Hz. Non- invasive blood
pressure was measured using an appropriately sized(7) disposable neonatal blood pressure cuff (Disposa-cuff- Critikon-Johnson and Johnson). This was connected to a standard mercury sphygmomanometer. No preference for any specific limb to measure the BP was shown. the BP cuff was wrapped around the arm or thigh ipsilateral and proximal to the sensor of the pulse oximeter (CSI-502-Criticare) by the nursing staff during routine cares so that the infant was not unduly disturbed. The procedure used to measure the BP was as follows: The transducer was zeroed prior to each measurement. Any air bubbles if present were removed. The pulse oximeter mode was set to display continuous plethysmographic wave pattern. When a stable plethysmographic wave was
obtained,
the BP cuff was inflated slowly in 2 mm increments. The SBP on the sphygmomanometer was noted when the plethysmographic waveform on the oximeter changed from a wave pattern to a straight line display. The intra-arterial BP reading was also noted concurrently. The cuff was inflated a further 20 mm and then deflated in decrements of 2 mm till the wave pattern on the pulse oximeter reappeared. 'The SBP recordings on the sphygmomanometer and on the transducer via the Athena monitor were again noted. Fifty observations were made in 19 infants.
Statistical Analysis
Pearson's correlation coefficients were determined for intra-arterial SBP (IASBP) on the Athena monitor and SBP on the sphygmomanometer at disappearance
DOWSBP and reappearance (ROWSBP)
of plethysmograhic wave pattern on the pulse oximeter. Agreement between methods
(IASBP with DOWSBP and ROWSBP respectively) is reported according to the method described by Bland and Altman(8).
Results
The mean gestational age of the infants studied was 30.6±5.1 weeks (range 24-41 weeks) and the mean birth weight was
1670±888.3 g (range 523-3738g). The
mean post-natal age at which
the study was done
was 3.9 ± 3.4 days (range 1-19 days). Thirty-eight readings on umbilical arterial lines and 12 on peripheral arterial lines were compared with 20 sphygmomanometry observations on right lower limb, 19 on left lower limb, three on right upper
limb and four
on left upper limb. All babies were ventilated and sedated
with
morphine and/or midazolam. No infant was on vasoactive drugs (dopamine/ dobutamine).
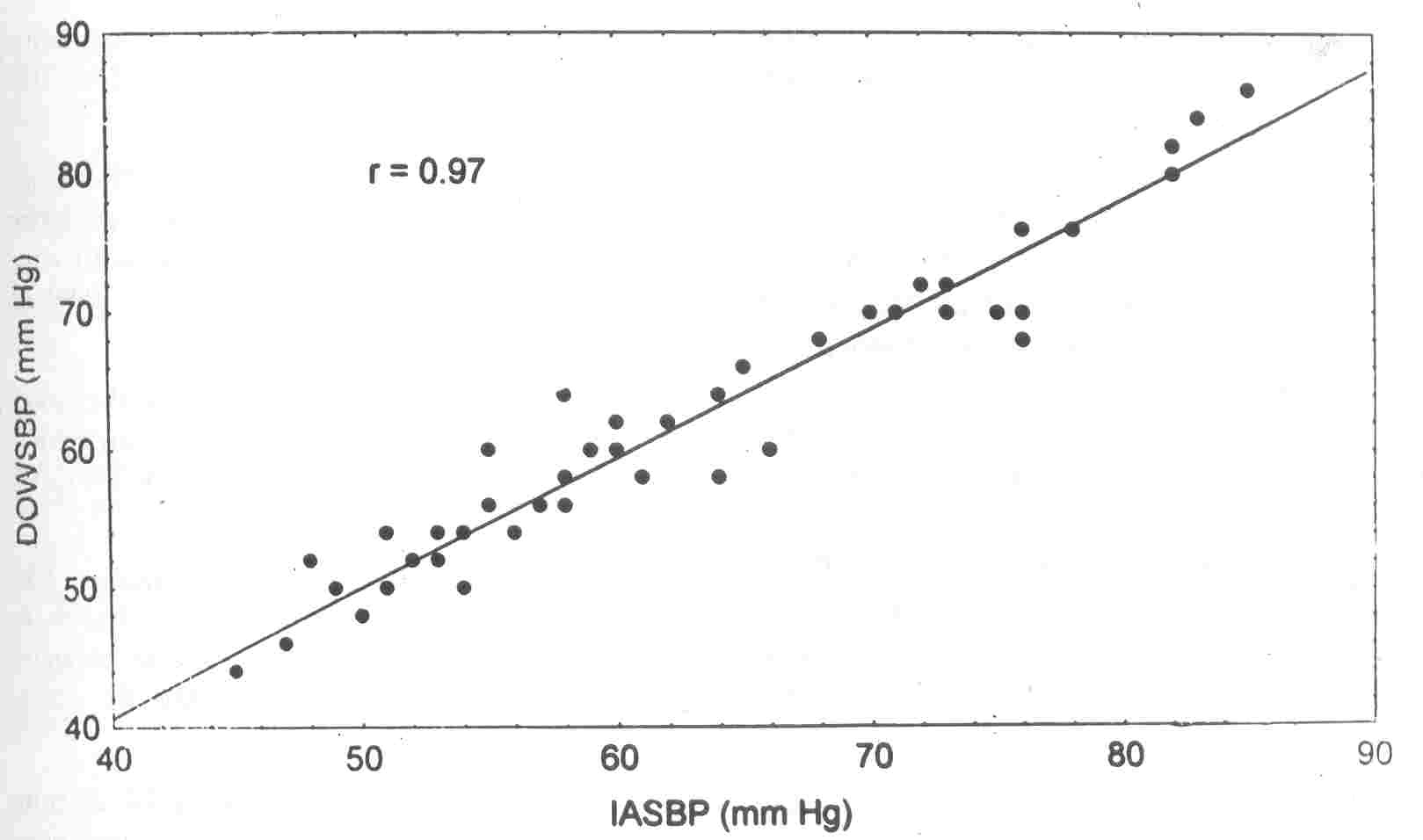
There was excellent correlation between IASBP and DOWSBP on the pulse oximeter
(r
=
0.97) (Fig. 1) But the correlation between ROWSBP on the pulse oximeter and
IASBP was poor (r
=
0.48).
ROWSBP on the
pulse oximeter also correlated poorly with mean and diastolic pressures noted via the transducer, although the. relationship to
diastolic BP
(r=0.60)
was greater than either
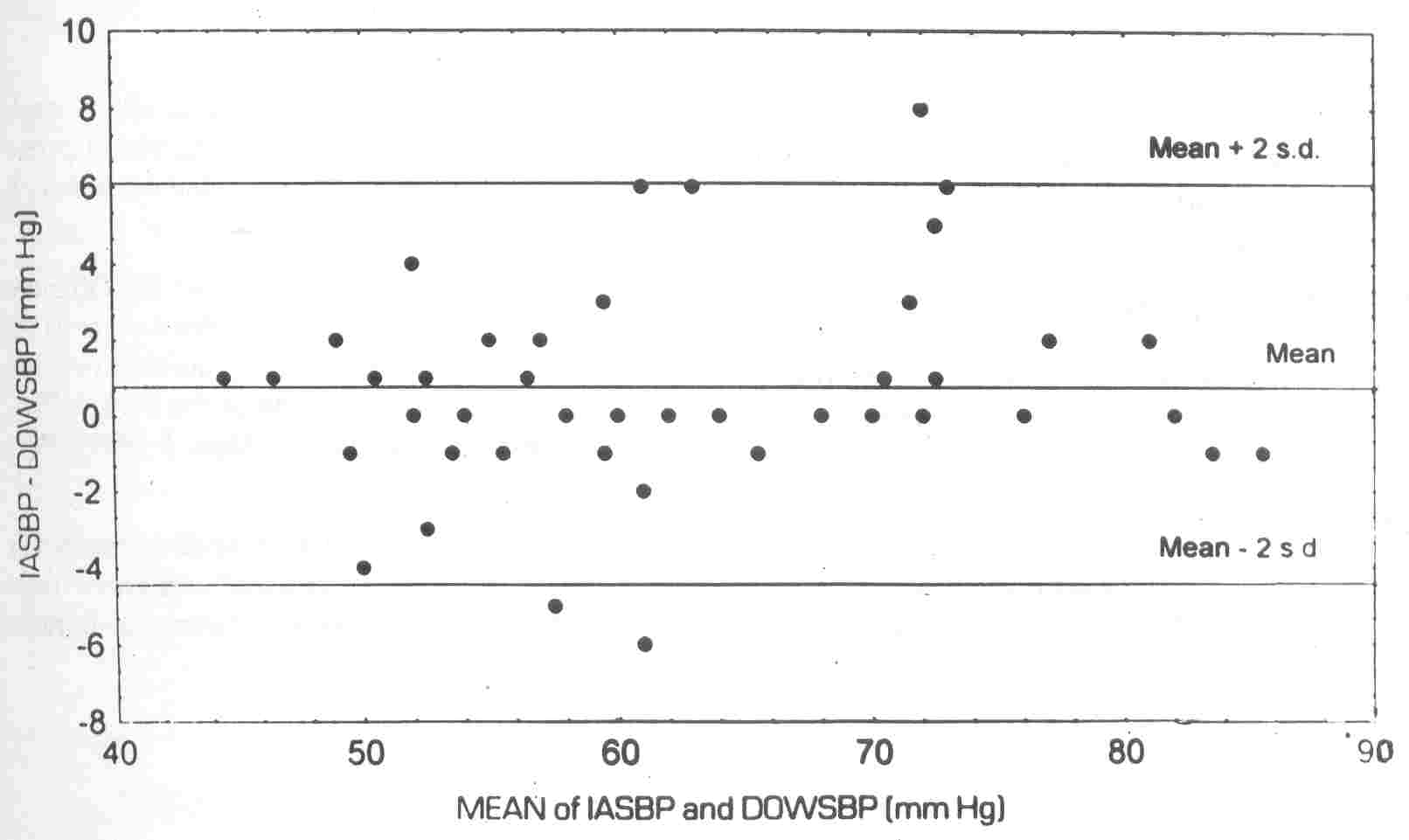
mean (r=0.53) or systolic (r=0.48). Fig. 2 summarizes the degree of agreement between the two methods. The bias, or mean difference between the IASBP and
DOWSBP was 0.76 points. The limits
of agreements (the
mean difference
±
2 SD)
between IASBP and DOWSBP were 4.6 to 6.1.
 |
|
Fig. 1. Plot of IASBP against DOWSBP with line of equality
|
 |
|
Fig. 2. Difference against mean of IABSP and DOWSP |
Discussion
This study reports a
simple
and
inexpensive method of non-invasive BP measurement. No attempt was made to compare this measurement tool with other non-invasive methods. Sphygmomanometry with pulse oximetry can be used to measure SBP
without additional investment as a pulse oximeter is available in most NICUs.
This study showed both good correlation and agreement between DOWSBP and IASBP.
However, in contrast to other published data, in both adults and neonates(4- 6), we could find no correlation between ROWSBP and IASBP. In the only previous
report
of this technique
in neonates,
Langbaum
et al.(6) documented good
agreement
of
IASBP with sphygmomanom- eter SBP recordings at the time
of both
reappearance and disappearance of wave. The different findings may result from the
recordings'
of
ROWSBP in our study at the
time of complete re-appearance of the plethysmographic waveform. The recordings were not taken at the first deviation from
the straight line pattern, as
this
early deviation may represent artifact. This may also be oximeter dependent, as no
other
study
has used Critic are CSI pulse oximeters. Previous studies have either used the Nellcor N-100(1) or the Ohmeda Biox 3700(2-4,6)
pulse oximeter and have not stated what constituted reappearance of waveform. Langbaum. et al.(6) despite finding good
agreement between ROWSBP and IASBP believe that readings performed during BP cuff inflation (disappearance of waveform) are more reliable and practical. Talke et al.(2) used only ROWSBP to record SBP and Caulkett et al.(5) recommend ROWSBP to measure SBP as their findings suggested measurement of ROWSBP is associated with less bias and hence better precision. Langbaum et al.(6) however, found no improvement in precision with additional in- formation of ROWSBP. In contrast, the findings of this study suggest the most practical and reliable approach is to observe the plethysmographic wave pattern straightening (disappearing) on cuff inflation.
This study was performed prior to the publication of Langbuam et al.(6). We confirmed in newborn infants that non-invasive measurement of SBP, with sphygmomanometry and pulse oximeter
is accurate and reliable. In contrast to other studies, the measurement was accurate only when taken with inflation of cuff pressure and the observations of SBP at the disappearance of the pulse waveform.
Acknowledgements
We are grateful to Andrew Shearman, Respiratory Technician, for helping with the statistical analysis.
|
1.
Wallace CT, Baker JD, Alpert CC, Tankersley C], Conroy JM, Kern RE. Comparison of
blood pressure measurements by Doppler and by pulse oximetry techniques. Anesth Analg 1987; 16: 1018- 1019.
2. Talke PO, Nichols RJ, Traber DL. Does measurement of systolic blood pressure with pulse oximeter correlate with Con- ventional methods.
J
Clin Monit 1990; 6: 5-9.
3.
Talke PO. Measurements of systolic blood pressure using pulse oximetry during helicopter flight. Crit Care Med 1991; 19: 934-937.
4.
Chawla. R, Kumarvel V, Girdhar KK, Sethi AK, Indrayan A, Bhattacharya A. Can pulse oximetry be used to measure systolic blood pressure. Anesth Analg 1992; 74: 196-200.
5.
Caulkett NA, Duke T, Bailey JV. A comparison of systolic blood pressure measurement obtained using a pulse oximeter and dired: systolic blood pressure in anesthetized sows. Can
J
Vet Res 1994; 125:
591-595.
6.
Langbaum M, Eyal FG. A practical and reliable method of measuring blood pres- sure in the neonates by pulse oximetry.
J
Pediatr 1994;125: 591-595.
7.
Swiet M de, Dillon MJ, Littler W, O'Brien E, Padfield PL, Petrie Je. Measurement of blood pressure in children: Recommendations of a working party of the British Hypertension Society. Br Med
J
1989; 299:
497.
8.
Bland MJ, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307-310.
|
