|
|
|
Indian Pediatr 2016;53:
394-397 |
 |
Lactose and Fructose
Intolerance in Turkish Children with Chronic Abdominal Pain
|
|
Özlem Yüce, Ayhan Gazi Kalayci, Atakan Comba, Esra
Eren and Gönül Caltepe
From Department of Pediatric Gastroenterology,
Ondokuz Mayis University, Samsun, Turkey.
Correspondence to: Dr Özlem Yüce, Ondokuz Mayis
University, Faculty of Medicine, Department of Pediatric
Gastroenterology, Samsun, Turkey.
Email: [email protected]
Received: April 25, 2015;
Initial review: September 07, 2015;
Accepted: March 15, 2016.
|
Objective: To investigate the prevalence of lactose and
fructose intolerance in children with chronic abdominal pain.
Methods: Hydrogen breath tests were done
to detect lactose and fructose malabsorption in 86 children with chronic
abdominal pain (44 irritable bowel syndrome, 24 functional abdominal
pain and 17 functional abdominal pain syndrome as per Rome III criteria)
presenting to a Pediatric Gastroentreology department.
Results: 14 (16.3%) of patients
were diagnosed with lactose intolerance and 11 (12.8%) with fructose
intolerance.
Conclusions: Lactose and fructose
intolerance in children can lead to chronic abdominal pain and symptoms
improve with dietary modifications.
Keywords: Diagnosis, Etiology, Functional gastrointestinal
disorders.
|
|
C
hronic abdominal pain is a symptom that can
affect patients physically, psychologically and socially. It affects
13-38% of school-age children [1]. Studies in recent years, particularly
in adults, have reported that lactose and fructose intolerance can cause
chronic abdominal pain [2-6]. However, the data are insufficient in
childhood [3,5,7].
This study was planned to investigate the prevalence
of lactose and fructose intolerance in children with chronic abdominal
pain.
Methods
Children between the ages of 4 and 18 years,
presenting with chronic abdominal pain were included in the study.
Chronic abdominal pain was defined as three or more episodes of pain or
discomfort capable of affecting daily activity lasting for at least 3
months [8]. Organic causes were excluded. Patients with excessive
bacterial growth identified using the Hydrogen breath test (HBT), and
those with a history of antibiotic, proton pump inhibitor, laxative or
probiotic use were also excluded. The study was approved by the Ondokuz
Mayis University Medical Research and Ethical Committee.
The HBT was performed using a gas analyzer (Bedfont
Gastro+Gastrolyzer, ME13QX, Great Britain) with 1 ppm sensitivity.
Patients were given a carbohydrate-poor diet before the HBT. Following
the measurement of patients first basal hydrogen value in breath after
8-h fasting, measurements continued for 3 h every 30 minutes with
patients drinking test substances. Lactulose HBT was first performed to
identify patients with excessive bacterial growth. Lactose was given in
a 2 g/kg dose (maximum 25 g), and fructose was given at a dose of 1 g/kg
(maximum 50 g) in 25% concentration. Tests with an increase in hydrogen
levels of 20 ppm over basal levels were regarded as positive [3,9,10].
Appropriate dietary adjustments were made in children
diagnosed with lactose or fructose malabsorption. A symptom score
ranging from 0 and 3 (0: none, 1: mild, 2: present, 3: severe) for
abdominal pain, bloating, flatulence, headache, vomiting and diarrhea
was recorded [5]. In addition, frequency of abdominal pain per week and
days of school missed per month, and frequency of difficulty in sleeping
were recorded.
SPSS 15 was used for statistical analysis.
Categorical data were analyzed using the Pearson and Fisher chi-square
test. Analysis of variance (ANOVA) was used for group comparisons of
normally distributed values, and the Kruskall Wallis test for
non-normally distributed parameters. Student t test was used to
compare differences of normally distributed means between two groups and
the Mann-Whitney U test for comparing means between non-normally
distributed data. The Wilcoxon test was employed in pre- and post-diet (intragroup)
analysis. Significance was set at P<0.05 for all results.
Results
Eighty-six patients, (52 girls), were enrolled in the
study. When patients were assessed using Rome III criteria, 44 (51.2%)
were diagnosed with irritable bowel syndrome (IBS). Functional abdominal
pain was present in 24 (27.9%) patients and functional abdominal pain
syndrome in 17 (19.8%). One patient was diagnosed with functional
dyspepsia.
Carbohydrate intolerance was observed in 27 patients;
14 (16.3%) had lactose intolerance, 11 (12.8%) had fructose intolerance
and 2 (2.3%) patients had combined lactose and fructose intolerance (Table
I).
TABLE I Characteristics of Children with Positive or Negative Lactose and Fructose Breath Tests (N=86)
|
L(+), (n-14) |
F(+), (n=11) |
LF(-), (n=59) |
P value |
|
Age (y), mean (SD) |
11.9 (3.6) |
9.8 (3.6) |
10.8 (3.5) |
0.36 |
|
Female gender, n (%) |
11 (78.6) |
6 (54.5) |
34 (57.6) |
0.32 |
|
BMI (kg/ m²), mean (SD) |
21 (2.2) |
19.7 (2.1) |
20.6 (2.2) |
0.38 |
|
History of allergy, n(%) |
5 (35.7) |
2 (18.2) |
14 (23.7) |
0.55 |
|
L(+) Lactose hydrogene breath tests were positive, F(+)
Fructose hydrogene breath tests were positive, LF(-) Lactose and
fructose hydrogene breath tests were negative. Two children had
positive breath tests for both lactose and fructose. |
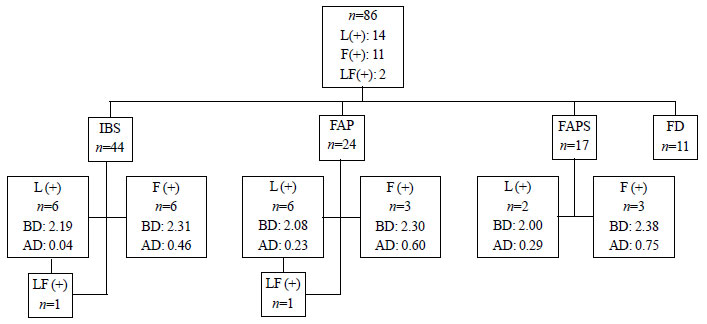
Carbohydrate intolerance was observed in 12 (27.2%)
patients with IBS, 10 (41.6%) patients with functional abdominal pain
and 5 patients (29.4%) with functional abdominal pain syndrome (Fig.
1). Patients demographic data and HBT results are shown in
Table II. No significant difference was determined between IBS,
functional abdominal pain and functional abdominal pain syndrome in
terms of age, gender and prevalence of lactose and fructose intolerance
(P=0.71; P=0.749; P= 0.40 and P=0.80,
respectively).
 |
|
Fig. 1 IBS: Irritable bowel
syndrome, FAP: Functional abdominal pain, FAPS: Functional
abdominal pain syndrome, FD: Functional Dyspepsia L(+) Lactose
hydrogene breath tests were positive, F(+) Fructose hydrogene
breath tests were positive, LF(+) Lactose and fructose hydrogene
breath tests were positive, BD: Abdominal pain score of before
diet, AD: Abdominal pain score of after diet
|
TABLE II Demographic Data of Patients and HBT Results
|
Vriable, n(%) |
IBS (n=44) |
FAP (n=24) |
FAPS (n=17) |
|
*Age, y |
10.6 (3.7) |
10.9 (3.4) |
11.8 (3.2) |
|
Females |
30 |
13 |
9 |
|
L(+) |
6 (13.6) |
6 (25) |
2 (11.7) |
|
F(+) |
5 (11.4) |
3 (12.5) |
3 (17.7) |
|
LF(+) |
1 (2.2) |
1 (4.1) |
0 |
|
IBS: Irritable bowel syndrome, FAP: Functional abdominal pain,
FAPS: Functional abdominal pain syndrome, L(+): Positive Lactose
hydrogene breath tests, F(+): Positive Fructose hydrogene
breath tests, LF(+): both hydrogen breath tests positive; LF(-)
Both hydrogen breath tests negative; *Values in mean (SD); All
comparisons P>0.05. |
One patient with lactose intolerance dropped out from
the study, and two failed to comply with their diets. Symptoms resolved
entirely in 8 of the 11 patients (72.7%) at the end of the 2nd month,
and decreased in the other three. A significant decrease was observed in
the severity of abdominal pain, nausea, bloating and days of school
missed (P=0.003, P=0.002, P=0.015, P=0.024
and P=0.046, respectively) (Web Fig. 1).
One patient with fructose intolerance dropped out
from the study and four failed to comply with their diets. Symptoms did
not resolve in one of the six patients monitored, decreased in three and
resolved completely in two. A significant decrease was observed after
diet in abdominal pain in patients with fructose intolerance (P=0.04)
(Web Fig. 2).
Discussion
In this study, the prevalence of lactose and fructose
intolerance in children with chronic abdominal pain was observed to be
16.3% and 12.8%, respectively. Symptoms resolved entirely in 10
HBT-positive patients in response to the modified diet. Two of these
were from the fructose group and 8 from the lactose group.
Earlier studies aimed at determining the prevalence
of lactose intolerance in children with chronic abdominal pain have
reported estimates of 20-30% [3,11,12]. Excessive bacterial growth in
the gut is known to lead to false positive outcomes at HBT. Nucera,
et al. [13] reported a level of lactose malabsorption of 83% before
treatment of excessive bacterial growth at HBT in patients with IBS, and
a level of 48% after treatment. The fructose malabsorption level was 75%
before treatment, falling to 25% after treatment. It has therefore been
suggested that breath tests are more reliable for identifying lactose
and fructose malabsorption, and should be performed after excluding
excessive bacterial growth [13].
Lactose malabsorbtion can cause abdominal fullness,
bloating, nausea, abdominal pain, flatulence, and diarrhea, which are
similar to the symptoms of IBS. However, it is unclear if these
digestive disorders contribute to or cause the symptoms of IBS. Some
previous studies have concluded that there is no evidence that
lactose-free diets benefit children with IBS [7]. While the mechanism
involved in the lack of symptoms with carbohydrate intolerance is
uncertain, the common view is that individual differences are
significant in the presence of symptoms. In the same way, responses to
diet therefore also exhibit individual differences. Research studies
show that a proper diagnosis and effective dietary intervention
significantly reduces the severity and frequency of gastrointestinal
symptoms in IBS [14,15]. In our study, symptoms improved markedly with
lactose free diet.
Limitations to this study include absence of healthy
controls. Additionally, our patients on modified diets were not
regularly followed-up by clinical examination.
In conclusion, lactose and fructose intolerance may
be common in children with chronic abdominal pain. Large-scale
controlled studies are needed to confirm our findings.
Contributors: ÖY, AGK: designed the study,
collected and analyzed the data, and drafted the manuscript; AC, EE:
supervision of the work, collection of data; GC: literature search and
drafted the manuscript; ÖY will act as the guarantor. All authors
approved the final version of manuscript.
Funding: Ondokuz Mayis University Scientific
Research Projects (PYO.TIP.1904.10.041).
Competing interest: None stated.
|
What This Study Adds?
Lactose and fructose intolerance
can cause chronic abdominal pain in children.
|
References
1. Saps M, Seshadri R, Sztainberg M, Schaffer G,
Marshall BM, Di Lorenzo C. A prospective school-based study of abdominal
pain and other common somatic complaints in children. J Pediatr.
2009;154:322-6.
2. Latulippe ME, Skoog SM. Fructose malabsorption and
intolerance: Effects of fructose with and without simultaneous glucose
ingestion. Crit Rev Food Sci Nutr. 2011;51:583-92
3. Gijsbers CF, Kneepkens CM, Büller HA. Lactose and
fructose malabsorption in children with recurrent abdominal pain:
Results of double-blinded testing. Acta Paediatr. 2012;101:411-5.
4. Tsampalieros A, Beauchamp J, Boland M, Mack DR.
Dietary fructose intolerance in children and adolescents. Arch Dis
Child. 2008;93:1078.
5. Gomara RE, Halata MS, Newman LJ, Bostwick HE,
Berezin SH, Cukaj L, et al. Fructose intolerance in children
presenting with abdominal pain. J Pediatr Gastroenterol
Nutr.2008;47:303-8.
6. Born P. Carbohydrate malabsorption in patients
with non-specific abdominal complaints. World J Gastroenterol.
2007;13:5687-91.
7. Huertas-Ceballos AA, Logan S, Bennett C, Macarthur
C. Dietary interventions for recurrent abdominal pain (RAP) and
irritable bowel syndrome (IBS) in childhood. Cochrane Database Syst Rev.
2009;1.
8. Apley J, Naish N. Recurrent abdominal pains: A
field survey of 1000 school children. Arch Dis Child. 1958;33:165-70.
9. Hoekstra JH, van Kempen AA, Bijl SB, Kneepkens CM.
Fructose breath hydrogen tests. Arch Dis Child. 1993;68:136-8.
10. Babu J, Kumar S, Babu P, Prasad JH, Ghoshal UC.
Frequency of lactose malabsorption among healthy southern and northern
Indian populations by genetic analysis and lactose hydrogen breath and
tolerance tests. Am J Clin Nutr. 2010;91:140-6.
11. Webster RB, DiPalma JA, Gremse DA. Lactose
maldigestion and recurrent abdominal pain in children. Dig Dis Sci.
1995;40:1506-10.
12. Wald A, Chandra R, Fisher SE, Gartner JC, Zitelli
B. Lactose malabsorption in recurrent abdominal pain of childhood. J
Pediatr. 1982;100:65-8.
13. Nucera G, Gabrielli M, Lupascu A, Lauritano EC,
Santoliquido A, Cremonini F, et al. Abnormal breath tests to
lactose, fructose and sorbitol in irritable bowel syndrome may be
explained by small intestinal bacterial overgrowth. Aliment Pharmacol
Ther. 2005;21:1391-5.
14. Kim JH, Sung IK. Current issues on irritable
bowel syndrome: Diet and irritable bowel syndrome. Korean J
Gastroenterol. 2014;64:142-7.
15. Rana SV, Malik A. Breath tests and irritable bowel syndrome.
World J Gastroenterol. 2014;20:7587-601.
|
|
|
 |
|

