|
|
|
Indian Pediatr 2020;57: 75 -76 |
 |
Pamidronate in Treatment of Calcinosis in Juvenile
Dermatomyositis
|
|
Shatabdi Giri 1,
Jyoti Ranjan Parida2,
Mrutunjay Dash1*
and Maitreyee Panda3
Departments of 1Paediatrics, 2Rheumatology,
and 3Skin and VD, IMS and SUM Hospital, Siksha ‘O’ Anusandhan
(Deemed to be University), Bhubaneswar, Odisha, India.
Email: [email protected]
|
|
Juvenile dermatomyositis is a rare
systemic autoimmune disease wth calcinosis as its hallmark sequelae. We
report three patients with juvenile dermatomyositis with calcinosis, who
were treated with pamidronate. There was complete clearance of
calcinosis in one child.
Keywords: Management, Sequalae.
|
|
Juvenile dermatomyositis (JDM) is an inflammatory disease of the muscle,
skin and blood vessels with peak age of onset 5-14 years and female:male
ratio 1.7:1 [1,2]. Calcinosis is a hallmark sequelae [3]. Pamidronate
has been used earlier for this indication [4] but there is lack of
reported experience in Indian set-up.
A 9-year-old boy presented to us with complaints of
fever, pain in all limbs and difficulty in walking for one and half
months. Child was initially treated with non-steroidal anti-inflammatory
agents (NSAIDS) after which pain had initially subsided to recur again.
On examination, there was peripheral myopathy, heliotrope rash and
Gottron papules. Laboratory investigations showed hemoglobin 7.7 g/dL,
elevated lactate dehydrogenase (399 U/L) and creatinine phosphokinase
(321 ug/L), and normal electromyogram. A muscle biopsy from Vastus
lateralis showed features of immune-mediated inflammatory myopathy.
Child was diagnosed as having JDM, and was started on steroids (20
mg/day), hydroxychloroquine (100 mg/day) and methotrexate (7.5 mg once a
week). The child improved over the next 3 years with good compliance and
regular follow-up, and gradually steroids were tapered to 5 mg/day. He
presented after fall from a bicycle with swelling of the little finger
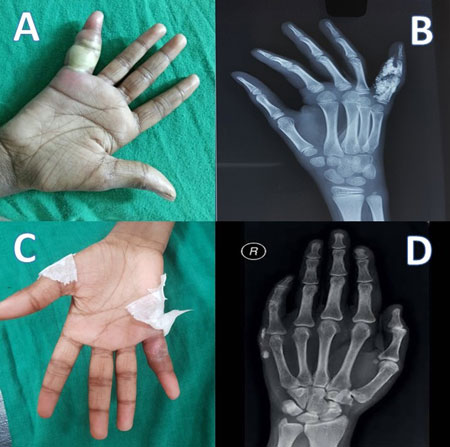
with chalky white discharge for 3 days (Fig. 1a). X-ray
revealed calcium deposits in soft tissue of little finger (Fig.
1b). Pamidronate was infused at 1 mg/kg/day for 3 consecutive days
every 3 months. On follow-up after one year, there was complete
clearance of calcinosis of fingers without any new focus and good
disease control without signs of myositis (Fig. 1c and
d).
 |
|
Fig. 1 (a) Calcinosis in the
little finger before treatment; (b) X-ray hand showing
calcinosis before treatment; (c) clinical resolution of
calcinosis after pamidronate; and (d) radiological resolution
after pamidronate
|
An 11-year-old girl presented with complaints of
swelling over right elbow and bilateral buttocks. She was diagnosed as
having JDM at 8 years of age. She was initially treated with steroids,
hydroxychloroquine and NSAIDS but had poor compliance to medicines.
Following a fall from the stairs, she started developing calcinosis of
buttocks followed by calcinosis of right elbow. There was presence of
heliotrope rash and Gower sign. X-ray showed calcium deposits on
affected areas. Child was started on 3-monthly pamidronate infusion
after which there was significant decrease in calcinosis with no fresh
foci. Complete resolution of disease process was not observed (Web
Fig. 1a), but the compliance to drugs was also not
optimal.
A 7-year-old girl presented with complaints of
multiple swellings over the body and difficulty in walking for one year.
The first swelling appeared in the waist region, followed by swellings
in bilateral chest walls and scalp (Web Fig. 2 a). The
swelling on the chest was excised by a local physician mistaking it to
be an abscess. Following this, the child developed more swellings in the
lateral chest near the site of excision (Web Fig. 2 b). On
examination, there were nodules on left anterior chest wall with scar
marks in bilateral infra-axillary area, Gottron papules and proximal
myopathy. Laboratory investigations showed anemia with raised LDH and
CPK. Hip X-Ray showed white nodular opacity around hip joint,
suggestive of calcinosis (Web Fig. 2 c and d).
Electromyogram showed membrane instability and fiber destruction. Child
was diagnosed as a case of JDM with calcinosis and was started on
steroids, hydro-xychloroquine, methotrexate, folic acid and 3-monthly
pamidronate infusion. Follow-up after 1 year showed significant decrease
in scalp swelling with complete disappearance of swelling over chest
wall and the waist region with no new calcinosis.
Calcinosis is a hallmark sequelae of JDM [1]. Alum,
alendronate, diltiazem and rituximab are few drugs used for treatment of
calcinosis [3]. Pamidronate is a nitrogen-containing bisphosphonate
which inhibits bone resorption used to treat osteoporosis [4]. Although
the mechanism of action of pamidronate is unclear, it was chosen based
on available adult studies [1,4,6]. A significant decrease in calcinosis
was found in two cases whereas there was complete clearance in one case.
Aggressive treatment with disease modifying anti-inflammatory agents
(DMARDs) early in the course of disease seem to be effective in good
disease control as was evident from case 1 and 3. Prompt diagnosis and
early intervention prevents further calcinosis. Our results suggest that
treatment with pamidronate infusion may achieve good disease control in
prevention of further calcinosis in JDM.
Acknowledgments: Prof. MR Nayak, Honorable
President, Siksha’O’ Anusandhan (Deemed to be) University and Mr
Somadatta Das, Central Research Laboratory, IMS & SUM Hospital for
technical support in submitting the manuscript.
Contributors: SG: collected data and
drafted the manuscript; JRP, MD and MP: diagnosed the case, and
planned the management. All authors approved the final version of
manuscript.
Funding: None; Competing interest: None
stated.
References
1. Rider LG, Miller FW. Deciphering the clinical
presentations, pathogenesis and treatment of the idiopathic inflammatory
myopathies. JAMA. 2011;305:183-90.
2. Bohan A, Peter JB. Polymyositis and
dermatomyositis. N Engl J Med. 1975;292:403-7.
3. Clara M, Ricardo Y, Luz C. Calcinosis as a
complication of juvenile dermatomyositis (JDM). Pediatr Rheumatol.
2011;9:P55.
4. Marco Puche A, Calvo Penades I, Lopez Montesinos
B. Effectiveness of the treatment with intravenous pamidronate in
calcinosis in juvenile dermatomyositis. Clin Exp Rheumatol.
2010;28:135-40.
5. Rauch F, Glorieux FH. Osteogenesis imperfect.
Lancet. 2004;24:1377-85.
6. Martillotti J, Moote D, Zemel L. Improvement of calcinosis using
pamidronate in a patient with juvenile dermatomyositis. Pediatr Radiol.
2014;44:115-8.
|
|
|
 |
|

