|
S.B. Grover,
K.A. Charan,
N.C. Saxena,
From the Department of Radiology and Imaging, Safdarjung Hospital. New Delhi 110 029. India.
Dr. Shabnam Bhandari Grover, E-81, Kalkaji, New Delhi 110 019. India.
Manuscript Received: June 29, 1998; Initial review completed: July 28, 1998;
Revision Accepted: September 22, 1998.
Frontonasal dysplasia was first described in the. mid nineteenth century(1). The anomaly consists of hypertelorism, broad nasal root and lack of nasal tip. Variable manifestations include anterior cranium bifidum occultum, widow's peak; midline clefting of nose and/or upper lip and notching or
coloboma: of the nostril. Lipomas of corpus callosum are traditionally considered as tumors of adults and their presence in children is infrequent(2). Frontonasal dysplasia
is itself a rare entity and its association with corpus callosum lipoma has only recently been recognized with the advent of sectional imaging. We describe a case of frontonasal dysplasia
with corpus callosum lipoma, who was initially being treated only for cleft lip and cleft palate.
Case Report
An 11-year-old male, presented with a history of headache and vomiting of
increasing frequency over the preceding six months. A
surgical repair of cleft lip, cleft palate and an absent right nasal ala had been performed in
early infancy. Presently the child was well oriented, without neurological
deficit. The fundus was normal. The child's face revealed a normal forhead and hairline, hypertelorism, a broad nasal root, deformed right nostril with surgical scars of a repaired cleft lip, cleft
palate and right nostril. The patient was an introvert with an IQ of 70. In view of the history of headache and vomiting of increasing frequency, investigative procedures were undertaken to rule out an intracranial space occupying lesion. Routine. investigations were normal.
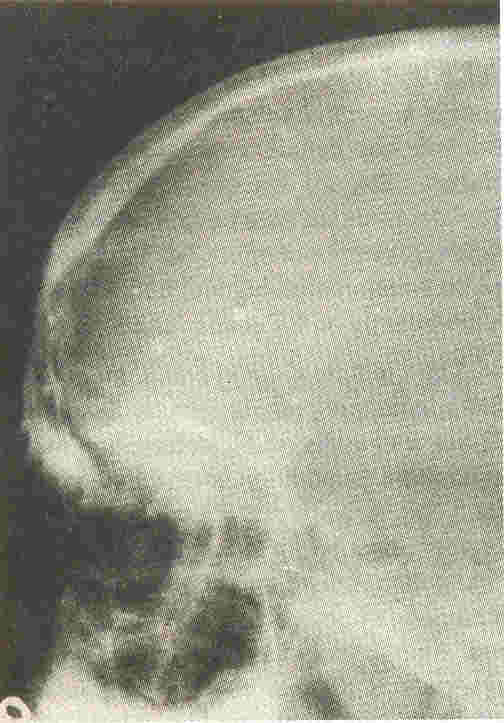
The lateral skull radiograph revealed widely separated nasal bones with an anterior frontal luscency (Fig. 1). No intracranial
calcification could be demonstrated. CT scan in axial plane revealed a non-enhancing hypodense midline tumor with. attenuation values of lipid, located in the anterior part of the corpus callosum (Fig. 2). Anterior cranium bifidum
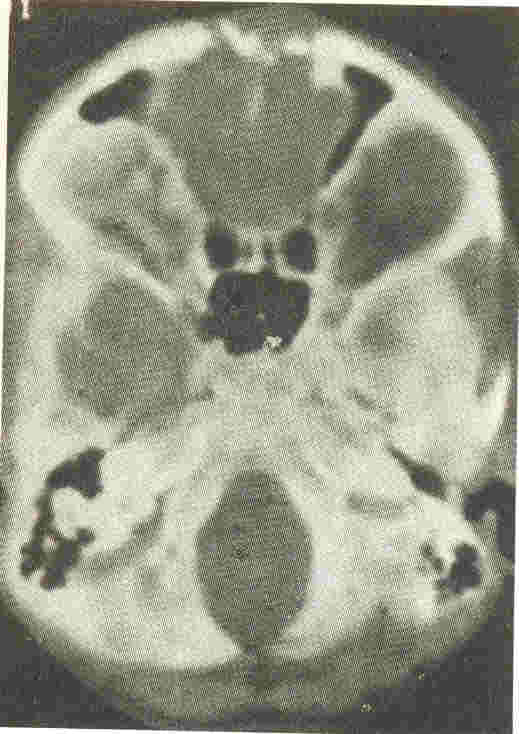
was documented on bone windows (Fig. 3) and corresponded to the lucent region seen on the lateral skull radiographs. The entire gamut of anomalies was consistent with a diagnosis of frontonasal dysplasia with bifid cranium and corpus callosum lipoma. In view of the pre-existing mental retardation and the multiple congenital facial anomalies, further surgical intervention for the intracranial lipoma was refused by the child's parents.
 |
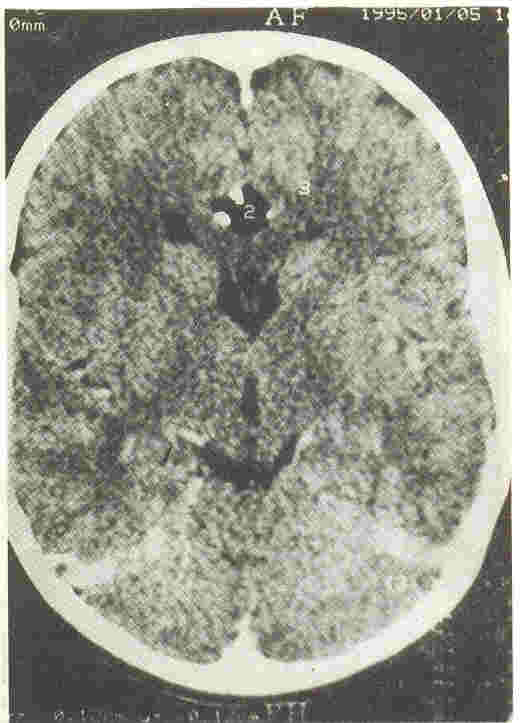 |
Fig. 1. Lateral skull radiograph shows anterior frontal
luscency and widely placed nasal bones.
|
Fig. 2. Axial CECT scan shows fat containing tumor in the
anterior part of corpus callosum, with peripheral calcification. |
 |
|
Fig. 3 Bone window view,
shows bone defect in frontial region indicating bifid cranium. |
Discussion
Frontonasal dysplasia (FND) is also known as Burian's syndrome or median cleft face syndrome(1). Although, first recognized in the mid nineteenth
century(1), it is a rare condition and only about 100 cases have been reported till 1996(1-3).
This dysmorphic syndrome is polygenetic
.
because it is sometimes inherited as a dominant and sometimes as a recessive trait(1). The parents of an affected child can expect the risk to be 25% for the next child(1).
The diagnosis of FND is possible by combined clinical and imaging approach. In a patient with hypertelorism, bifid nose, broad nasal root,
cleft lip and palate, this diagnosis should be considered and psychological. and
mental impairment must be excluded. The associated cranial and cerebral
anomalies characteristic of this condition can be documented only by imaging studies. Our patient fulfilled all the described clinical criteria along with psychological and mental impairment, and
also the cranial (bifid cranium) and cerebral (lipoma of corpus callosum) abnormalities.
Fig. 3. Bone window view, shows bone ,lefect in frontal region indicating bifid cranium.
Intracranial lipomas are classically considered as tumors of adults, however, the lipomas associated with FND are believed to be present from birth(2) and many of these children have an associated extracranial frontal lipoma as well(2). The presence of extracranial frontal lipoma
indicates excessive proliferation of fatty tissue; before closure of the anterior neuropore and entrance of part of this tissue into the prosencephalic
zone(2). The association of corpus callosum lipomas in FND is variable. In one series(3), all the patients were examined by CT scan, however only 4 patients out of 2] had an associated intracranial lipoma. In another series(2) however, all 8 patients had intracranial lipoma which were
documented by CT scan. An interesting feature regarding corpus callosum lipomas associated with FND is that these tumors are always anteriorly situated and cause minimal neurological deficit, in contradistinction to corpus callosum lipomas without FND(2). The diagnostic hallmark of shell-shaped calcification at tumor margins, has been described on conventional roentgenograms(2), but was revealed only on CT scan in our patient.
The important differential diagnosis of FND includes frontofacionasal dysplasia or FFND which has ocular defects and midface hypoplasia in addition to the midline facial cleft(4,5). Acro-frontofacionasal dysostosis is another disorder of the FND development field which is distinguished from FND by the presence of camptobrachy-polysyndactyly
and limb hypoplasia(6). Craniofrontonasal dysplasia is another entity which is distinguished from frontonasal dysplasia by the presence of coronal synostosis(7), as opposed' to a bifid cranium which is seen in FND. Clinically these patients of craniofrontonasal dysplasia are observed to have characteristic dry, curly or fuzzy hair(7).
The treatment of the median cleft face syndrome has been described by De Myer(8), based on a classification of the type of faces and mental status. In view of the high risk (25%) of a similar craniofacial anomaly occurring in the next sibling(1), genetic counselling of the parents is an important part of the management strategies. We have described the characteristic clinical, genetic and imaging features of frontonasal dysplasia and also discussed its related differential diagnosis: In a child with cleft lip and palate, the possibility of median cleft face syndromes should be kept in mind; the clinical examination and imaging evaluation must be aimed at excluding the known associated cranial and cerebral abnormalities. Following the complete clinical and
imaging evaluation, relevant genetic counseling and appropriate treatment should be instituted at the earliest.
|
|
1. Fox JW, Golden GT, Edgerton MT. Frontonasal dysplasia with alar
clefts in two sisters. Genetic considerations and surgical correction. Plast
Reconstr Surg 1976; 57: 553- 561.
2. Castroviego IP, Pascual-Pascual SI, Higueras AP. Frontonasa] dysplasia and
lipoma of the corpus callosum. Eur J Pediatr 1985; 144: 66- 71.
3. Almeida MLG, Costa AR, Saavedra 0, Cohen Jr MM. Frontonasal dysplasia:
Ana]ysis of 21 cases and literature review. lnt J Oral Maxillofac
Surg 1996; 25: 91-97.
4. Gollop TR, Kiota MM, Martins RMM, Lucchesi EA, Alvarenga E. Frontofacio nasal
dysplasia: Evidence for autosomal recessive inheritence. Am J Med Genet
1984; 19: 301- 305.
5. Gollop TR. Fronto-Facio-Nasal dysostosis-A new autosomal syndrome. Am J Med
Genet 1981; 10: 409-412.
6. White EW, Figueroa R, Flannery DB. Brief clinical report-frontofacionasal
dysplasia. Am J Med Genet 1991; 40: 338-340.
7. Orr OJ, Slaney S, Ashworth GJ, Poole MD. Cranio frontonasal,
dysplasia, Br J Plast Surg 1997; 50: 153-161.
8. De Myer W. The median cleft face syndrome. Differential diagnosis of cranium
bifidum occultum, hypertelorism and median cleft nose, lip and palate. Neurology
1967; 17: 961- 971.
|
