The term 'Pulmonary Hemosiderosis' is
used to describe a number of rare conditions characterized by an abnormal accumulation of hemosiderin in the lungs. Pulmonary hemosiderosis
may occur as a primary phenomenon, most commonly in children or
secondary to cardiac, systemic vascular' or hemorrhagic diseases(1). The secondary form is seen more frequently in adults, There are four types of primary pulmonary hemosiderosis, an idiopathic form, a form associated with cow's milk hypersensitivity (Heiner Syn- drome)(2), a form occurring in association with myocarditis and a form associated with progressive glomerulonephritis (Goodpasture's Syndrome). We report 2 cases of Idiopathic Primary Pulmonary Hemosiderosis, a rare entity in children. Our 12 year search of the Indian literature revealed an isolated case report(3).
Case
Reports
Case 1: A 1-year-9-month-old female child presented to us with recurrent episodes of fever, cough and hurried respiration since the age of 8 months and the latest episode commence 10 days prior to admission. On 3 occasions at the ages of 10, 13 and 21 months, the child was found to have significant anemia that required blood transfusion. On the last occasion the child tested positive for malaria and was treated with antimalarials. The child was fed exclusively with breast milk till the age of 4 months and then weaning was started with formula milk. There was no history of chronic rhinitis, ear discharge, hematemesis or contact with tuberculosis.
On examination the child was in respiratory distress. The respiratory rate was 70/min, pulse 160/min and temperature was normal. There was significant pallor and clubbing was present. Systemic examination revealed evidence of congestive cardiac failure. Our clinical impression was idiopathic pulmonary hemosiderosis.
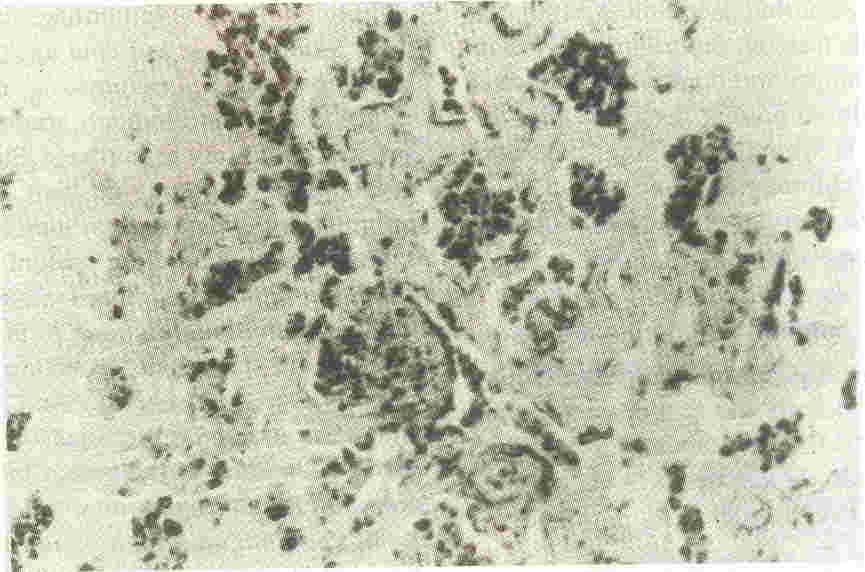
The laboratory investigations are summarized in Table I. The lung biopsy (Fig.
1) con- firmed our diagnosis. The child was managed with supportive measures and
steroids: The child's condition improved steadily after starting steroids and she was discharged 2 weeks after initiating steroid therapy. At present 15 months after discharge, the child is on maintenance
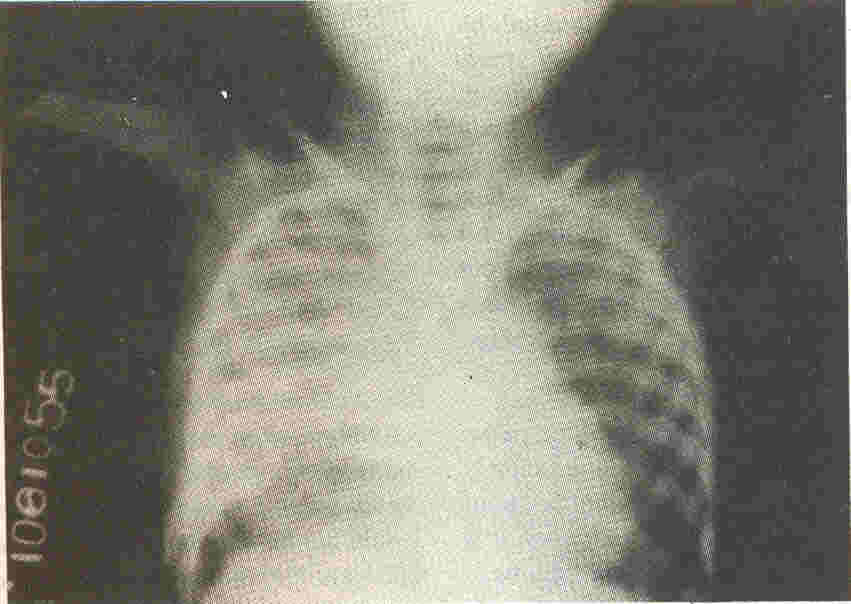
steroid and she has improved symptomatically. Her cough has subsided, tachypnea has decreased and she has not required further' blood transfusions. However, the chest X-ray
(Fig. 2)
shows no significant improvement
and mild hypoxia on ABG is persistent.
 |
|
Fig 1.
Histophathological picture of lung parenchyma (prussian blue
stain) showing alveoli containing hemosiderin laden macrophages |
 |
|
Fig. 2. Chest
X-ray showing bilateral interstitial infiltrates |
Case 2: A 2-year-8-month-old female
child presented to us with fever of one month duration, rapid breathing and
progressive pallor associated with abdominal pain of I week duration. On admission the child was in respiratory distress and markedly pale. The respiratory rate was 82/min, pulse was 160/min and BP was
110/70 mm Hg. Systemic examination revealed evidence of congestive cardiac failure.
The child's respiratory distress persisted despite 4 weeks of treatment with antibiotics,
decongestive measures, packed cell transfusions and other supportive measures. ABG showed persistent hypoxia on 5 liters of oxygen. She remained oxygen dependent and ,the repeat chest X-rays showed persistent infiltrates, She also developed mild clubbing during this period. Our investigations directed at detecting toe cause of anemia revealed 'a microcytic hypochromic blood picture' with depleted iron stores (Table I). A diagnostic lung biopsy to confirm our impression of Idiopathic Pulmonary Hemosiderosis was
considered at this stage but was not done, as the parents were not willing to subject the child to an invasive procedure.
The child was started on steroids and her condition gradually improved over 2 weeks. Her tachypnea decreased and we were able to
stop supplementary oxygen. The child was discharged. She was put on maintenance steroids and was symptom free for 15 months. She was then readmitted for a superadded pneumonia requiring mechanical ventilation and antibiotic therapy. On readmission a diagnostic lung biopsy was done which confirmed our diagnosis. At present, 3 months after discharge, she is symptom free on maintenance steroid and chloroquine. However, chest X- ray shows no improvement and mild hypoxia on ABG is persistent.
Discussion
The clinical picture of Idiopathic Pulmonary Hemosiderosis was first documented by Ceelen
in 1931 (4). We attempt to highlight" the salient features and trends in the
management of this rare disorder.
The majority of patients with primary pulmonary hemosiderosis have the isolated or idiopathic form. The disease occurs most frequently in the first decade of life. Cases are distributed equally among males and females. Clinically the process is characterized by acute or insidious onset of pulmonary symptoms including cough, hemoptysis, wheezing, cyanosis and dyspnea. Hematemesis may occur as a result of swallowed pulmonary blood. Other common features include pallor, poor weight gain and fatigue. The long term course is usually characterized by recurrent episodes of pulmonary hemorrhage" with associated fever and tachypnea. Digital clubbing is often present.
Both our cases presented with fever, pallor and hurried respiration. Other features namely hematemesis, hemoptysis, wheezing and poor weight gain were not present. However, it is well known that, any of the clinical features of the disease may be it's first manifestation(5) and hemoptysis may never occur.
Laboratory findings at presentation typically include a microcytic hypochromic anemia and the serum iron is low. Most patients demonstrate a reticulocytosis during periods of acute pulmonary hemorrhage. A positive direct Coomb's test and cold agglutinins are sometimes noted. Leukocytosis
and an elevated ESR not uncommonly accompany episodes of pulmonary hemorrhage. Stool guaiac evaluation is frequently positive. Iron laden macrophages (siderophages)
may be demonstrated in specimens from sputum or gastric washings which have been stained using the Prussian Blue reaction. A more direct approach is fibre optic bronchoscopy with bronchoalveolar lavage(6). Anti basement antibodies may be present in 90% of those with Goodpasture's syndrome. Children with
cow's milk sensitivity may
have
elevated
levels of serum antibodies to constituents of cow's milk or positive intradermal skin tests to cow's milk proteins.
A variety of radiographic findings have been described(4). The findings may be mistaken for pulmonary edema. In others it may resemble miliary tuberculosis.
A microcytic hypochromic anemia with reticulocytosis, bilateral interstitial infiltrates on chest X-ray and serial ABGs showing persistent hypoxia were features seen in both our cases. However, gastric aspirates did not reveal siderophages in both cases. We investigated both our cases for known causes of hemosiderosis, but all the tests were negative.
Antibasement membrane, antinuclear (ANA) antineutrophil cytoplasmic. (ANCA)
antibodies and cold agglutinins could not be detected. LE cells and rheumatoid
factor could not be detected either. Results of urine analysis, levels of serum
complement components, blood urea and serum creatinine were all normal. Our
evaluation included intradermal
skin tests for milk protein allergy
which were negative.
Lung biopsy is justified in infants or young children in whom clinical findings
are atypical or if diagnosis is still in doubt after all simpler procedures have
been done. The characteristic pathologic findings include interstitial fibrosis, numerous iron laden macrophages in the alveoli and interstitium often with increased number of mast cells(7).
The treatment of pulmonary hemosiderosis is largely supportive. Patients with acute crisis may require oxygen, mechanical ventilation and blood transfusions.
ACTH (10-25 units/day) or methylpred-nisolone 1 mg/kg (6 hourly) by intravenous infusion is recommended for the first 24-48 hours. Oral prednisolone or methylprednisolone may then be given. The corticosteroid may be tapered as clinical improvement occurs but should be restarted or increased if any signs of recurrent pulmonary hemorrhage develop( 4).
A second immunosuppressant drug may be considered in some patients with persistent symptoms or high corticosteroid requirement. Azathioprine(8),Chloroquine(9) and cyclophosphamide(10) have been used and may permit lowering the corticosteroid dose. Plasmapheresis and plasma exchange have also been used(11).
Other measures that have been employed are the use of desferrioxamine and a hypo allergenic diet(4). The tendency for spontaneous remissions and exacerbations in this disorder create considerable difficulty in evaluating any form of therapy. Soergel and Sommers in their review concluded that steroids were probably worthwhile in stemming acute bleeding episodes, but that long term therapy did not alter the course or prognosis of the disease(7). There are reports of children
being only mildly symptomatic and trans- fusion independent for three years on chloroquine therapy(9).
Approximately one half of the patients die within 1-5 years usually from acute pulmonary hemorrhage and progressive respiratory failure. The average duration of life in those dying from the disease is about two and a half years after the onset of symptoms(7).
In conclusion, Idiopathic Pulmonary Hemosiderosis is a rare disease in children, which poses many diagnostic problems and often requires prolonged therapy with immunosuppressant drugs.
