xillary thermometry is a
non-invasive method for temperature measurement in sick febrile infants
but may disturb the sleep of the infants and may contribute to
infections by frequent direct contact. Non-contact infrared thermometry
(NCIT) avoids these risks preserving the clinical accuracy of
conventional methods [1-3]. It is a rapid non-invasive method for
temperature measurement in febrile infants; however, with discordant
results reported earlier [3,4]. The objective of this study was to study
the agreement between NCIT and mercury-in-glass thermometer.
This was a cross-sectional study conducted in the
pediatric department of a tertiary healthcare facility after approval
from institute research and ethics committee. Written informed consent
was obtained from the parents/legal representative. Infants from 1st day
of life to 12 mo of age attending the pediatric outpatient department
between 1st September to 31st October, 2018 were included in the study
population. Sick and unstable infants were excluded. Axillary
temperature was measured using mercury-in-glass thermometer (Enbee; Wuxi
Moxibei Clinical Thermometer Co. Ltd.) after the axilla was wiped with a
dry towel. The thermometer probe tip was placed under the axilla so that
the tip was touching the skin and the temperature was measured after 5
min. Forehead temperature was recorded for NCIT with infrared
thermometer Equinox EQ-IF-02 (Equinox Meditech Private Limited, New
Delhi). Accuracy Range-10°C to 40°C) at approximately 0.5-1 cm distance
from the glabella [5]. Measurements were taken by a trained nurse and
the duty doctor from both the devices within 6 minutes.
The degree of agreement between the two methods was
studied using the Bland and Altman method and the mean difference with
95% confidence limits noted for clinical consideration. SPSS 18.0
software was used to analyze the results.
 |
|
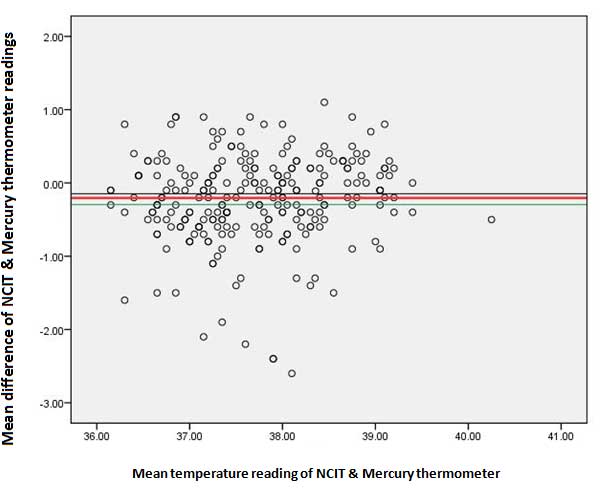
Fig. 1 Bland altman plot showing the
comparison of now-contact infrared thermometer (NCIT) and
mercury thermometer readings.
|
Among 250 infants approached for the study, 7 (2.8%)
were aged less than 28 days and 243 (97.2%) were aged from one month to
one year. The mean (SD) infrared thermometer and temperature recordings
of mercury-in-glass thermometer were 37.6 (0.91)°C and 37.6
(2.49) °C, respectively; mean difference -0.016 (95% CI: -0.32,
0.29). There was a significant correlation between NCIT and axillary
thermometry measurements (r=0.22; P<0.001). Number of observed
agreement was for 80.8% of observations, indicating moderate agreement
(kappa=0.602) between both instruments (Fig. 1).
The mean (SD) temperature recordings of infrared
thermometer and mercury-in-glass thermometer were 37.6 (0.91)°C and 37.6
(2.49)°C, respectively; mean difference. The present study established a
good correlation between NCIT and axillary thermometry. Few earlier
studies revealed conflicting results about the validity and accuracy of
NCIT [4,6]. However, other studies have proven the clinical accuracy of
NCIT compared to digital axillary thermometry [7-9]. The accuracy and
reproducibility of NCIT in different body sites in comparison to
conventional thermometers was demonstrated by Osio, et al. [8].
Digital thermometer is safer but its clinical accuracy is considered
inferior to mercury-in-glass thermometer. Thus, we compared the clinical
accuracy of NCIT with that of mercury-in-glass thermometer as also
conducted by Chiappini, et al. [10] who reported significant
correlation between the two methods (P<0·0001), similar to our
study.
In our study, moderate agreement between NCIT and
mercury thermometry reading was demonstrated. The cost effectiveness of
NCIT in resource poor settings needs to be determined. Further studies
comparing NCIT with rectal thermometry which is the gold standard would
support the use of NCIT in clinical settings.
Contributors: ST,RB: collected data and managed
the patients; ST reviewed the literature and drafted the initial version
of the manuscript; SP: contributed to literature review and critically
revised the manuscript. All authors approved the final version of the
manuscript.
Funding: None; Competing interest: None
stated.
1. Sollai S, Dani C, Berti E, Fancelli C, Galli L,
Martino M, et al. Performance of a non-contact infrared
thermometer in healthy newborns. BMJ Open. 2016:6;1-5.
2. El-Radhi AS. Determining fever in children: The
search for an ideal thermometer. Br J Nurs. 2014; 23:91-4.
3. Smith J. Are electronic thermometry techniques
suitable alternatives to traditional mercury in glass thermometry
techniques in the pediatric setting? J Adv Nurs. 1998; 28: 1030-9.
4. Atas Berksoy E, Bag Ö, Yazici S, Çelik T. Use of
noncontact infrared thermography to measure temperature in children in a
triage room. Medicine (Baltimore). 2018; 97: 9737.
5. Robertson-Smith J, McCaffrey FT, Sayers R,
Williams S, Taylor BJ. A comparison of mid-forehead and axillary
temperatures in newborn intensive care. J Perinatol. 2015; 35:120-2.
6. Sethi A, Patel D, Nimbalkar A, Phatak A, Nimbalkar
S. Comparison of forehead infrared thermometry with axillary digital
thermometry in neonates. Indian Pediatr. 2013; 50:1153-4.
7. Wang K, Gill P, Wolstenholme J, Price CP, Heneghan
C, Thomson M, et al. Non-contact infrared thermometers for
measuring temperature in children: Primary care diagnostic technology
update. Br J Gen Pract. 2014; 64: 681-3.
8. Osio CE, Carnelli V. Comparative study of body
temperature measured with a non-contact infrared thermometer versus
conventional devices. The first Italian study on 90 pediatric patients.
Minerva Pediatr. 2007;59: 327-36.
9. Uslu S, Ozdemir H, Bulbul A, Comert S, Bolat F,
Can E, et al. A comparison of different methods of temperature
measurements in sick newborns. J Trop Pediatr. 2011; 57: 418-23.
10. Chiappini E, Sollai S, Longhi R, Morandini L, Laghi A, Osio CE.
Performance of non-contact infrared thermometer for detecting febrile
children in hospital and ambulatory settings. J Clin Nurs. 2011; 20:
1311-8.

