|
|
|
Indian Pediatr 2019;56: 749-752 |
 |
Improvement in Successful Extubation in
Newborns After a Protocol-driven Approach: A Quality Improvement
Initiative
|
|
Rameshwar Prasad
and Asit Kumar Mishra
From Department of Pediatrics, Tata Main Hospital,
Jamshedpur, Jharkhand, India
Correspondence to: Dr Rameshwar Prasad, Flat no 3,
Crystal Villa, Kadma Jamshedpur 831 005, Jharkhand, India.
Email:
[email protected]
Received: June 22, 2018;
Initial review: December 03, 2018;
Accepted: June 11, 2019.
|
|
Objective: To reduce extubation
failure rate by implementing protocol-driven ventilation and extubation
strategies. Methods: Quality improvement project in a level II
neonatal care unit from April 2017 to January 2018. Ventilation and
extubation protocols implemented from 1 August, 2017. 18 ventilated
newborns in the pre-protocol period, 16 in Plan-do-check-act (PDCA)
cycle I and 17 in PDCA cycle II. Primary outcome was
extubation failure within the first 72 h of extubation. Results:
Extubation failure rate reduced from 41.7% (pre-protocol period) to
23.8% (PDCA 1 and 2, OR 0.44, 95% CI 0.12 to 1.59, P = 0.21).
Median time to first extubation attempt significantly decreased (71.5 h
to 38 h, P=0.046). Conclusions: A protocolized approach
through quality improvement initiative demonstrated a sustained
improvement in successful extubation with a significant reduction in the
median time to first extubation attempt in ventilated newborns.
Keywords: Extubation failure, Neonate, Quality
improvement, Ventilation.
|
|
E
arly successful extubation of ventilated newborns
is an important way to reduce ventilator-induced lung injury, sepsis and
length of stay. Evidence-based strategies improve successful extubation
rate [1,2]. Nonetheless, the inconsistent practices and arbitrary
approach to ventilation and extubation result in repeated extubation
failures and consequential reintubation [3,4]. An average of 25%
ventilated newborns fail extubation [5,6]. Extremely preterm newborns
have a much higher risk of failed extubation [7]. The evidence of
protocol-driven management approach in reducing the duration of
mechanical ventilation and weaning time is limited in newborns [8]. This
study was designed to assess the impact of quality improvement on
extubation failure in neonates.
Methods
The study was conducted in a level II neonatal care
unit in an industrial hospital in India between 1
April, 2017 and 31
January, 2018. The study had 3 periods – Baseline (1
April, 2017 – 30 June, 2017), Plan-Do-Check-Act (PDCA) cycle I (1
August, 2017 – 31
October, 2017) and PDCA cycle II (1
November, 2017 – 31
January, 2018). Our primary outcome was extubation
failure which was defined as reintubation within 72 hours of extubation
irrespective of the cause [6]. Reintubation was defined as intubation
occurring after 72 hours of extubation and was excluded from extubation
failure. During the baseline period, patient data were collected by
reviewing patients’ charts and electronic database. We constituted a
team comprising a consultant-in-charge of the neonatal unit,
specialists, a neonatologist and two senior nursing staff. In a
brainstorming session, the probable causes of extubation failure were
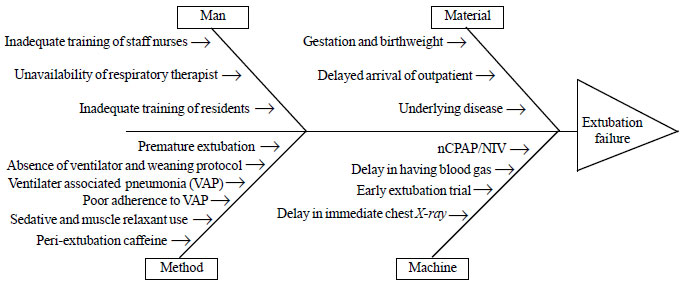
identified and put into a fish-bone diagram (Fig. 1). Most
of the modifiable root causes of extubation failure belonged to man and
method groups. Further, why-why analysis led us to the two main problems
of lack of standardized ventilation and extubation strategies.
 |
|
Fig. 1 Cause and effect diagram.
|
We addressed the above two problems by drafting
ventilation and extubation strategies by searching the literature for
evidence-based practices. We prepared a checklist for extubation
readiness. Printed copies of ventilator strategy, ventilator-associated
pneumonia (VAP) prevention bundle and checklist for extubation readiness
were displayed at the bedside. Training was given to residents,
pediatricians and staff nurses twice a month about the protocol and
records maintained. The consultant-in-charge of the neonatal unit
crosschecked the extubation checklists before taking a decision to
extubate a newborn. Post-extubation adrenaline nebuli-zation was given
regularly although its evidence is lacking in newborns. We did not
include peri-extubation dexamethasone in the protocol due to concerns
over both short and long term complications.
The protocols were implemented from 1
August, 2017. Ethical approval was not sought as
this was a quality improvement initiative. Our primary objective was to
reduce extubation failure rate by 25% from baseline. Secondary outcomes
to assess the impact of intervention were: time of first extubation
attempt, multiple extubation failures (defines as two or more extubation
failures in a newborn during hospital stay) and duration of mechanical
ventilation. During the first PDCA cycle, patient data for all baseline
and outcome variables were collected.
During PDCA cycle II, we uploaded the protocol in the
hospital’s digital document control system. Nursing staff and residents
were given training monthly and ventilator and weaning strategies were
discussed with them during daily rounds.
The study included all consecutively ventilated
newborns during the study period. Newborns who died, discharged
against medical advice (DAMA) or those referred to higher center before
attempting first extubation were excluded from analysis.
Statistical analyses: SPSS 15 was used to analyze
data. Data were examined for normality by Kolmogorov-Smirnov and
Shapiro-Wilk tests. We used the chi-square test and Fischer’s exact test
for categorical variables. Independent t-test and Mann Whitney U test
were used for continuous variables, as appropriate. A P value of
<0.05 was considered statistically significant and all tests were
2-tailed. The data were analyzed on an intention-to-treat basis.
Results
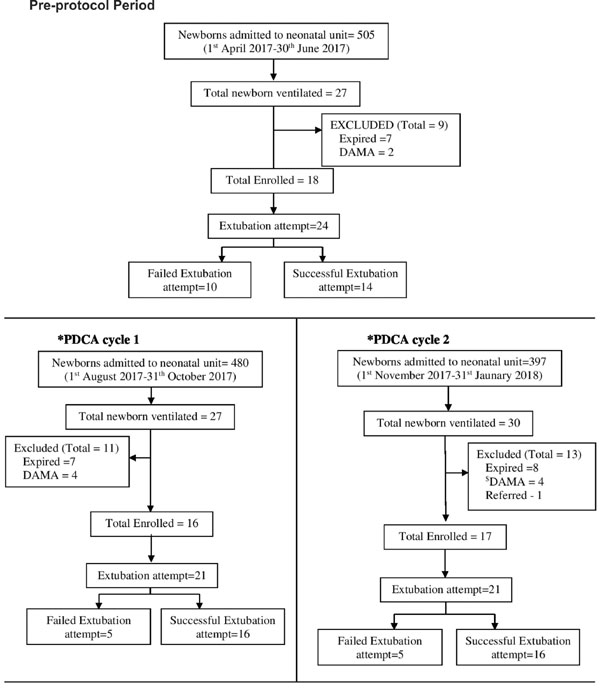
Study flow is depicted in Fig. 2. The
demographic characteristics were similar in all three groups. In
baseline period, PDCA-1 and PDCA-2, mean (SD) birth weight was 2168
(1008), 2176 (861.4), and 2226 (651) g, and mean (SD) gestational age
was 34.6 (3.4), 34.2 (4.6) and 35.0 (3.7) wk, respectively. In the three
groups, males were 67%, 75% and 76% and inborn newborns were 61%, 42%
and 53%, respectively. Table I provide the details of
outcomes in the three groups. There was a significant reduction in time
to first extubation attempt.
 |
|
Fig. 2 Participant recruitment
flow diagram.
|
TABLE I Clinical Outcomes in Neonataes Before and After a Quality-improvement Intervention (N=17)
|
Outcome |
Pre-protocol period (n=18) |
PDCA-1 (n=16) |
PDCA-2 (n=17) |
|
Extubation failure rate* |
10/24 (41.7%) |
5/21 (23.8%) |
5/21(23.8%) |
|
Extubation failure ≥2#
n/N (%) |
4/18 (22.2%) |
1/16 (6%) |
0/17 |
|
Time (h) of first extubation attempt, median (IQR) |
71.5 (46.5-75) |
51 (16.6-92.4) |
38$ (21.5-83) |
|
Duration (h) of mechanical ventilation, median (IQR) |
73.5 (70.5-139.3) |
68.5 (18.8-96.3) |
49 (22.0-112.5) |
|
*PDCA: plan-do-check-act cycle; *Number of re-intubations
within 72 h of extubation ÷ total number of extubation attempts
(%); #Number of newborns needed
≥2 reintubations within 72 h of extubation÷ total number
of newborns in that period (%); $P= 0.046
(pre-protocol vs PDCA-2). |
Compliance to caffeine use, pre-extubation chest X-ray,
target minimal ventilator settings, withholding enteral feed, inotropes
and sedation according to extubation checklist was 100% in both
post-protocol periods 1 and 2. Compliance to pre-extubation blood gas
analysis was 33.3%. All newborns were ventilated on either
Synchronized intermittent mandatory ventilation – pressure support or
Assist control mode.
Discussion
In the present study, quality improvement PDCA cycles
resulted in significant reduction in extubation failure rate. It also
resulted in time to first extubation attempt.
The major constraint of this study is small sample
size from a single center that limits generalizability and precludes
subgroup analysis. The study group is heterogeneous in gestational age,
birth weight and morbidities that can introduce selection bias.
Prolonged mechanical ventilation in very preterm newborns could
potentially confound the results. Out-born newborns coming late to our
hospital preclude early surfactant therapy and/or early ventilator
support. Our study did not measure other important outcomes e.g.
retinopathy of prematurity, bronchopulmonary dysplasia and neuro-developmental
outcomes.
Extubation failure is multifactorial and a single
intervention may not bring down its incidence. The extubation failure
rate varies widely among centers depending on the characteristics of
patients and the mode of support used after extubation. The definition
of extubation failure varies widely in literature from 24 hours to 7
days after extubation [6,9]. Two randomized controlled trials comprising
a small subgroup of term newborns evaluating weaning protocol were
inconclusive [8,10,11]. Hermato, et al. [12] demonstrated a
significant reduction in extubation failure rate, the median age of
first extubation attempt and the median duration of mechanical
ventilation in newborns (birth weight
³1250 g) after
implementing respiratory therapist-driven ventilation protocol in a
retrospective study. These were similar to results of the present study.
Our findings underscore the importance of using
quality improvement methodology [13,14] in settings where failed
extubation is a common troublesome phenomenon. The ventilation and
extubation protocols can be further updated according to available
resources at the local level as well as the current best scientific
knowledge. Studies are needed to study the impact of this approach on
other morbidities.
Acknowledgements: Dr Sudhir Mishra, Head,
Department of Pediatrics, Tata Main Hospital for his valuable inputs in
revising the manuscript. Air Marshal (Dr) Rajan Chaudhry, AVSM, VSM (Retd.),
GM (Medical Services), Tata Main Hospital, for providing permission
to submit the manuscript for publication. Contributors:
RP: planning, collection and analyses of data, literature review and
preparation of final manuscript; AKM: concept and design of the study,
review and revision of manuscript, final approval of manuscript. Both
authors approved the final version of manuscript, and are accountable
for all aspects related to the study.
Funding: None; Competing Interest: None
stated.
|
What This Study Adds?
•
A ventilation and extubation strategy, implemented using the
quality PDCA methodology, has the potential to reduce extubation
failure and time to first extubation attempt in ventilated
newborns.
|
References
1. Lemyre B, Davis Pg, De Paoli Ag, Kirpalani H.
Nasal intermittent positive pressure ventilation (nippv) versus nasal
continuous positive airway pressure (ncpap) for preterm neonates after
extubation. Cochrane Database Syst Rev. 2017;2:CD003212,
2. Ferguson KN, Roberts CT, Manley BJ, Davis PG.
Interventions to improve rates of successful extubation in preterm
infants: A systematic review and meta-analysis. JAMA Pediatr.
2017;171:165-74.
3. Al-Mandari H, Shalish W, Dempsey E, Keszler M,
Davis PG, Sant’anna G. International survey on periextubation practices
in extremely preterm infants. Arch Dis Child - Fetal Neonatal Ed.
2015;100:F428.
4. Shalish W, Anna GMS. The use of mechanical
ventilation protocols in canadian neonatal intensive care units.
Paediatr Child Health. 2015;20:e13-9.
5. Hiremath GM, Mukhopadhyay K, Narang A. Clinical
risk factors associated with extubation failure in ventilated neonates.
Indian Pediatr. 2009;46:887-90.
6. Giaccone A, Jensen E, Davis P, Schmidt B.
Definitions of extubation success in very premature infants: A
systematic review. Arch Dis Child Fetal Neonatal Ed. 2014;99:f124-7.
7. Hermeto F, Martins BMR, Ramos JRM, Bhering CA,
Sant’anna GM. Incidence and main risk factors associated with extubation
failure in newborns with birth weight < 1,250 g. J Pediatr (Rio J).
2009;85:397-402.
8. Wielenga JM, van den Hoogen A, van Zanten HA,
Helder O, Bol B, Blackwood B. Protocolized versus non protocolized
weaning for reducing the duration of invasive mechanical ventilation in
newborn infants. Cochrane Database Syst Rev. 2016;3:cd011106.
9. Wang S-H, Liou J-Y, Chen C-Y, Chou H-C, Hsieh W-S,
Tsao P-N. Risk factors for extubation failure in extremely low birth
weight infants. Pediatr Neonatol. 2017;58: 145-50.
10. Schultz TR, Lin RJ, Watzman HM, Durning SM, Hales
R, Woodson A, et al. Weaning children from mechanical
ventilation: A prospective randomized trial of protocol-directed versus
physician-directed weaning. Respir Care. 2001;46: 772-82.
11. G Randolph A, Wypij D, Venkataraman S, H Hanson
J, Gedeit R, L Meert K, et al. Effect of mechanical ventilator
weaning protocols on respiratory outcomes in infants and children: A
randomized controlled trial. JAMA. 2002; 288:2561-8.
12. Hermeto F, Bottino MN, Vaillancourt K, Sant’anna
GM. Implementation of a respiratory therapist-driven protocol for
neonatal ventilation: Impact on the premature population. Pediatrics.
2009;123:e907-16.
13. Chawla D, Darlow BA. Development of quality
measures in perinatal care – Priorities for developing countries. Indian
Pediatr. 2018;9:797-802.
14. Mehta R, Sharma KA. Use of learning platforms for quality
improvement. Indian Pediatr. 2018;9:803-8.
|
|
|
 |
|

