|
|
|
Indian Pediatr 2019;56: 745-748 |
 |
Effect of a Formative Objective Structured
Clinical Examination on the Clinical Performance of
Undergraduate Medical Students in a Summative Examination: A
Randomized Controlled Trial
|
|
Nazdar Ezzaddin Alkhateeb 1,
Ali Al-Dabbagh2,
Mohammed Ibrahim3
and Namir Ghanim Al-Tawil4
From Departments of 1Pediatrics, 2Surgery,
4Community Medicine, College of Medicine, Hawler Medicine
University, Erbil, Kurdistan region, Iraq; and 3Clinical
Training, Queensland Health Service, Australia.
Correspondence to: Dr Nazdar Ezzaddin Alkhateeb,
Department of Pediatrics, College of Medicine, Hawler Medical
University, Erbil, Kurdistan region, Iraq.
Email:
[email protected]
Received: February 11, 2019;
Initial review: April 29, 2019;
Accepted: July 13, 2019.
|
|
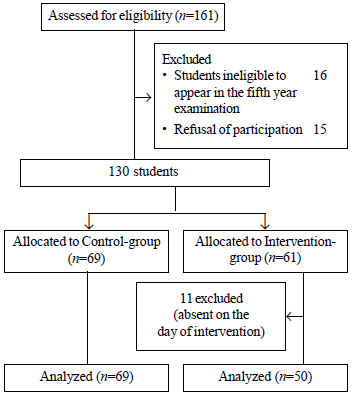
Objective: To study the effect of
formative Objective structured clinical examination (OSCE) on the
undergraduate medical students’ performance in a subsequent
summative-OSCE assessment. Methods: In a randomized single-blind
trial, 130 fifth year medical students at Raparin hospital, Erbil were
assigned to intervention (n=61) and control group (n=69).
Formative-OSCE was performed for the intervention group in pediatric
module with feedback on their performance versus standard
pediatric module for the control group. Students’ clinical performance
was assessed by a summative-OSCE. Multiple regression was used to
predict the summative-OSCE score depending on the participation in
formative-OSCE along with the other factors. Results: Eleven
students were excluded because of early drop-out, leaving 119 students
for analysis. The summative-OSCE mean score (out of a total score of
100) in intervention group 64.6 (10.91) was significantly lower as
compared to the control group 69.2 (10.45). Conclusion: Single
formative-OSCE does not necessarily lead to better performance in
subsequent summative-OSCE.
Keywords: Assessment, Clinical
competence, Educational measurement, Medical Eduation.
Trial Registration: Clinical trial.gov/NCT 035
99232.
|
|
A
ssessment is the cornerstone of any educational
project. It gives evidence about the success in the achievement of
specific learning outcomes [1,2]. Depending on the time and the intent,
assessment can serve three functions: diagnostic, a function for
prevention of learning difficulties; formative, a function for
regulating learning with delivery of feedback; and summative, a function
for certificate or social recognition [3].
As the assessment role shifts from a pure assessment
of learning to assessment for learning, there is an incentive to
determine how and when assessment of different forms have educational
value [4]. Unlike other
professional training culture, true feedback culture is not cultivated
in medical education. Therefore, a formative assessment must be at the
core of student training, not just included to fulfill accreditation
requirement [5].
In a performance-based assessment, the Objective
Structured Clinical Examination (OSCE) has gained importance because of
its reliability [2], and could be used in a summative or formative way
to measure clinical competence [6-8]. There are several medical schools
where formative assessments are established and carried out on regular
basis; unfortunately, it is not very frequent in the Mediterranean
countries [1]. Meanwhile,
undergraduate medical education in Iraq is going through a transitional
period and has started the process of changing its curriculum to
competency-based medical education – formative assessment of students’
performance is a requirement in this process.
Though previous studies suggest that formative-OSCE
contributes positively to final summative examination performance [9],
these were based on the students’ perception [10,11]. Therefore, this
study aims to look for evidence to evaluate if a single formative-OSCE
has an impact on student’s clinical performance in summative
competency-based assessment.
Methods
A single-blind randomized controlled trial was
conducted on fifth year medical students who attended a seven-week
pediatric module at Raparin pediatric hospital, Erbil between September
2016 and May 2017. Our medical college provides a 6-year MBChB program.
Students were divided randomly by the registration office into four
groups: A, B, C and D with around 40 students per group, which attended
the pediatric module at a specific time of the year. At the end of
pediatric module, students’ clinical competencies were assessed by a
summative-OSCE. Students’ performance data (fourth year grade point
average (GPA)) was obtained from student records. A student’s GPA is a
standard way of measuring academic achievement at the end of academic
year. Each course is given a certain number of credits depending on the
content of the course. It is calculated by the
S (scores obtained by
the students in each course x the credit unit of that course) /
S credit units.
The trial was approved by our institutional ethics
committee. All students were suggested to participate in the study and
provided written consent. Student groups were randomized with a computer
program (Microsoft Excel 2010) into two groups: intervention group and
control group. Students were not randomized as individuals from each of
the groups to avoid knowledge contamination between the students of the
same group. We concealed the groups’ allocation until the start of the
intervention (Fig. 1).
 |
|
Fig. 1 Study flow chart.
|
A formative-OSCE was performed for the intervention
group at the beginning of the pediatric module to assess the
competencies they gained from previous modules. The author explained the
purpose of formative-OSCE as a learning experience in the study group.
Failing the formative-OSCE had no adverse effect on the final summative
scores and the participation was voluntary. In comparison, the
participants in control group were attending the standard pediatric
module.
The formative-OSCE design involved a blueprint
development that served as a guideline for the development and
face-validation of the eight stations, which were both interactive and
static. The interactive stations included history taking, examination,
communication and procedural skills while non-interactive stations
included data interpretation, management and a video-station.
The formative-OSCE examiners consisted of two
teaching staff and 11 postgraduate pediatric board trainees, who were
trained by the investigators. At the time of result declaration,
students received feedback on their performance in the formative-OSCE on
a one-to-one basis. Feedback was given by the author as narrative
feedback as well as scores.
The examiners in the summative-OSCE were blinded to
the group assignment and the two-teaching staff who took part in the
intervention, did not participate in the summative exam. The allocation
sequence was generated by a person not involved in the data analysis.
The main outcome was the students’ performance in summative-OSCE. This
was measured by students’ summative-OSCE scores with the passing mark of
a total of at least 50 from all stations.
Statistical Package for Social Sciences (IBM SPSS
version 21) was used for data analysis. Sample size was calculated based
on previous studies [12] by statistical software, the power was set at
90% and a=0.01.
Accordingly, the estimated sample size was 27 for each group.
Considering the non-response rate probability, the authors decided to
include all the students. Students’ t-test used for two independent
samples and paired t-test to compare between pre- and post-module OSCE
scores of the same group. Multiple regression was used to analyze effect
of different factors on summative-OSCE and McNemar test to compare
proportions of the same sample (formative and summative-OSCE success
rate of the intervention group). A P-value of less than 0.05 was
considered significant.
Results
Of the 161 students who attended the seven weeks
pediatric module and screened, 130 were eligible for enrolment (Fig.
1). We excluded 11 students of the intervention group from the
initial analysis as they did not participate in the formative-OSCE due
to their absence on the day of formative-OSCE. There were no significant
differences in the baseline characteristics of the two groups except for
the place of residence (Table I).
TABLE I Baseline Characteristics of Fifth Year Medical Undergraduates Enrolled in the Study (N=119)
|
Factors |
Student-group |
|
Control group
|
Intervention group |
|
(n=69) |
(n=50)
|
|
Place of residence* |
|
Local |
43 (62.3) |
49 (98) |
|
Dormitories |
26 (37.6) |
1(2) |
|
English-based secondary school# |
|
No |
60 (86.9) |
42 (84) |
|
Yes |
9 (13.04) |
8 (16) |
|
Female gender |
38 (55.07) |
27 (54) |
|
Previous year GPA |
Average-grade |
Average-grade |
|
Mean (SD) |
61.48 (6.3) |
66.37 (6.7) |
|
*P<0.001; # P=0.6; $P = 0.9. |
The intervention group’s summative-OSCE mean (SD)
score 64.6 (10.9) was significantly higher than their formative-OSCE
mean (SD) score 53.5 (8.3) (P<0.001). A comparison of both
intervention and control group did not show a statistically significant
difference in pass rate in the summative-OSCE [48/50 (96%) and 67/69
(97%), respectively]. Interestingly, the mean (SD) summative-OSCE score
of the control group 69.2 (10.45) was higher than that of the
intervention group 64.61(10.91) (P=0.02).
Multiple regression analysis revealed that the
summative-OSCE scores were positively correlated with the previous year
grade point average, and negatively correlated with participation in the
formative-OSCE (P<0.001) (Table II).
TABLE II Output for a Multiple-regression Model Where the Dependent Variable is Scores of Summative-OSCE (N=119).
|
Model |
B |
P value |
95.0% Confidence-Interval for B
|
|
|
|
(Lower-Bound,
|
|
|
|
Upper-Bound) |
|
(Constant) |
10.226
|
0.201 |
(-5.542, 25.994) |
|
Previous year GPA |
0.951
|
<0.001 |
(0.703, 1.199) |
|
English-based secondary school |
-0.613
|
0.798 |
(-5.340, 4.114) |
|
Male gender |
0.171
|
0.917 |
(-3.068, 3.410) |
|
Place of residence (dorm) |
1.374
|
0.532 |
(-2.964, 5.713) |
|
Participation in formative-OSCE |
-8.754
|
<0.001 |
(-12.491, -5.018) |
Discussion
The formative-OSCE introduction did not result in a
considerable change in the overall summative-OSCE pass rate in the
intervention group compared with the control group, similar to results
obtained by Chisnall, et al. [6], but it improved the students
mean score in the intervention group if compared with their
formative-OSCE mean.
This finding supports the work of other studies in
this area linking medical students review of formative-OSCE scores and
their performance in summative-OSCE [13]. But it is contradictory to
other researches that appreciate the role of formative assessment in
improving the overall performance in OSCE [14,15].
One criticism of much of the literature on formative
assessment effectiveness is that it does not depend merely on its
availability; it rather relies upon the quality and communication tools
of the assessment feedback [16]. In this study, feedback on students’
performance in formative-OSCE was provided by the authors in form of
comments and numerical scores. Even though it is difficult to disagree
with the efficiency of numerical scores for summative purposes, its use
for formative purposes that guide progress in learning has long been
argued [17]. Numerical scores and letter grades would tend to direct
students’ concentration to the self and away from the task, thus leading
to a negative impact on performance [17,18].
According to cognitive evaluation theory, even
positive feedback that is useful for students can be weakened by
negative motivational effects as a result of giving grades or comparing
the students to a norm [19].
Feedback could be immediate or delayed according to
its timing. When it is planned to facilitate lower-order learning
outcomes, for example, the recall of facts, prompt feedback works best.
However, when higher-order learning outcomes are a concern and
necessitate the transfer of what has been learned to a new situation,
delayed feedback probably works better [20]. In this study, feedback was
given when the results were released (delayed); although, it is
suggested that students prefer immediate feedback [20].
Another factor is that having four summative-OSCEs
for the four groups of the 5th year might have contributed to possible
difference in summative examination difficulty; although, all the OSCEs
had the same blueprint. This was noticed when comparison was made
between the mean (SD) summative-OSCE scores gained by the intervention
group 64.6 (10.9) with what was gained by the excluded students from the
intervention group 53.4 (15) (P<0.001), even though there was no
significant difference in their GPA of the previous year. Whilst this
was a potential limitation, it had the benefit of excluding prior
knowledge influence on success in the summative-OSCEs.
Moreover repeated administration of OSCE by teaching
hospitals improves the performance of students on the successive
summative-OSCE [15]. However, in our study formative-OSCE was carried
out once.
To conclude, students who faced a single
formative-OSCE obtained less summative-OSCE scores than their
peers in control group.
Contributors: MI,NA,AA: study design and concept;
NG was the trial coordinator and participated in data analysis and
interpretation. NA: data collection, data entry and wrote the draft of
manuscript. All authors critically reviewed and approved the manuscript.
Funding: Hawler Medical University. No
contribution to data design, collection, analysis or interpretation was
made by the funding resource. Competing interests: None stated.
Ethical clearance: The study was approved
by Ethics Committee of the College of Medicine of Hawler Medical
University (document no.16, 23/4/2016)
|
What This Study Adds?
• Participation in a single formative-OSCE did not improve
the students’ performance in a subsequent summative-OSCE.
|
References
1. Carrillo-de-la-Peña MT, Baillès E, Caseras X,
Martínez À, Ortet G, Pérez J. Formative assessment and academic
achievement in pre-graduate students of health sciences. Adv Heal Sci
Educ. 2009;14:61-7.
2. Siddiqui ZS. Framework for an effective
assessment: From rocky roads to silk route. Pakistan J Med Sci.
2017;33:505-9.
3. Tridane M, Belaaouad S, Benmokhtar S, Gourja B,
Radid M. The impact of formative assessment on the learning process and
the unreliability of the mark for the summative evaluation. Procedia
-Social Behav Sci. 2015;197:680-5.
4. Pugh D, Desjardins I, Eva K. How do formative
objective structured clinical examinations drive learning? Analysis of
residents’ perceptions. Med Teach. 2018;40:45-52.
5. Konopasek L, Norcini J, Krupat E. Focusing on the
formative: Building an assessment system aimed at student growth and
development. Acad Med. 2016;91:1492-7.
6. Chisnall B, Vince T, Hall S, Tribe R. Evaluation
of outcomes of a formative objective structured clinical examination for
second-year UK medical students. Int J Med Educ. 2015;6:76-83.
7. Sobh AH, Austin Z, Izham MIM, Diab MI, Wilby KJ.
Application of a systematic approach to evaluating psychometric
properties of a cumulative exit-from-degree objective structured
clinical examination (OSCE). Curr Pharm Teach Learn. 2017;9:1091-8.
8. Gupta P, Dewan P, Singh T. Objective structured
clinical examination (OSCE) revisited. Indian Pediatr. 2010;47:911-20.
9. Townsend AH, Mcllvenny S, Miller CJ, Dunn E V. The
use of an objective structured clinical examination (OSCE) for formative
and summative assessment in a general practice clinical attachment and
its relationship to final medical school examination performance. Med
Educ. 2001;35:841-6.
10. Furmedge DS, Smith L-J, Sturrock A. Developing
doctors: What are the attitudes and perceptions of year 1 and 2 medical
students towards a new integrated formative objective structured
clinical examination? BMC Med Educ. 2016;16:32.
11. Farahat E, Javaherian-Dysinger H, Rice G,
Schneider L, Daher N, Heine N. Exploring students’ perceptions of the
educational value of formative objective structured clinical examination
(OSCE) in a nutrition program. J Allied Health. 2016;45:20-6.
12. Jain V, Agrawal V, Biswas S. Formative assessment
as an educational tool. J Ayub Med C Abbottabad. 2012;24:68-70.
13. Bernard AW, Ceccolini G, Feinn R, Rockfeld J,
Rosenberg I, Thomas L, et al. Medical students review of
formative OSCE scores, checklists, and videos improves with
student-faculty debriefing meetings. Med Educ Online. 2017;22:1324718
14. Gums TH, Kleppinger EL, Urick BY. Outcomes of
individualized formative assessments in a pharmacy skills laboratory. Am
J Pharm Educ. 2014;78:166.
15. Lien H-H, Hsu S-F, Chen S-C, Yeh J-H. Can
teaching hospitals use serial formative OSCEs to improve student
performance? BMC Res Notes. 2016;9:464.
16. Radford BW. The effect of formative assessments
on teaching and learning [Master]. Brigham Young University. 2010.
Available from: https://scholarsarchive.byu.edu/etd/2086.
Accessed January 10, 2019.
17. Lipnevich AA, Smith JK. Response to assessment
feedback: The effects of grades, praise, and source of information. ETS
Research Report Series. 2008;1:i-57.
18. Kluger AN, Denisi A. The effects of feedback
interventions on performance: A historical review, a meta-analysis, and
a preliminary feedback intervention theory. Psychol Bull. 1996;9:254-84.
19. Butler R. Enhancing and undermining intrinsic
motivation: The effects of task involving and ego involving evaluation
on interest and performance. Br J Educ Psychol. 1988;58:1-14.
20. Van der Kleij F. Computer-based feedback in
formative assessment. University of Twente 2013. Available from:
https://www.researchgate.net/profile/ Fabienne_ Van_Der_ Kleij/publication/304628867_Computer-based_feedback_
in_formative_assessment/links/57759dbf08aead 7ba0700138/ Computer-
based-feedback-in-formative-assessment.pdf. Accessed January 10,
2019.
|
|
|
 |
|

