|
|
|
Indian Pediatr 2018;55:818-823 |
 |
Quality Improvement
Collaborative for Preterm Infants in Healthcare Facilities
|
|
Srinivas Murki 1,
Sai Kiran1,
Praveen Kumar2,
Deepak Chawla3
and Anu Thukral4
From 1Department of Neonatology,
Fernandez Hospital, Hyderabad; 2Division of
Neonatology, Department of Pediatrics, PGIMER, Chandigarh; 3Department
of Pediatrics, GMH, Chandigarh; 4Department of
Pediatrics, AIIMS, New Delhi; India.
Correspondence to: Dr Srinivas Murki,
Chief Neonatology, Fernandez Hospital, Hyderguda, Hyderabad 500 035,
India. [email protected]
|
Across all healthcare settings, it is important not only to provide safe
and effective healthcare, but also to ensure that it is timely,
patient-centered, efficient and equitable. There is a wide variability
in neonatal and perinatal outcomes in India and other developing
countries, with certain units demonstrating clinical outcomes that match
the developed world, while others showing higher than expected mortality
and morbidity. Collaborative quality improvement initiatives offer a
pragmatic way to improve performance of healthcare delivery within and
between neonatal units. Variations in application of evidence-based
healthcare process and dependent health outcomes can be identified and
targeted for improvement in quality improvement cycles. We herein
describe the concept of Collaborative quality improvement, and the
success stories of the best-known Collaborative quality improvement
initiatives across the world. We also highlight the process and progress
of creating Collaborative quality improvement in our country.
Keywords: Evidence-based medicine, Neonatal intensive care
unit, Outcome, PDSA cycle.
|
|
Quality improvement (QI) in healthcare is "the
combined and unceasing effort of everyone – healthcare professionals,
patients and their families, researchers, payers, planners and educators
– to make the changes that will lead to better patient outcomes
(health), better system performance (care) and better professional
development (learning)" [1]. At the core of this QI is orienting
healthcare towards patient needs or meeting their unmet needs. In the
neonatal intensive care unit (NICU), patient would include both the
infant and his/her parents.
Evidence-based medicine (EBM) is all about promoting
‘practices that work, while eliminating those that are ineffective or
harmful’ [2]. There is always this challenge of implementing what we
know from research to what we do in clinical practice [3]. An important
step in the practice of EBM is to evaluate one’s own performance. This
is where quality improvement provides a framework to the clinicians to
provide best possible care for their patients. Taking cues from other
sectors like aviation and nuclear industry, high reliability and safety
culture concepts are now being applied to the NICU environment also. But
the outcomes measured should not be simply life or death but rather what
the family and infant experience over long-term because of the time
spent in the NICU. Considerations of the lifetime outcomes have shown to
improve care for patients and are the most important measures to collect
[4].
With rapid advancements in neonatal care and
interventions like antenatal steroids, non-invasive respiratory support
and surfactant, survival and morbidities of preterm infants have
improved significantly [5-7]. In both developed and developing
countries, it is important not only to provide safe and effective health
care, but also care which is timely, patient-centered, efficient and
equitable. Each of these six dimensions of quality defined by the
Institute of Medicine in its landmark report can be measured and
prioritized as outcomes to be improved using the QI framework [8]. There
is often wide variability between healthcare facilities for all these
outcomes. Some units achieve outcomes that can be benchmarked, while
others may still be at the bottom of the ladder. Some of the variation
can be attributed to the gap between the recommended and available
infrastructure, monetary resources and personnel, which can be improved
by forming a network of secondary- and tertiary-care neonatal units so
that they can learn from each other on how to improve outcomes with more
effective utilization of available resources [9].
Collaborative QI project involves a group of
professionals from a single or multiple organization who get together to
learn from one another, support and motivate each other in a structured
approach with the intent of improving quality of health services. The
underlying concept is that teams learn faster and are more effective in
implementing and spreading improvement ideas and assessing their own
progress when collaborating and benchmarking with each other.
Collaborative initiatives provide an unique opportunity to look into
various clinical practices, outcomes and healthcare costs across
different participating units, which are operating in similar
demographic and economic conditions. Benchmarking these variations in
clinical practices and outcomes is a powerful motivator for
participating teams to improve many outcomes, as it represents what has
been achieved locally by one’s peers [10].
Collaborative QI methodology was started in North
America in the late 1980s (New England Cardiovascular Disease Study
Group, 1986 and Vermont Oxford Network, 1988) with the approach becoming
more popular as the Breakthrough Series by the Institute for Healthcare
Improvement (IHI) in 1995. Neonatal collaborative QI (Web
Table I) [11-18] projects have ranged from collaborative
working to improve the administration of antenatal steroids to eligible
mothers to compliance with transfusion guidelines [19, 20].
Collaborative Learning
The core concepts of a quality improvement
collaborative include (Web Fig. 1) [21, 22]:
• An improvement collaborative is a shared
learning activity that brings a large number of teams from different
sites to work together to gain rapid achievements in processes,
quality and efficiency in a specific area of care (e.g.,
improve breastfeeding rates, reduce Hospital Acquired Infections)
during a defined time period.
• Essential components of any collaborative QI
are [23]: Identifying specific topic or agenda; Stakeholders or
participants include multi-disciplinary teams from different
centers; Clinical and QI experts to support participant teams; Model
for improvement: Plan and test changes; and Series of structured
learning activities over a pre-defined time period.
• At the outset of starting a collaborative QI is
the identification of a common agenda, where good evidence exists on
best practices and has a potential to improve patient-and
system-outcomes. Well defined agenda ensure participating groups
understand their own processes, outcomes and try to ensure closure
of gap between existing and best practices.
• Organizational structure of Collaborative QI
usually has two wings namely data and quality improvement.
Administration is run by an executive committee that develops and
prioritizes strategic plan. Subcommittee on collaborative quality
improvement analyze data and address priority areas of quality
improvement. Person in charge of administrative, data and quality
improvement oversee day-to-day operations [24].
• Developing implementation packages in QI for
individual units includes creating toolkits, webcasts, workshops and
academic presentations on identified areas of quality improvement
and disseminating the knowledge amongst the individual unit stake
holders after identifying a local champion.
• Clinical practices that are evidence based,
practices in places that are good or best and adaptations that lead
to improved care are shared among the participating centers. These
practices and processes form the implementation packages of a
collaborative QI.
• Participation is voluntary and include
multidisciplinary team of doctors, nursing staff and non-clinical
members from different organization. Usually each team has 2-8
members.
• The participating sites work out and test ways
to put in practice the concepts included in the implementation
package and work to overcome barriers to make them work in their
local settings.
• Participating teams collect a set of core
indicators that define the common outcome indicators and shared
process indicators. The process indicators guide the quality of the
care processes the teams are trying to improve and the achievement
of desired health outcomes.
• Participant teams are guided and supported by
clinical and QI experts who also act as facilitators and provide
technical ideas on clinical and quality improvement strategies.
• Teams test changes by applying an improvement
or change model. In any improvement model an intervention is
introduced, and one or more indicators are monitored and measured to
see the effect of the intervention on the desired outcome. Many
improvement models have been implemented using the Model for
Improvement advocated by the Institute for Healthcare Improvement
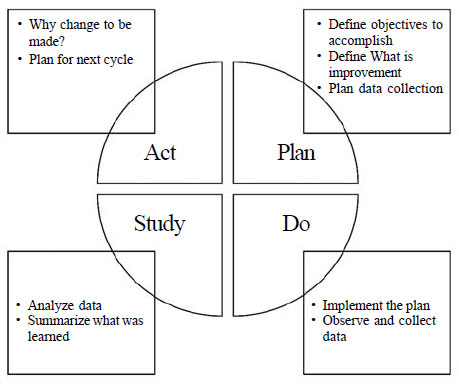
(IHI) (Fig. 1). Most commonly, practice changes in
NICUs are tested using the Rapid Cycle Model, which involves a
series of Plan-Do-Study-Act (PDSA) cycles [25]. In each cycle, a
small change is planned and tested, the outcomes of the process are
monitored and evaluated, and then further changes are made.
• An intervention that is successful in improving
the process is adopted and if the intervention leads to failure it
is either adapted or abandoned. The change ideas are shared among
the participating centers on a regular basis leading to a faster QI
process, decreasing wastage in systems and saving cost.
• Shared learning is the most distinct
differentiating feature of improvement collaborative from a
traditional QI method. Multiple teams try improvements in same topic
area. The teams test and implement process redesigns and changes and
share their experiences in doing so. This facilitates shared
learning of test changes that are both successful and unsuccessful.
Frequent monitoring of process and outcome indicators and sharing of
test changes help to spur the pace of improvement and creates a
friendly competition among the participating teams. The network of
shared learning results in rapid development and testing of
innovations to solve problems, rapid dissemination of effective
changes, and rapid development of effective models of care,
enhancing the original implementation package of evidence-based
standards with operational learning. Shared learning may also
involve communication of results by coaches who visit multiple
teams, use of a Web site where data and experiences are posted,
telephone calls, smaller meetings of representatives from all QI
teams together [21].
• Typically, collaborative QI projects run for
9-18 months; launched with an initial shared learning session of 2
days, where all participants teach and learn. This session includes
sharing the aim, defining changes, measures and outcomes. Also, the
participants develop action plans. In addition, monthly conference
or video call is done to review data reports on strategies, changes
and learning. Feedback and coaching from reports is done once or
twice per month for all. Two to three learning sessions are done
separated over duration of few months, wherein participating units
freely exchange ideas, share strategies employed to overcome
obstacles and create an environment of tactic competition. Three to
six months after the conclusion of collaborative QI project, a
shared learning session is conducted to sustain the improvements
gained [24].
 |
|
Fig. 1 PDSA model (Adopted from IHI
white paper) [22].
|
Another distinct feature of a collaborative is to
spread the improvement beyond the initial teams to larger organizations
and regions and countries. A collaborative usually concludes with a
final package of interventions that have been field-tested and proven to
yield results in a particular setting complemented by a set of
organizational learning that facilitates achieving those results.
Dissemination of information gathered from Collaborative QI activities
through online tools such as CNN-EPIQ’s Virtual Research Community, the
VON’s NICQ pedia or Pediatrix’s Quality Steps system, Pediatrix-University
Web site and so on widen the scale of implementation packages across
clinical settings [13,26]. Collaborative QI offers a pragmatic way to
improve performance of healthcare delivery both at hospital and
community level. The power of collaborative research lies in multiple
centers performing the same project locally and submitting their results
to a coordinating team. The sample size is therefore bigger, and the
results are more generalizable [27].
Challenges in Implementation of a QI Collaborative [22,28]
Current review of evidence suggests that success of
running a quality improvement collaborative depends on following
factors.
• Participating teams which consist of
multi-professionals, like nursing staff are more likely to implement
process changes.
• Administrative and leadership support at
participating units in fostering a culture of quality improvement.
• Geographical span of participating units might
influence success of collaboratives, even though evidence on
comparative efficacy of regional versus national
collaboratives is lacking.
• Nature of participating centers influences
success of collaborative, if all are of similar nature like
(tertiary or primary care), then there is more probability of
completing collaborative.
• Availability of continuous and reliable quality
data on measurement of practices and change is another bottleneck in
the implementation of collaborative QI, maintaining data quality.
Legal and ethical framework regarding data sharing and public
display of collaborative QI data needs to be addressed clearly.
• Not enough evidence to suggest if one
particular method of contact (physical versus online or
email) between the participating centers has influence on
collaborative successes.
• Challenges to health care organization include
convincing people involved in owning up problem solving, aligning
regional quality improvement priorities with those of individual
centers and getting data collection and monitoring systems right.
Organizational barriers can be technical, structural, psychosocial,
managerial, and related to goals and values [29].
• Sustaining the results of Collaborative Quality
Improvement efforts can be particularly challenging and requires
systematic, thoughtful planning and action to ensure that the
changes result in permanent work culture improvement [14].
An Example of Collaborative Quality Improvement in
India
In 2012, a Neonatal collaborative consisting of six
of the best public and private neonatal intensive care units in the
country came together to decrease Healthcare-associated infections.
ACCESS Health International facilitated this with technical assistance
from the Institute for Healthcare Improvement. The collaborative
objective was to decrease healthcare associated infections (HAIs) by
transparently comparing outcomes, sharing best practices, testing
changes for resolving barriers identified by application of problem
analysis tools and acceleration of improvement by learning from each
other. Several changes were done to decrease incidence of HAIs by
increasing the reliability of processes like hand hygiene, aseptic
insertion and maintenance of peripheral and central venous line, aseptic
preparation of parenteral nutrition and intravenous fluids. The
participating hospitals met once every 6 months over a period of 18
months for learning sessions. The first meeting provided an opportunity
for all the clinical leaders to agree upon operational definitions of
the outcome, process measures and capability was built on quality
improvement methods and tools. This helped create a standardized
surveillance mechanism for recording healthcare associated infections.
Across all six hospitals, data was collected along with testing of
changes over a period of 12 months. Four out of six hospitals continued
the surveillance mechanism and improvement activity even after the
collaborative ended, demonstrating the sustainability of the
intervention. The hospital with the highest incidence of healthcare
associated infections showed the maximum improvement with more than 50%
reduction from baseline in both microbiological and clinical blood
stream infections per 1000 patient days. The collaborative approach with
adoption of shared practices, strong engagement of clinical leaders, and
utilization of data were thought to be key reasons for this improvement.
The results of this collaborative led to the scale up of QI work across
two Indian states as the Safe Care Saving Lives project [30].
Scope for Indian Collaborative
Below mentioned are examples of Indian collaboratives
where data was collected and variation in outcome and clinical practices
were measured in NICUs across the country. They can form the basis of
future collaborative QI by shared learning.
National Neonatal Perinatal Database Network (NNPD):
Over a time period of 1995-2003, data collected for about 200,000
neonates across various NICUs in India showed improved neonatal outcomes
over three different time periods, probably attributed to improved care
practices. Across NICUs from a similar geographical area and having
similar disease burden, mortality and morbidity outcomes varied. This is
ideal platform for planning QI collaborative across different health
care practices and outcomes.
VLBW Infant Survival in Hospitals of India (VISHI):
In a more recent collaborative work across India, 11 different level
3 NICU units collaborated for over a period of one year. In this
collaborative effort, outcomes of VLBW infants admitted across different
NICUs were studied. Standardized neonatal mortality rates varied across
different neonatal centers, thus emphasizing the need to start QI
collaborative practice to reduce variability in clinical practice
responsible for varied outcomes [31].
Indian Neonatal Collaborative (INNC): A group of
hospitals led by PGIMER, Chandigarh have created a database platform for
collecting data on neonatal quality indicators and processes. Nearly 12
centers are contributing data to this online database. Centers with at
least 100 VLBW admissions per annuum are eligible for this
collaborative. The live reporting of quality indicators on a dashboard
from this database would form a platform for network centers to initiate
unit based and collaborative improvement projects [32].
All collaborative or networking initiatives in our
country have so far collected invaluable data on neonatal survival,
morbidities across the country. Going beyond passive data collection, a
road map needs to be put in place to establish collaboratives across the
length and breadth of the country to address pertaining problems of VLBW
outcomes, antibiotic resistance, birth asphyxia and many more. Initially
providers need to be identified who are passionate and knowledgeable
about QI. For any quality initiative to succeed the clinical team must
be enthusiastic about improving, transparent and honest in sharing data,
and willing to learn and make practice changes to support improvement.
Ultimately collaborative QI needs to be integrated in day-to-day work
culture (Box 1).
|
Box I The Future Directions for Quality
Improvement in Healthcare of Preterm*
• Including parents of infants in the
implementation of QI collaborative projects, this will achieve
true multidisciplinary nature of teams.
• QI should be a part of medical curriculum,
thus inculcating the culture of collaborative QI very early in
to the day to day life of future lead clinicians and
administrators.
• Research should focus on determining
effectiveness of different approaches of collaborative like
‘breakthrough’ versus ‘communities of practice’.
• Collaboratives are very intense in terms of
manpower and cost, hence there is a need to determine their cost
effectiveness in long term.
*From reference 22.
|
In our country, identifying and creating QI teams at
service delivery or unit level will form the first step in starting
collaborative QI projects. QI team members will work together to
understand their local priorities at unit level, analyze their
processes, test and implement changes to improve performance, and
monitor results. Such QI teams can then be connected to create a
platform to share results, innovations, and challenges and to learn from
one another. Sharing outcome variations and clinical challenges in
different NICU units, will avoid duplication of efforts in solving
problems and provide an opportunity to improve service delivery. Hand
holding or ‘coaching’ will ensure that QI teams function optimally,
possessing knowledge and skills in both technical content related to the
improvement objectives and quality improvement tools.
Contributors: SM, SK: literature search and
drafted the manuscript; PK, DC, AT: guided the framework of the
manuscript and critical review. All authors approved the final version
of manuscript.
Funding: None; Competing interest: None
stated.
References
1. Batalden PB, Davidoff F. What is "quality
improvement" and how can it transform healthcare? Qual Saf Health Care.
2007;16:2-3.
2. Soll RF. Evaluating the medical evidence for
quality improvement. Clin Perinatol. 2010;37:11-28.
3. Glasziou P, Ogrinc G, Goodman S. Can
evidence-based medicine and clinical quality improvement learn from each
other? BMJ Qual Saf. 2011;20:i13-17.
4. Porter ME. What is value in health care? N Engl J
Med. 2010;363:2477-81.
5. National Neonatology Forum: Report 1995: National
Neonatal Perinatal Database network. New Delhi: 1996.
6. National Neonatology Forum: National Neonatal
Perinatal Database. Report of the year 2000. New Delhi, 2001.
7. National Neonatology Forum: National neonatal
perinatal report of the year 2002. New Delhi, 2005.
8. Institute of Medicine (US) Committee on Quality of
Health Care in America. Crossing the Quality Chasm: A New Health System
for the 21st Century. Washington (DC): National Academies Press (US);
2001. Available from: www.ncbi.nlm.nih.gov/books/NBK222274/.
Accessed April 18, 2018.
9. Lasswell SM, Barfield WD, Rochat RW, Blackmon L.
Perinatal regionalization for very low-birth-weight and very preterm
infants: A meta-analysis. JAMA. 2010;304:992-1000.
10. Schouten LMT, Hulscher MEJL, van Everdingen JJE,
Huijsman R, Grol RPTM. Evidence for the impact of quality improvement
collaboratives: Systematic review. BMJ. 2008;336:1491-4.
11. Horbar JD, Rogowski J, Plsek PE, Delmore P,
Edwards WH, Hocker J, et al. Collaborative quality improvement
for neonatal intensive care. NIC/Q Project Investigators of the Vermont
Oxford Network. Pediatrics. 2001;107:14-22.
12. Payne NR, Finkelstein MJ, Liu M, Kaempf JW,
Sharek PJ, Olsen S. NICU practices and outcomes associated with 9 years
of quality improvement collaboratives. Pediatrics. 2010;125:437-46.
13. Walsh M, Laptook A, Kazzi SN, Engle WA, Yao Q,
Rasmussen M, et al. A cluster-randomized trial of benchmarking
and multimodal quality improvement to improve rates of survival free of
bronchopulmonary dysplasia for infants with birth weights of less than
1250 grams. Pediatrics. 2007;119:876-90.
14. Lee SK, Aziz K, Singhal N, Cronin CM, James A,
Lee DSC, et al. Improving the quality of care for infants: A
cluster randomized controlled trial. CMAJ Can Med Assoc J J Assoc
Medicale Can. 2009;181:469-76.
15. Lee HC, Kurtin PS, Wight NE, Chance K,
Cucinotta-Fobes T, Hanson-Timpson TA, et al. A quality
improvement project to increase breast milk use in very low birth weight
infants. Pediatrics. 2012;130:e1679-87.
16. Ozawa M, Yokoo K, Funaba Y, Fukushima S, Fukuhara
R, Uchida M, et al. A quality improvement collaborative program
for neonatal pain management in Japan. Adv Neonatal Care.
2017;17:184-91.
17. Spence K, Henderson-Smart D. Closing the
evidence-practice gap for newborn pain using clinical networks. J
Paediatr Child Health. 2011;47:92-8.
18. Johnston AM, Bullock CE, Graham JE, Reilly MC,
Rocha C, Hoopes RD, et al. Implementation and case-study results
of potentially better practices for family-centered care: The
family-centered care map. Pediatrics. 2006;118:S108-14.
19. Baer VL, Henry E, Lambert DK, Stoddard RA,
Wiedmeier SE, Eggert LD, et al. Implementing a program to improve
compliance with neonatal intensive care unit transfusion guidelines was
accompanied by a reduction in transfusion rate: A pre-post analysis
within a multihospital health care system. Transfusion (Paris).
2011;51:264-9.
20. Lee HC, Lyndon A, Blumenfeld YJ, Dudley RA, Gould
JB. Antenatal steroid administration for premature neonates in
California. Obstet Gynecol. 2011;117:603-9.
21. The_improvement_collaborative. Available from:
https://www.usaidassist.org/sites/assist/files/the_improvement_
collaborative.june08.pdf. Accessed May 29, 2018.
22. IHI Breakthrough Series whitepaper 2003.
Available from: http://www.ncpc.org.uk/sites/default/files/Anita_IHI
Break throughSerieswhitepaper2003.pdf. Accessed April 18,2018.
23. Improvement Collaboratives in Healthcare.
Available from:
https://www.health.org.uk/sites/health/files/Improvement
CollaborativesInHealthcare.pdf. Accessed June 15, 2018.
24. Gould JB. The role of regional collaboratives:
the California Perinatal Quality Care Collaborative model. Clin
Perinatol. 2010;37:71-86.
25. Langley GL, Moen R, Nolan KM, Nolan TW, Norman
CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing
Organizational Performance. 2nd ed. San Francisco, California, USA:
Jossey-Bass Publishers; 2009.
26. Lee SK, McMillan DD, Ohlsson A, Pendray M, Synnes
A, Whyte R, et al. Variations in practice and outcomes in the Canadian
NICU network: 1996-1997. Pediatrics. 2000;106:1070-9.
27. Kilo CM. Improving care through collaboration.
Pediatrics. 1999;103:384-93.
28. Wells S, Tamir O, Gray J, Naidoo D, Bekhit M,
Goldmann D. Are quality improvement collaboratives effective? A
systematic review. BMJ Qual Saf. 2018;27:226-40.
29. Ziegenfuss JT. Organizational barriers to quality
improvement in medical and health care organizations. Qual Assur Util
Rev.1991;6:115-22.
30. Safe Care, Saving Lives. ACCESS Health Int.
Available from: http://accessh.org/project/safe-care-saving-lives/.
Accessed April 18, 2018.
31. Investigators VIS in H of I (VISHI) S, Murki S,
Kumar N, Chawla D, Bansal A, Mehta A, et al. Variability in
Survival of Very Low Birth Weight Neonates in Hospitals of India. Indian
J Pediatr. 2015;82:565-7.
32. Indian Neonatal Collaborative. Available from:
https://innc.org/. Accessed April 18, 2018.
|
|
|
 |
|

