Quality improvement (QI) is defined as the combined
and unceasing efforts of everyone involved in healthcare including
providers, patients and their families, researchers,
planners and administrators to make changes that will
lead to better patient outcomes, better health system performance and
better professional development [1]. Better quality of care (QoC)
ensures that the healthcare provided is safe (avoids harm), effective
(evidence-based best practices), patient centred (care that respects
patients and their preferences), timely (avoids unnecessary delays),
efficient (avoiding wastage) and equitable. QI also helps one to
translate best clinical and scientific evidences into clinical practice.
The key ingredient of any QI initiative is the ‘change’ (context
specific improvement) that is proposed and the ‘methodology’ by which
the change is introduced [1]. QI initiatives in low- and middle- income
countries (LMIC) targeting small and sick neonates have shown benefits
in the form of reduction in neonatal mortality and morbidity [2].
However, overburdened staff and lack of sufficient equipment were
identified as the most common barriers during implementation [2].
While a number of approaches can be used for QI
initiatives, some general principles hold true for all of them. These
include a thorough understanding of the problem to be addressed, the
system and processes that prevail within the unit, appropriate data
collection, choosing suitable changes, executing them, and finally
evaluating and measuring the impact of such changes. All these can be
accomplished only with good leadership support, staff engagement,
motivation and team work. In this article, we share a number of QI
initiatives undertaken in the neonatal unit of our institute and
elaborate our learning from them.
Quality Improvement Journey at Our Center
Setting: Our Neonatal intensive care unit
(NICU) caters to an average of 2800 inborn neonates, in 10 bedded level
III, 12 bedded level II, 8 bedded kangaroo care unit or in the
rooming-in beds. Most neonates are born to mothers with high risk
obstetric conditions and approximately a quarter of them require NICU
admission. NICU team includes highly skilled nurses, four full-time
faculty, fellows undergoing super-speciality neonatal training and
rotating pediatric residents and other support staff.
Way back in 1980s, AIIMS NICU achieved a marked
reduction in neonatal mortality rate (NMR) from 36.6 per 1000 live
births in 1985 to 23.9 in 1986, just by introducing a few changes in
routine practice- (use of intravenous cannula in place of butterfly
needles, reducing intravenous fluid usage, stopping the use of stock
solution, not admitting caesarean babies for ‘observation’, meticulous
adherence to asepsis and promotion of breastfeeding) [3]. This was in
fact a quality improvement activity based on common sense and clinical
acumen but little did we know about its science and implementation then.
The data collected was part of the monthly morbidity and mortality
report. Similarly, there are reports from other parts of country [4] and
abroad [5] wherein implementation of simple interventions (e.g.,
rational admission policy and antibiotic usage, curbing non-essential
routine investigations and interventions, focus on asepsis and training
of nurses) have led to reduced neonatal mortality. These are examples of
‘lean principles’ – whereby better patient outcomes was created by
decreasing non-value added interventions/waste and fewer resources.
While there is no dearth of evidence, what afflicts
most LMIC settings including ours is the struggle to implement them in
practice: the knowledge-implementa-tion gap. This is important because,
while there may be many approaches to implement an evidence; the best
approach in a given setting cannot be determined without understanding
why certain practices and policies prevail within the setting and the
sentiments of people whose behavior we wish to change [6]. We at AIIMS
strived to implement evidence-based practices, succeeded in some, failed
in many but did not formally analyze failures and perhaps focussed more
on outcomes rather than processes.
Learning the science and art of QI: This outlook
certainly got more refined when we embarked on a journey of providing
quality care in a systematic way in August 2015, under the leadership of
the Director of AIIMS. A team comprising of a faculty, a nurse educator
and a resident from the pediatrics department attended a seminar on QI
and brought home clinical wisdom and enthusiasm to initiate QI
activities. They did their first QI project in NICU and tasted success.
QI was infectious; with early and obvious improvements, more people
wanted to be part of the process. Thus with more interest gathering,
participatory learning sessions (3-4 hours each) were organized to guide
members in the scientific way of doing QI. Initially five departmental
teams participated at the first workshop wherein teams brought problems
to work on and went home with an aim statement and to collect a few
baseline data. They formed local teams and came up with change ideas.
They were then taught to test these ideas in small Plan-do-study-act
(PDSA) cycles and to see if the changes led to improvement. The teams
met fortnightly to share progress and help out each other. More help
came from agencies like USAID Applying Science to Strengthen and Improve
Systems (ASSIST) Project and Institute of Healthcare Improvement (IHI),
which hand-held many departmental teams, conducted workshops, webinars
and arranged platforms for sharing QI work. Once a few QI projects were
completed, there emerged champions and local leaders in various
departments who then led the change movement. Frontline workers became
involved and better patient outcomes, client satisfaction and a sense of
fulfilment fuelled more QI projects. In the following paragraphs, we
describe various QI activities done in the NICU.
Improving the Rates of Hand-hygiene – Our Initial QI
Hand-hygiene (HH) is the most effective strategy in
reducing healthcare-associated infection in the unit. AIIMS NICU has a
very strong culture of implementing asepsis routines including HH, yet
the rates remained around 60% similar to most units with rates of 50% or
less [7]. We wanted to implement measures in a step-wise fashion to
improve compliance.
Implementation and evaluation: We designed a
prospective before-after study [8]. The intervention consisted of 4
steps as listed: step 1: standard teaching of health care providers with
posters, videos and self-learning module; step 2: face to face
interaction with practical demonstration and appreciation of hand
hygiene champions of the week; step 3: closed circuit television (CCTV)
monitoring; and step 4: CCTV monitoring with individual feedback for the
missed opportunities of hand hygiene. Each phase of intervention lasted
4 weeks. The compliance with HH was observed by trained research nurses
for the 5 moments of HH at various opportunities. The baseline HH
compliance in the unit was 61.8%, which improved significantly to 77%
after implementation of all 4 steps in a stepwise manner (relative
change 25%, 95% CI: 18% to 32%).
Learning and implications for practice: In
this improvement effort, we focussed on the process – namely performance
of HH and chose all the change ideas at the outset. There is a
possibility that the improvement we saw reflected Hawthorne effect of
being observed and fear of being monitored by CCTV cameras. While
adherence to HH was monitored continuously, the improvement was not
displayed to motivate everyone in the unit. We also did not analyze the
possible causes of poor compliance, barriers in implementation or make
efforts to sustain the improvement. However, the final study result
motivated all.
Improving Exclusive Mother’s Milk Feeding Rates among
Preterm Neonates
Exclusive human milk feeding in preterm
neonates is associated with lower rates of necrotizing enterocolitis
(NEC), sepsis, lesser rehospitalization rates and better
neurodevelopmental outcomes [9]. Early expression of mother’s milk
particularly within 6 hours after delivery and frequent expression are
associated with lactation beyond 40 weeks’ gestational age [10].
However, in reality lactation is delayed for mothers delivering preterm
babies due to various reasons like, being separated from the neonate,
illnesses that preclude oral feeding, maternal anxiety and lack of
support. Despite being very proactive for breast milk feeding in our
NICU, we found that even on postnatal day 7 of life, only 12.5% of all
admitted preterm neonates were on exclusive mother’s milk
feeding. We desired to increase the proportion of neonates
receiving mother’s own milk at postnatal day 7 from the current
rate of 12.5% to 30% over a period of six weeks [11].
Implementation and evaluation: A QI team
comprising of a faculty, two resident physicians, a nurse educator and
two senior staff nurses explored the reasons for poor breastmilk
expression using fish-bone analyses. Baseline data collected for initial
7 days included time of first expression of breast milk (EBM) in mothers
delivering preterm neonates, daily amount of EBM and percentage of
neonates on exclusive mother’s milk feeding in NICU. Poor awareness
among healthcare providers and lack of maternal counselling were
identified as most important causes for the problem. Hence as a change
solution, a comprehensive postnatal counselling was implemented wherein
the bed-side nurse was assigned the responsibility to initiate the first
milk expression within 6 hours of delivery. The mother was educated with
videos on breast feeding and encouraged to pump every 4-hourly as soon
as she was stable postpartum. Successive PDSA cycles focused on staff
motivation and the primary nurse whose neonate achieved exclusive breast
feeding on or before 7
th day
of life was awarded with a certificate. Run charts were displayed
showing percentage of neonates each day on exclusive EBM. This QI also
addressed the supply chain issues like the availability of breast pump
and its accessories as well as a refrigerator for milk storage both in
NICU and postnatal wards.
The NICU team finally succeeded in their efforts.
While the time to first expression of breast milk was 48 hours in the
baseline phase, milk expression began within 3 hours of delivery after
the intervention. The proportion of neonates on exclusive mother’s milk
increased from 12.5% to 81% on day 7 of life. A re-evaluation one year
after implementation showed that the success was sustained with
exclusive EBM rates of 80% on day 7 of life.
Learning and implications for clinical practice:
This QI initiative is an example wherein front-line workers (nurses in
this case) were empowered for initiating milk expression and driving the
entire QI to increase EBM use in NICU. The QI tools used in this
initiative include fish-bone analyses and PDSA cycle for implementation
of change ideas. The entire QI could be done with the available
resources and with continued staff motivation, the team sustained their
efforts even a year later.
Improving Life of Radiant Warmer Probes in NICU
Equipment used in the NICU are costly and failure or
break-down of equipment or its parts affect patient safety and increase
the cost of care. We found that there was frequent breakage of radiant
warmer temperature probes in NICU with one particular unit requesting a
new probe once in 9 days. We wanted to explore and rectify this
equipment failure using QI methods.
Implementation and evaluation: A team was formed
including faculty in-charge as team leader, 4 nurses and a resident
doctor. The potential reasons for temperature probe breakage were
evaluated using 5 whys (Table I).
TABLE I Five Whys Analyses for Deriving the Root Cause of a Problem*
|
Whys |
Question |
Answer what caused the situation |
|
1. |
Why only one NICU was having this specific equipment failure? |
Because this NICU caters to stable growing preterm babies
|
|
2. |
Why probes of stable babies are damaged more often? |
Because, these babies are taken off the warmer more frequently
for kangaroo mother care |
|
3. |
Why probes get damaged with frequent disconnection? |
Because care providers do not know that probes are costly
that they often allowed mothers to do the task themselves |
|
4. |
Why do care providers not aware of this? |
Because no one provided in-service orientation of nurses on
equipment maintenance |
|
5. |
Why was no orientation provided? |
No one thought that this was important. This is the root cause
of the problem in hand. |
The ‘SMART’ (Specific, Measurable, Applicable,
Realistic and Timely) aim was to increase the life span of temperature
probe from the current lifespan of 9 days by 80% over a period of 8
weeks. The change ideas involved providing a refresher course for nurses
on equipment care, supervising mothers and junior nurses while handling
probes and tracking probe breakage. After implementing the PDSA cycle 1,
the life of temperature probe increased up to 40 days, which was not as
good as expected. Exploring the reasons, it was noted that mothers
needed more support and can be taken as partners in QI. In 2
nd
PDSA cycle, the bedside nurses provided face to face education of
mothers on taking care of warmer equipment and made it a point to
discuss status of temperature probes during nursing hand-over in each
shift. After the 2nd PDSA
cycle, the minimum time interval between two temperature probe
break-down increased to median of 60 days as indicated by run chart (Fig.
1).
 |
|
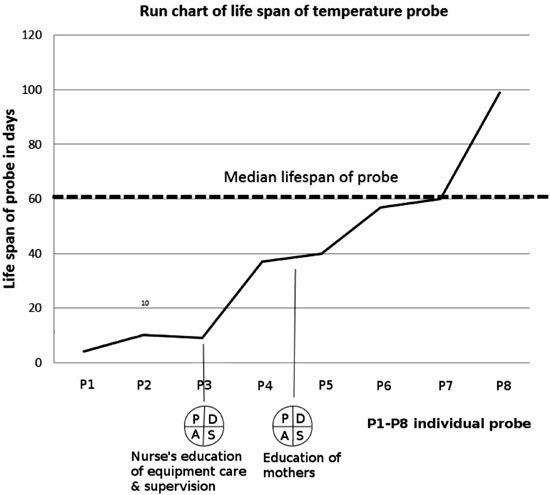
Fig. 1 Annotated run chart showing
life span (in days) of temperature probe in the NICU. P1-P8 on
the x axis indicates an individual temperature probe. The dashed
line indicates median life span.
|
Learning and Implications for clinical practice:
This QI initiative began because one astute nurse recognized that an
order for new temperature probe was being placed too often. She had to
convince the other staff that something was wrong. Unless people
recognize the problems and are involved in initiating the change, there
is often resistance. The team used 5-whys analyses to identify the major
cause of probe breakdown. They came up with solutions, tested them to
see if it worked and then implemented those that worked. Following this
QI, recommendations were made in the unit to provide regular in-service
training of nurses on proper equipment use and its maintenance.
Involvement of mothers as partners in care as suggested by this QI
initiative improved the success rate.
Prevention of Admission Hypothermia Among Preterm
Neonates
Hypothermia is an important contributor of neonatal
mortality and morbidity. During an audit, we observed that
majority of inborn preterm neonates <32 weeks gestation admitted to our
NICU were hypothermic with mean admission temperature of 35.6°C despite
the use of plastic wraps, attention to warmth during resuscitation and
transport. We wanted to improve the mean admission temperatures (AT) of
preterm neonates from the existing baseline of 35.6°C to normal range
(36.5-37.5°C) by implementing all the components of an evidence based
thermoregulation bundle in a stepwise manner using PDSA cycles over a
period of 11 months [12].
Implementation and evaluation: A
multidisciplinary QI team was formed who analyzed the causes of
hypothermia using fish bone analyzes (Web Fig. 1).
During an observation period of three months, a dedicated nurse observed
the delivery room activities and a Pareto chart (Web
Fig. 2) was constructed to identify those few important
practices that needed to change. The Pareto chart revealed that the
application of plastic wrap at birth was not proper in a majority of
cases. Residents explained that the cling wraps crumpled when they tried
to wrap the babies. Thus the changes in PDSA cycle 1, included the use
of plastic bags instead of cling wraps for resuscitation. However, a
look at the run chart revealed that hypothermia was persisting. The team
discussed the issues with resident physicians and nurses and noted that
the plastic bag available in market was stiff and the cut ends remained
open exposing the neonate. Also the delivery room (DR) nurses were not
aware of this QI initiative. So in next cycle, the team reinstituted the
use of cling wraps but used a new way of application. The delivery room
nurses were educated on the importance of hypothermia and how they could
contribute to the initiative. In cycle-3, thermometers were installed in
DR to monitor room temperature and the team co-ordinated with nursing
assistants to ensure prompt transfer from DR to NICU. Frequent feedback
with run charts of AT and appraisal in monthly meetings were done to
ensure compliance and staff motivation in the post-intervention phase (4
months).
We studied a total of 79 preterm neonates during this
QI initiative and noted AT in the post-intervention period with mean AT
of 36.5°C and a significant drop in the incidence of moderate
hypothermia (axillary temperature between 32-36°C) from 50% to 12.5%. We
used a statistical process control chart for trending admission
temperatures over time and demonstrated both a sustained increase in
mean AT as well as decreased variability as reflected in the narrowing
of the control limits (Web Fig. 3). As a
balancing outcome, we did not notice any episode of hyperthermia or
increase in mortality among neonates.
Learning and implications for clinical practice:
This is an example of a complex QI study where team members
implemented a bundle of interventions in different regions of hospital
namely labour room, obstetric operation theatre and NICU. When too many
etiologies for a problem were noted in the fish-bone diagram, they used
the Pareto’s tool to identify those few important causes that contribute
most. The Pareto tool also called as ‘80-20 rule’ states that 20% of the
causes are responsible for 80% of the problems and can help one to focus
on the important few. The first PDSA was not successful but the
team innovated a new method in the second cycle. Some problems need
a multi-pronged approach or a bundle of interventions and one can
simultaneous test 2 or 3 change ideas as opposed to serial testing. The
other lesson from this QI was to involve all stake-holders from the
multiple areas for success. While we used run charts [13] for tracking
and display, we used the statistical process control charts (SPC) to
understand the process better. The SPC charts have an upper and lower
control line (±3 standard deviations) in addition to the central line
which represents the mean as opposed to the run chart where central line
represents median [14]. While both run charts and SPC charts can
visually display data over time and inform whether changes have resulted
in improvement, the SPC charts in addition tell us whether the process
is stable over time. A stable process, has most points near central
line, few points near control lines and none beyond control lines. If
points are above the control line, it indicates a special cause
variation due to changes introduced in the system that needs to be
investigated. There are other pointers to special cause variation too
[14]; and in our example we had eight successive points on the same side
of the centre line as an indicator.
Sustaining an improvement is important and in our
NICU we have implemented the following – regular monitoring of delivery
room temperatures, a checklist to ensure that all resuscitation supplies
and equipment are available and we use admission temperature as an
indicator of quality resuscitation, which is regularly audited for
feedback. Dutta, et al. [15] from India reported a similar QI
initiative to improve admission hypothermia in neonates wherein they
showed lesser hypothermia as well as reduced mortality and late onset
sepsis. The entire QI could be done without major cost, with no
additional staff or new equipment. All the change ideas focussed on
making the existing system and process of care easier for staff to
implement the interventions.
Reducing Breastfeeding Problems at Discharge
Breastfeeding problems are very common, almost 80% of
mothers experience one or more problems related to breastfeeding like
sore, cracked or flat nipples, painful or engorged breasts, difficulty
latching, feeling of decreased milk output etc. while in hospital
[16]. These problems, if not avoided or corrected with proper education
and support can even lead to early cessation of breastfeeding.
Breastfeeding in our postnatal mothers is primarily
assessed by resident doctors and counselling regarding specific or
anticipated problems is done individually at the bedside. Our postnatal
follow up clinic that runs all working days for 2 hours specifically
caters to neonates who are followed up within a couple of days after
discharge. We observed that up to 20-30% of mother-baby dyads presented
with issues related to breastfeeding. Hence we designed a QI initiative
to address this [17].
Our SMART aim was to reduce the incidence of breast
feeding problems at discharge from baseline of 75% to at least 37.5%
among mothers delivering term babies by implementing a post-partum
education package over a period of four months from September 2016 to
December 2016. A QI team was formed and two members (a nurse educator
and neonatal resident) objectively assessed breastfeeding among eligible
mothers in initial phase (4 weeks) using LATCH breastfeeding assessment
scores [18] and collected data on breastfeeding issues. Fishbone
analyses was done, and the team planned to introduce a learning package
for mothers. The nurses in post-natal wards were involved in teaching
activities (phase 2 lasting 4 weeks) which consisted of distributing
pamphlets and video demonstration on breastfeeding. Mothers’ perception
and acceptability of the education package was then assessed on a
5-point Likert scale at the time of discharge. In the phase 3 (2 weeks),
the team stressed on compliance with education package by having a
checklist attached to neonate’s file. Focused group discussions with
postnatal nurses and mothers were conducted to obtain feedback and to
identify barriers in implementation. In phase 4 (2 weeks), a lactation
nurse provided one to one support to all postnatal mothers in addition
and in phase 5 (4 weeks), videos were uploaded in mother’s cell phone
for repeated viewing and other measures were continued.
A total of 330 mother-infant dyads were enrolled in
all the phases of QI. Incidence of breastfeeding problems at discharge
gradually decreased from phase 1 (baseline) to phase 5 from 72.6% to
6.8% (P<0.001) (Web Fig. 4). Compared
to baseline, the proportion of mothers with LATCH score >8/10 at end of
final phase (RR 3.8; 95% CI 2.7-5.5, P< 0.001) as well as each of
the individual phases were significantly greater. The compliance with
discharge checklist increased from 29.8% to 100% and mothers felt that
the educational package had utility as well as acceptability, with
43-65% of mothers strongly agreeing in favor of the education bundle.
Learning and implications for clinical practice:
This QI initiative addressed breastfeeding problems in postnatal mothers
by successful implementation of educational intervention driven by
stepwise rapid cycle PDSA based approach. As outcome measures of
improvement, the team used percentage of mother-infant dyads with
problems at discharge and LATCH score to objectively assess
breastfeeding. As process measures, they tracked the compliance with the
interventions using a checklist. The team used p-chart (p stands for
proportion) to monitor the proportion of mothers with breastfeeding
problems. Similar to a control chart, p-chart also has a central line
which corresponds to the mean proportion and 2 control lines
corresponding to three standard deviations (SD) around the mean. A
special-cause variation that requires investigation is indicated by
point (s) outside the control limits. Web Table 1 lists
the various QI projects done at AIIMS NICU.
Moving Forward With QI Activities
After multiple QI efforts, the NICU nurse educator
emerged as a champion who further supervised more QI work like,
increasing the duration of kangaroo care for preterm neonates in NICU,
decreasing medication errors, antibiotic stewardship and streamlining of
post-natal follow up clinic. QI had also been topics of dissertation
work for postgraduates in the department; the QI work on preventing
admission hypothermia, resolution of breast feeding problems in the
post-natal ward (both discussed above) and improving oxygen saturation
targeting among neonates on oxygen therapy are dissertation work done by
postgraduates. An ongoing QI dissertation work focuses on implementing
potentially best practices in the first week of life among preterm
neonates to reduce the incidence of bronchopulmonary dysplasia.
Dissemination and capacity-building: AIIMS, a WHO
Collaborating Center for Newborn health disseminates QI to other
organizations through its on-line resources, face-to-face workshops and
the Point of Care Continuous Quality Improvement (POCQI) module. A
dedicated website (http://aiimsqi.org/) on quality improvement
provides free resources for teaching and learning QI, and as a platform
for capacity building of teams and sharing QI work. The site also has
short videos and posters of various QI projects done in the Institute.
Many SEARO (South East Asian Regional Organization) countries
participated in a Regional Workshop for Improving Quality of Hospital
Care for Maternal and Newborn Health in May 2016 at New Delhi and have
initiated QI work in their areas. QI project power-point template is
freely available in the site that teams can use as a framework for QI
work.
Teaching and Research in QI: QI is taught to
undergraduates and nursing students at AIIMS. Postgraduates are
encouraged to be part of QI teams in clinical areas and as topics for
research or dissertation work. A good starting point for a dissertation
or thesis on QI work is a single-centre prospective study with a
pre-post design. The focus should be on implementation rather than
testing whether certain practices are effective or not. So careful
planning is essential to understand the existing processes, to identify
how and why the current practices differ from recommended or
evidence-based practice and to involve all stake-holders who may
influence implementation. The team should identify the data that needs
to be collected to measure improvement before study begins. Broadly this
includes process measures (measurement of processes to see if the
changes are being implemented), outcome measures (impact of the changes
on patient or provider outcomes) and balancing measures (unexpected
outcomes or changes both beneficial or harmful that are introduced
either in the same system or other parts of system due to improvement
efforts) [19]. For example, if a team plans to implement skin-to-skin
care (STS) at birth for neonates, exclusive breastfeeding rates at
discharge can be taken as outcome measure, the percentage of eligible
mother-baby dyad experiencing STS, number of STS checklists filled per
month and time to first breastfeeding can be process measures and
incidence of acute life threatening event in neonate (desaturation or
bradycardia) during STS can be chosen as balancing outcome. Published
guidelines are available for reporting QI work in order to improve the
completeness and accuracy of reporting so that improvement efforts can
be reproduced at other suitable settings [20]. It is equally important
to publish QI work to share one’s improvement experiences, so that
others working on similar problems can adopt or adapt the change ideas
without wasting time, effort and money testing the same ideas.
Learning From QI at AIIMS
What started as small projects in a few departments
mushroomed into several projects wherein several other departments like
Rajendra Prasad Ophthalmic Sciences Centre, Emergency medicine,
Pediatrics, Obstetrics, Cardio-Neuro centre and Jai Prakash Narayan Apex
Trauma Institute also participated. QI made people recognize the
problems in their system, utilize various tools (process mapping,
fish-bone analyses, 5 whys) to understand the cause, come up with
changes or solutions tailored for their system, test the changes in
small scale over a short period or on few patients (PDSA cycles), and
adapt/adopt or abandon the changes and finally implement them. People
understood that not all changes lead to improvement and collecting data
to assess baseline performance and reassessing performance over time
using annotated run charts or statistical process control charts help in
differentiating day-to-day variations from improvement. Importantly, the
teams learnt the scientific way of doing QI activities. There was a lot
of learning from each project (both success and failure) that people
shared in common meetings. Salient learning points are given below:
Bottom up approach: We created a culture for QI
in the unit by building conviction among front-line workers. The human
element is the most important component of any QI success story and
staff motivation and engagement is essential to work towards a common
goal [21]. Each team member contributes to improvement and in many
situations, we observed practical change ideas not from leaders but from
front-line staff. In our case, NICU nurses identified the problem of
frequent temperature probe breakdown and came up with change ideas like
empowering the bedside nurse to help mothers with milk expression; the
housekeeping staff volunteered in hypothermia QI and offered timely and
quick transport of neonates to NICU, and mothers of admitted neonates
joined as partners in some QI initiatives.
Understand the system and eliminate waste:
Traditionally, the solution to most problems are handled by increasing
human or material resources; but in healthcare system in which resources
are limited, focussing one’s attention to understanding the system to
identify the root cause and eliminating the redundant and wasteful
processes can help to utilise resources effectively [22]. In our case,
breastfeeding counselling by multiple team members with different
messages, lack of supplies in the delivery room despite their
availability etc. could be rectified when the counselling became more
standardized using pamphlets/videos and a checklist was used for
arranging supplies in the delivery room. Behavioral change of
healthworkers is also important in eliminating waste and facilitating
this change will require education, training, motivation and feedback.
Step-up and then scale-up: It is very essential
that initial projects be simple, doable, patient-centric and under the
control of the team members. Disease processes or problems with
multifactorial etiologies take time or produce no improvement at all.
Undertaking such projects at the outset would demotivate staff who may
feel over-burdened and incapacitated. Our team felt comfortable to use
the Institute for Healthcare Improvement’s Plan-Do-Study-Act (PDSA)
cycle for rapid cycle improvement and changes were accomplished through
small and frequent PDSAs [23]. Only change ideas that were tested on a
small population and adapted for local context were implemented on a
large scale. Building sustainability in each project is so important
[24], that improvements are maintained in long run and the changes
become a new norm in the unit. This involves making changes in the
system itself, use of visual reminders, posters, score cards and
identifying champions who would lead the change movement. In our NICU,
the following system changes were implemented to sustain the
improvements; regular in-service training on equipment handling for
nurses and residents, installation of room thermometers in delivery room
and tracking of temperatures each shift, charting admission temperatures
in the NICU admission register as a quality indicator, and use of videos
for breastfeeding counselling.
Celebrate and share success: Having QI meetings
both within and between departments helps to show case activities and
rally slow movers to gain pace. The QI teams from various departments
attended learning sessions and workshops organized by AIIMS from time to
time where they had the opportunity to learn from experts, presented
their work and shared their experiences. The teams also met face-to-face
with other teams, participated in webinars and conference calls, and
presented their work at conferences. Teams learnt that they could learn
and achieve more by collaboration than working in silos [25].
Time and patience surpasses hurdles: We
understood early that problems have to be solved by a team of people and
getting people on board could sometimes be challenging. Such factors
include staff misunderstanding the principles of QI, feeling
over-burdened with data collection, fear of being monitored or blamed
for poor performance or just an inertia to change. In our hand hygiene
QI, we noticed nurses’ resentment against being monitored, in our
exclusive breast feeding QI, only a couple of nurses from one NICU were
involved. Thus initially like-minded ones teamed up but with time even
the disinterested become passionate about change. Nurses participating
in QI mentored fellow nurses, and with time came up with ways to collect
or add essential data in the nursing flow sheet itself thus decreasing
additional paperwork and burden.
Organizations striving to improve their outcomes
should initiate and support quality improvement activities. The
important requisites for successful QI ventures are listed in Box
I.
| |
|
Box I Key Messages for Organizations
Planning QI Activities
Leadership support with a vision for quality
improvement. Leaders should encourage and motivate staff
involved in QI and also support shared goals for performance.
Capacity building of staff for QI by training
them in the art and science of QI. Encourage teams to attend
learning sessions and workshops. Allow staff to set aside time
for improvement activities apart from their work.
Empower teams to run and manage systems and
introduce changes at their level.
Dedicate time and resources to measure
performance over time. All QI work should be data driven.
Encourage all team members to openly discuss both success and
failure. Allow collaboration between teams in the organization.
|
Contributors: SS, AS: participated in QI, and
drafted the manuscript; MJ: supervised and implemented QI activities in
NICU, collected data; AT: supervised QI in NICU, data collection and
analyses; MJS: supervised QI in NICU, data collection and analyses; AKD,
RA: concept and design. Revised manuscript and were involved in QI
activities in NICU.
Funding: None; Competing interest: None
stated.
References
1. Batalden PB, Davidoff F. What is "quality
improvement" and how can it transform healthcare? Qual Saf Health Care.
2007;16:2-3.
2. Zaka N, Alexander EC, Manikam L, Norman ICF,
Akhbari M, Moxon S, et al. Quality improvement initiatives for
hospitalised small and sick newborns in low- and middle-income
countries: a systematic review. Implement Sci. 2018;13:20.
3. Singh M, Paul VK, Deorari AK, Ray D, Murali MV,
Sundaram KR. Strategies which reduced sepsis-related neonatal mortality.
Indian J Pediatr. 1988;55:955-60.
4. Mukherjee SB, Bandyopadhyay T. Perinatal
mortality- what has changed? Indian Pediatr. 2016;53;242-3.
5. Darmstadt GL, Ahmed ASN, Saha SK, Azad Chowdhury
MA, Alam MA, Khatun M, et al. Infection control practices reduce
nosocomial infections and mortality in preterm infants in Bangladesh. J
Perinatol. 2005;25: 331-5.
6. Varkey P, Kollengode A. A framework for healthcare
quality improvement in India: the time is here and now! J Postgrad Med.
2011;57:237-41.
7. Pittet D. Improving compliance with hand hygiene
in hospitals. Infect Control Hosp Epidemiol. 2000;21:381-6.
8. Gopalakrishnan S, Agarwal R, Paul VK, Deorari AK.
Effect of stepwise interventions aimed at improving hand hygiene
compliance among healthcare providers in a level III neonatal intensive
care unit: Before and after study: Dissertation submitted to the faculty
of Department of Pediatrics, AIIMS, New Delhi 2015.
9. Johnston M, Landers S, Noble L, Szucs K, L V.
Breastfeeding and the use of human milk. Pediatrics. 2012;129:e827-41.
10. Furman L, Minich N, Hack M. Correlates of
lactation in mothers of very low birth weight infants. Pediatrics.
2002;109:e57.
11. Sethi A, Joshi M, Thukral A, Dalal JS, Deorari
AK. A quality improvement initiative: improving exclusive breastfeeding
rates of preterm neonates. Indian J Pediatr. 2017;84:322-5.
12. Sivanandan S, Jeeva Sankar M, Thukral A, Agarwal
R, Paul VK, Deorari AK. Quality initiative on implementation of golden
hour bundle to improve outcomes of preterm neonates <32 weeks gestation:
focus on thermoregulation: Dissertation submitted to the faculty of
Department of Pediatrics, AIIMS, New Delhi, 2016.
13. Perla RJ, Provost LP, Murray SK. The run chart: A
simple analytical tool for learning from variation in healthcare
processes. BMJ Qual Saf. 2011;20:46-51.
14. Benneyan JC, Lloyd RC, Plsek PE. Statistical
process control as a tool for research and healthcare improvement. Qual
Saf Health Care. 2003;12:458-64.
15. Datta V, Saili A, Goel S, Sooden A, Singh M, Vaid
S, et al. Reducing hypothermia in newborns admitted to a neonatal
care unit in a large academic hospital in New Delhi, India. BMJ Open
Qual. 2017;6:e000183.
16. Colin WB, Scott JA. Breastfeeding: Reasons for
starting, reasons for stopping and problems along the way. Breastfeed
Rev. 2002;10:13-9.
17. Mangla MK, Jeeva Sankar M, Deorari AK, Thukral A,
Agarwal R, Paul VK. Quality improvement study to reduce incidence of
breastfeeding problems at discharge in postnatal mothers who delivered
at term gestation: Dissertation submitted to the faculty of Department
of Pediatrics, AIIMS, New Delhi; 2017.
18. Jensen D, Wallace S, Kelsay P. LATCH: A
breastfeeding charting system and documentation tool. J Obstet Gynecol
Neonatal Nurs. 1994;23:27-32.
19. Mainz J. Defining and classifying clinical
indicators for quality improvement. Int J Qual Health Care.
2003;15:523-30.
20. Davidoff F, Batalden P, Stevens D, Ogrinc G,
Mooney S, Group SD. Publication guidelines for quality improvement in
health care: Evolution of the SQUIRE project. Qual Saf Health Care.
2008;17:i3-9.
21. Baker DP, Day R, Salas E. Teamwork as an
essential component of high-reliability organizations. Health Serv Res.
2006;41:1576-98.
22. Bentley TG, Effros RM, Palar K, Keeler EB. Waste
in the US health care system: A conceptual framework. Milbank Q.
2008;86:629-59.
23. Harolds J. Quality and safety in health care,
part I: Five pioneers in quality. Clin Nucl Med. 2015;40:660-2.
24. Barker PM, Reid A, Schall MW. A framework for
scaling up health interventions: Lessons from large-scale improvement
initiatives in Africa. Implement Sci. 2016;11:12.
25. Nembhard IM. Learning and improving in quality
improvement collaboratives: Which collaborative features do participants
value most? Health Serv Res. 2009;44:359-78.

