reterm babies with Retinopathy of prematurity
(ROP) often require multiple hospital visits for retinal screening and
follow-up [1]. The examination is usually performed in neonatal
intensive care units (NICU) or specialized ROP clinic at tertiary eye
care centres. With increasing neonatal care and improved survival of
preterm infants, the magnitude of ROP blindness in India is worrisome
[2]. Also due to improved screening services and detection of treatment
requiring ROP, referrals to our tertiary eye care hospital was seen to
be increasing.
Outpatient/clinic waiting time is an important
parameter to assess quality of health care and patients’ satisfaction
towards hospital services [3]. We observed that there is a problem of
long waiting time for these preterm babies during each visit at the ROP
clinic in our hospital. These preterm babies are required to be kept
fasting for one hour prior to procedure, but it gets extended
indefinitely leading to prolonged crying and risk of systemic
instability. The increased waiting may also increase stress in parents,
and also the clinical staff. We undertook this quality improvement (QI)
project with the aim of reducing the maximum waiting time of preterm
babies in ROP clinic by 30% from baseline in 8 weeks.
Methods
This QI project was done in the ROP clinic of a
tertiary eye care hospital where preterm babies report for screening and
follow up of ROP. The quality improvement (QI) team involved in this
project included a faculty member (team leader), two senior residents
(post-MD), two junior residents (postgraduate students), a nursing
officer, and a registration counter staff. The ROP clinic at our
tertiary-care centre runs twice-a-week and is visited by around 30-40
preterm babies in each session.
The baseline process flow is as follows: the
registration time for these babies starts from 12.30 PM till 1 PM, and
then again from 2 PM to 3 PM. During the lunch time (1 PM to 2 PM), the
patient cards are collected, fasting instructions are given, and
pupillary dilation is performed by the nursing officer. The clinic
starts at 2 PM when two junior residents (JR) and one senior resident
(SR) arrive and set up the examination tables and equipment. The JR
issues wide angle viewing lens for use with the retinal camera (Retcam)
from lab in-charge after 2 PM. Thereafter the examination procedure
starts. Sometimes another SR arrives at 2.30 PM (if available), and the
faculty member arrives at 2.45 PM, to run 2-3 parallel examination
stations (Fig. 1).
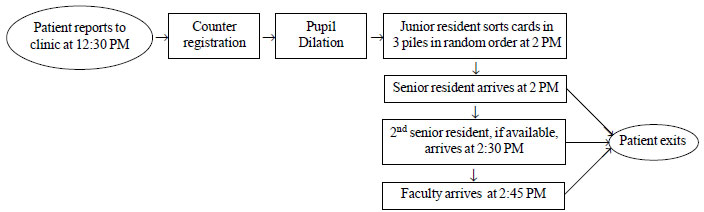 |
|
Fig. 1 Baseline process flow chart
for preterm babies attending the ROP clinic.
|
The baseline data was collected over initial 3 weeks.
A fishbone root cause analysis was done to identify issues with the
policy, people, place and processes responsible for long waiting time (Web
Fig. 1). Three Plan-Do-Study-Act (PDSA) cycles were
implemented.
First PDSA cycle: It was implemented in the 4th
week. Here the JR segregated the cards according to first-come
first-served basis and sorted them into three piles (one for each SR and
one for the faculty), instead of a random pile. The purpose was to
efficiently segregate patients depending on whether they need to be seen
by an SR (old cases), faculty (new cases/opinion cases/post-operative
cases) or had to undergo wide angle digital imaging by SR. The second
change was that the second SR was made permanent and he reported on time
at 2 PM, so that the clinic capacity was increased and it could start on
time.
Second PDSA cycle: It was implemented in the 5th
week wherein the faculty member also reported to the clinic at 2 PM.
This ensured that all staff came on time and all three stations started
at 2 PM. Since the card pile for faculty was segregated, he could
independently start examining the new cases, and opinion cases could
follow later.
Third PDSA cycle: It had several interventions
aimed at timely reporting of staff, timely availability of equipments,
proper examination order, and rescheduling of old and new patients.
These changes of this PDSA were tested for the next nine clinic days for
checking sustenance of the intervention. JRs and one SR reported now at
1.50 PM, sorted out the cards in three piles as before, and arranged all
the equipments by 2 PM, this ensured the preparation time occurred
before 2 PM, and the clinic could actually start at 2 PM. The 2nd SR and
the faculty member reported at 2 PM, which allowed three examination
stations to start functioning from 2 PM. The Retcam lens was issued
beforehand and kept safe within the clinic cupboard, instead of issuing
from the lab in-charge every time, who was on lunch and often lens
procurement was delayed. The postoperative patients were called at 2 PM
(instead of 12.30 PM) as their pupils were already dilated on
postoperative cycloplegic medication, and they could be examined
directly by faculty, who was now present at 2 PM.
To assess the impact of interventions, we measured
the ‘average waiting-time’, ‘maximum waiting-time’ and ‘last baby
entry-time’. The Waiting-time was defined as the time interval from the
arrival of baby at ROP clinic till first examination by the Senior
resident (post-MS)/faculty member. The Average waiting-time (AWT) was
defined as algorithmic mean of waiting-time of all babies on each clinic
day. The Maximum waiting-time (MWT) was the maximum time any baby had to
wait before examination, and was calculated from the record sheet. The
Last baby entry time (LBT) was defined as the time to examination for
the baby entering last in the clinic premises, calculated from start of
clinic at 2 PM – it approximately indicated total clinic time. To ensure
the completeness and accuracy of data collection, one JR was solely
allotted the task of recording the waiting time of babies on a record
sheet starting from 12.30 PM in every clinic. The QI team was shown the
power point presentation of benefits with each PDSA and were motivated
to further reduce the waiting time.
The data were entered into Excel sheet and analyzed
using STATA SE 12.1 software.
Results
The study was performed over 19 clinic days. The
number of babies attending the ROP clinic varied across different clinic
days during the study period (range 26- 39, median 32). The median
(range) AWT, MWT and LBT at baseline (6 clinic days) were 90.5
(74.1-118.8) min, 177.5 (160-190) min and 111 (90-118) min,
respectively.
During 1st PDSA cycle, all these measures had
worsened from baseline, indicating the changes did not work as expected
(Fig. 2). During the 2nd PDSA cycle, all the measures were
improved from 1st PDSA cycle. During the 3rd PDSA cycle, the median
(range) AWT, MWT and LBT were 77.6 (55.2-94.3) min, 122 (110- 135) min,
and 60 (45 to 80) min, respectively (Fig. 2).
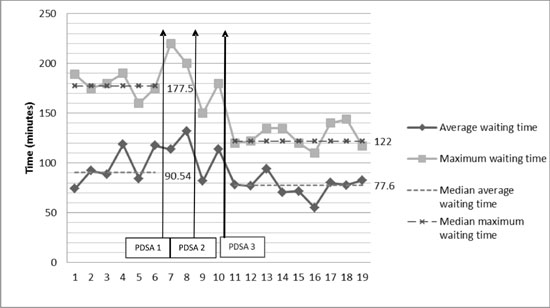 |
| (a) |
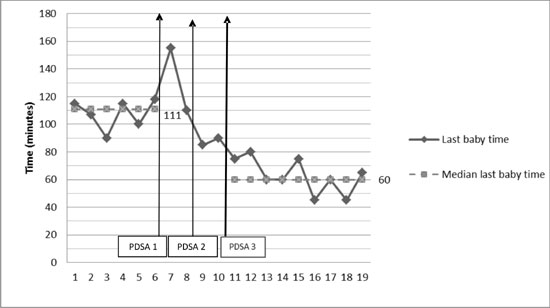 |
| (b) |
|
Fig. 2 (a) Change in Average waiting
time and Maximum waiting-time at a ROP clinic after a
Quality-improvement intervention; (b) Change in Last baby
entry-time at a ROP clinic after a Quality-improvement
intervention.
|
At the end of the project, the median AWT, MWT and
LBT decreased by 14.3%, 31.2%, and 46%, respectively. The changes were
sustained over the next few weeks.
Discussion
The waiting times for preterm babies decreased in our
ROP clinic after well planned interventions in three PDSA cycles. The
maximum decrease was noted in LBT (46%) followed by MWT (31.2%). The
specific aim of reducing MWT to at least 30% of baseline was achieved.
Multiple PDSA cycles were the strength of this study as improvement with
the previous cycle motivated QI team to work harder in the subsequent
cycles.
PDSA is a widely accepted method of quality
improvement in healthcare system [4]. The first PDSA was aimed at
improving the process related flow by segregation of cards, which
allowed clear division of patient flow and allowed patient’s reporting
earlier to be seen earlier – which not only brought in a sense of order
in patient flow, but also reassured the patients that late reporters do
not jump the queue. The staff capacity was permanently increased by
bringing in one more working SR (who previously used to come if
available), which led to three examination stations. However, these
steps increased the waiting time which was surprising to the team. It
was because the clinic was not starting on time as the preparation time
was prolonged, and the staff came late. It highlights how small-scale
testing helps to realize that outcomes may not occur as expected. A
failed PDSA should not be disheartening, as it provides deeper insights
into the process problems, and provides new ideas to tweak the process.
The 2nd PDSA was aimed at all the staff (SR and
faculty member) starting clinic on time, which led to an improvement,
but was far from the expected goals. More extensive tweaks were tested
in the 3rd PDSA – it reduced preparation time (by starting even earlier
and keeping all equipment ready), and optimized flow of postoperative
patients and significantly reduced their waiting times. These small
quality improvement changes were tracked across the next few weeks and
the changes were sustained.
The study had a few limitations. Due to quick changes
and less clinic visits between each PDSA cycle, we could not
statistically analyze the difference achieved with each PDSA cycle. The
reporting time was noted by the resident from the time they entered the
clinic area, but it could have been logged in a more automated way by
coordinating with the patient registration time. We are now working on
an automated way of measuring waiting times, which will allow hospital
administrators to easily visualize and optimize patient waiting times
across different clinics in our hospital. There were no balancing
outcomes measured. A more detailed interview/questionnaire from parents
before and after the study would have strengthened the study with useful
qualitative data.
To conclude, the ROP clinic waiting
area time was significantly reduced by small QI changes and served as a
model for improvement in other clinics at our hospital. Small scale
testing can lead to systems improvement via repeated PDSA cycles and can
significantly improve patient quality of care.

