|
|
|
Indian Pediatr 2018;55:773-775 |
 |
Reducing Preoperative
Waiting-time in a Pediatric Eye Operation Theater by Optimizing
Process Flow: A Pilot Quality Improvement Project
|
|
Parijat Chandra, Ruchir Tewari, Yangchen Dolma,
Deepsekhar Das and Devesh Kumawat
From Dr Rajendra Prasad Centre for Ophthalmic
Sciences, AIIMS, New Delhi, India.
Correspondence to: Dr Parijat Chandra, Additional
Professor of Ophthalmology, Room No 373,
Dr Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute
of Medical Sciences,
Ansari Nagar, New Delhi 110 029, India.
Email:
parijatchandra@gmail.com
Received: December 17, 2017;
Initial review: January 27, 2018;
Accepted: June 12, 2018.
|
Objective: To decrease the preoperative area
waiting-time for children posted for eye surgery.
Methods: A pilot quality improvement project
was conducted in a single paediatric eye operation theatre in our
tertiary-care hospital. Operation theatre process flow was analyzed,
baseline data was collected, and two Plan-Do-Study-Act cycles were
performed on consecutive days. Average and maximal waiting-time were
recorded across six operation theatre days.
Results: The average and maximal waiting time
at baseline were 221 and 390 minutes, respectively. After two rapid
Plan-Do-Study-Act cycles, these were reduced to 29 (87% reduction) and
52 minutes (87% reduction) from baseline, respectively, and could
subsequently be sustained.
Conclusion: Preoperative waiting time in
ophthalmic operation theatre was significantly reduced by simple process
flow optimization, thereby improving quality of care.
Keywords: Healthcare delivery, Plan-do-study-act cycle,
Start-time delay.
|
|
P
ediatric eye surgeries are performed under
general anaesthesia (GA) at our tertiary-care eye hospital, but we noted
many children kept waiting for long periods in the preoperative area
leading to overcrowding, difficulty in patient coordination, increased
risk of infection and prolonged fasting periods for small babies,
leading to increased anxiety of the child and parents. Effective
operation theatre (OT) planning is must for optimal utilization of
treatment facilities [1]. Waiting-time is an important parameter to
assess quality of healthcare and patients’ satisfaction towards hospital
services [2]. The aim of this pilot Quality improvement (QI) project was
to reduce waiting time in the GA waiting-area for inpatients by 50% in a
four-week period.
Methods
This pilot project was done in a single eye OT of a
single surgical unit (operating twice-a-week) at a tertiary-care eye
hospital. A team was formed consisting of a faculty member (team
leader), a senior resident (Post-MD), a junior resident (Postgraduate
student) and a member of the nursing staff.
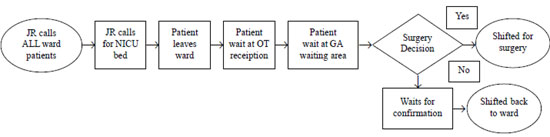
The baseline process was studied (Fig. 1).
The junior resident (JR) called all patients from the ward, and then
called the Neonatal Intensive Care Unit (NICU) for arrangement of backup
postoperative bed. The patients left the ward and arrived at the OT
reception area and were shifted inside to the GA waiting area. If found
fit by the anaesthesia team, they were shifted for surgery, else awaited
confirmation by the JR, and exited from the OT.
 |
|
Fig. 1 Baseline process flow chart
depicting patient flow from ward to operation theatre till exit.
|
All eight patients posted for surgery were called
much before the arrival time of the anaesthesia team i.e. 8.30
AM. Two of these patients were cancelled after five hours of waiting. An
infected case posted for an intravitreal injection had to wait for over
6 ˝ hours. two ‘plan do study act (PDSA)’ cycles were performed on two
consecutive OT days.
1 st
PDSA cycle – The JR only called the first two
patients from the inpatient ward. No calls were made before 8 AM, and
only a single JR called so as to avoid confusion. The third patient
would be called after the first case exited OT recovery area after
surgery. The JR would physically escort cancelled patients out of the
OT.
2 nd
PDSA cycle – The JR only called the first ward
patient in the morning. The pre-anaesthetic examination and neonatology
clearance was ensured the previous evening. Both these departments were
supportive for this change and no resistance was encountered. The NICU
team was informed by 8 PM by email. If no one replied, NICU bed was
considered available and no calls were made to NICU in morning. The
patient was kept ready in the ward in OT clothes, and parents were
advised to take the stairs instead of waiting for lift. The JR kept
checking the OT reception area and shifted these babies into the GA
waiting area quickly. The JR called the second case only after the first
case started; in case of bilateral eye surgery, when the second eye
surgery started; in case a multipart surgery by different surgeons to be
performed, when the last surgeon started the surgery. Surgery was
considered started when the surgical eye drape was cut.
Outcome Parameters - The waiting-time was defined
as the time from the patient reporting to the OT reception area (outside
the OT) to the time when the baby was shifted for surgery into the OT.
The ‘average waiting- time was defined as the mathematical mean of
waiting-time of all babies posted for surgery in that OT. The maximum
waiting-time was the maximum time any baby had to wait before being
shifted for surgery or out of the OT and was calculated from the record
sheet. The data was collected across a total of six OT days to test the
sustenance of changes.
Results
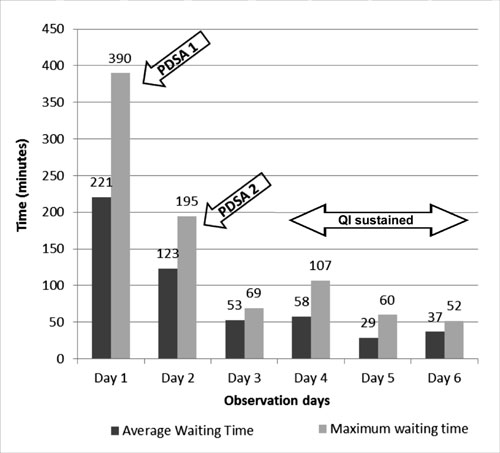
The study was performed over six consecutive OT days
over three weeks with baseline data being collected on the first day.
The number of patients operated on these days were 3, 3, 4, 3, 4, 4,
respectively. The Average waiting-time and Maximal waiting-time at
baseline were recorded as 221 minutes and 390 minutes, respectively.
The Average waiting-time reduced to 123 minutes (44%
reduction) after the first PDSA cycle and further maximally to 29
minutes (87% from baseline) after the second PDSA cycle. Similarly, the
Maximum waiting-time reduced to 195 minutes (50% reduction) and further
maximally to 52 minutes (87% reduction) after the first and second PDSA
cycles, respectively (Fig. 2). The changes were sustained
over next 3 days. Statistical analysis could not be performed due to
small number of data points.
 |
|
Fig. 2 Bar chart depicting
sustained reduction in average and maximum waiting time
following two Plan-Do-Study-Act cycles.
|
Discussion
The need of effective and organized OT planning for
continuous quality improvement has been a concern for hospital
management. The communication gap among anaesthesiologists, surgeons and
nursing staff is known to be a factor for start time delays and high
waiting time in OT [1], and QI methodologies can significantly improve
surgical care, from reducing infection to increasing OT efficiency [3].
This pilot QI project highlights the importance of
collection of baseline data to detect notable waiting time issues. PDSA
is a widely accepted method of quality improvement in healthcare systems
[4]. Repeated PDSA cycles lead to better understanding of the process
flow issues, with identification of new factors providing better than
expected outcome. Rapid PDSA changes across 2 OT days led to quick
reduction in waiting times, JR and this led to a less crowded GA waiting
area, and more efficient workflow, which can indirectly lead to more
cases being operated in the same OT day.
Since it was a pilot project, the waiting time was
recorded only for six OT days. This is a limitation of the study and
data collection over a longer period of time would have provided better
insight into sustenance of quality improvement. These simple tweaks in
process flow can be easily scaled and implemented across different
operation theatres (not necessarily in eye OTs) to decrease waiting
time. This project highlights how a common sense approach to tweak the
system process flow can lead to improved patient quality of care at no
extra cost.
Acknowledgements: This pilot project was
conducted as part of QI training sessions at our center under the
guidance of teams from IHI and USAID ASSIST.
Contributors: PC and RT: Conceptualization of
research and interpretation of data; DD, YD and DK: Data collection; RT,
DD and DK: Manuscript preparation; All authors were involved in
critically revising the manuscript and approving the final manuscript.
They agree to be accountable for all aspects of this research.
Funding: None; Competing interests:
None stated.
|
What This Study Adds?
• Small changes in the process flow may lead
to significant reduction in waiting-time at no extra cost.
|
References
1. Gupta B, Agrawal P, D’souza N, Soni KD. Start time
delays in operating room: Different perspectives. Saudi J Anaesth.
2011;5:286-8.
2. Ahmad BA, Khairatul K, Farnaza A. An assessment of
patient waiting and consultation time in a primary healthcare clinic.
Malays Fam Physician. 2017;12:14-21.
3. Nicolay CR, Purkayastha S, Greenhalgh A, Benn J,
Chaturvedi S, Phillips N, Darzi A. Systematic review of the application
of quality improvement methodologies from the manufacturing industry to
surgical healthcare. Br J Surg. 2012;99:324-35.
4. Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell
D, Reed JE. Systematic review of the application of the
plan–do–study–act method to improve quality in healthcare. BMJ Qual Saf.
2014;23:290-8.
|
|
|
 |
|

