|
|
|
Indian Pediatr 2018;55:768-772 |
 |
A Quality Improvement
Initiative for Early Initiation of Emergency Management for Sick
Neonates
|
|
Asim Mallick, Mukut Banerjee, Biswajit Mondal,
Shrabani Mandal, Bina Acharya and Biswanath Basu
From Department of Pediatrics, Nilratan Sircar
Medical College and Hospital, Kolkata, India
Correspondence to: Dr Mukut Banerjee,
Assistant Professor, Department of Pediatrics, Nilratan Sircar Medical
College and Hospital, Kolkata, India.
Email: [email protected]
Received: January 19, 2018;
Initial review: February 15, 2018;
Accepted: July 13, 2018.
|
Objective: To determine efficacy of Point-of-care
Quality improvement (POCQI) in early initiation (within 30 minutes) of
emergency treatment among sick neonates.
Design: Quality improvement project over a period
of twenty weeks.
Setting: Special Newborn Care Unit (SNCU) of a
tertiary care center of Eastern India.
Participants: All consecutive sick neonates ( ³
28 wk gestation) who presented at triage during morning shift (8 am to 2
pm).
Intervention: We used a stepwise
Plan-do-study-act (PDSA) approach to initiate treatment within 30 min of
receiving sick newborns. After baseline phase of one month, a quality
improvement (QI) team was formed and conducted three PDSA cycles (PDSA I
, PDSA II and PDSA III) of 10 d each, followed by a post-intervention
phase over 3 months.
Main outcome measure(s): Percentage of sick
babies getting early emergency management at SNCU triage.
Results: 309 neonates were enrolled in the study
(56 in baseline phase, 88 in implementation phase and 212 in post-
intervention phase). Demographic characteristics including birthweight
and gestational age were comparable among baseline and post intervention
cohorts. During implementation phase, successful early initiation of
management was noted among 47%, 69% and 80% neonates following PDSA I,
PDSA II and PDSA III, respectively. In comparison to baseline phase, the
percentage of neonates receiving treatment within 30 minutes of arrival
at triage increased from 20% to 76% (P<0.001) and the mean (SD)
time of initiation of treatment decreased from 80.8 (21.0) to 19.8 (5.6)
min (P<0.001) during post-implementation phase. Hospital
mortality (33% vs 15%, P=0.004) and need for ventilator
support (44% vs 18%, P<0.001) were also significantly
lower among post intervention cohort in comparison to baseline cohort.
Conclusion: Stepwise implementation of PDSA
cycles significantly increased the percentage of sick newborns receiving
early emergency management at the SNCU triage, thereby resulting in
better survival.
Keywords: Outcome, PDSA cycle, Point-of-care Quality
improvement, Triage.
|
|
P
erinatal and neonatal care have improved
remarkably over last few decades, resulting in substantial decrease in
national neonatal mortality rate; although, as per India Newborn Action
Plan, our goal is to achieve single digit neonatal mortality rate by
2030 [1,2]. This entails addressing the major causes of neonatal
mortality including cost effective strategy to solve the problems [3].
We detected various lacunae within our system (reducing delay in
emergency management of sick babies, ensuring early initiation of breast
feeding, reducing sepsis, ensuring KMC in eligible babies) which can be
addressed to reduce neonatal death.
Existing literature revealed that delay in emergency
treatment of sick neonates may increase the risk of mortality and long
term morbidities [4,5]. We also noticed that outborn babies referred
from distant places are more vulnerable to death in comparison to inborn
babies. These neonates were already compromised during the time of
referral. Even after reaching at referral centre, these already
compromised out born babies suffer further delay in initiating emergency
treatment due to various administrative and procedural reasons. A
relevant prospective cohort study observed similar findings and
documented that hourly delay in initiation of appropriate resuscitation
or persistence of hemodynamic abnormalities was associated with a
statistically significant increased risk of death among sick neonates
[4]. Based on this literature review, we planned to undertake a quality
improvement (QI) initiative to reduce the time of initiation of
management of neonates presenting to triage with emergency signs. We
prioritized reducing delay in emergency management of sick babies,
because it is important to patient outcomes, affordable in terms of time
and resources, easy to measure and under control of team members.
Methods
All consecutive sick neonates presenting at the
triage area during morning shift (8 AM to 2 PM) of a tertiary-care
medical center between February and June 2017, were approached for
enrolment. Neonates attending triage seeking emergency management during
the month of February 2017 formed baseline cohort; those during March
2017 formed implementation cohort; and those between April and June 2017
formed post-intervention cohort. Neonates with major congenital
malformations, neonates of <28 weeks of gestation and who expired
shortly (within thirty minutes) after receiving in the triage area were
excluded (Web Fig. 1). We defined a neonate as sick if
presenting with any of the emergency signs: Significant hypothermia (axillary
temperature < 35.5 ºC), apnea
or gasping respiration, severe respiratory distress [rate >70, severe
retraction (subcostal, intercostals and supraclavicular and suprasternal
retraction), grunt], central cyanosis, shock (cold periphery, Capillary
filling time >3s, heart rate >160/min) coma, convulsions or
encephalopathy [6]. The study was approved by the Institutional Review
Board of our institute and informed written consent was obtained from
parents of each enrolled neonate.
According to POCQI module [7] quality improvement
team comprised of total nine members (a team leader, one supervisor, an
analyser, two time keeper and communicator and four nursing staffs)
including two faculty members was formed. The team reviewed the
literature on evidence based practices for emergency management, and
presented the recommendations informally which were then agreed upon or
modified for local implementation.
Baseline phase and Root cause analysis: A
time keeper and communicator, who were not involved in managing the sick
neonate, were commissioned as observer to note the practices and the
time of initiation of emergency management by using stop watch in
triage. The doctors and the nursing staffs involved in management
received no feedback about the time of initiation of management of sick
neonates. During baseline phase, 20% (56) sick neonates attended SNCU
triage received treatment within 30 minutes and median time to initiate
emergency treatment was 80 minutes (60 to 104 minutes)
(Web Fig. 2).
We performed a cause and effect analysis of delay in
emergency care using process flow chart (Web Fig. 3),
fishbone diagram (Web Fig. 4) and a key driver diagram (Web
Fig. 4). While analyzing the existing process flow chart, used
at our SNCU triage, we found that maximum delay occurs during receiving
the baby, examining by the on duty doctors and execution of advice by
the nursing staff (Web Fig. 3). We found following
lacunae; there was no assigned doctor and nurse in triage area, no
measurement of time by using stopwatch, no separate emergency tray in
triage, lack of urgency, no written policy, and lack of positive
attitude.
The aim of the study thus was to initiate early
(within 30 min) emergency management of sick neonates at triage of SNCU
from baseline 20% to at least 80% over a period of eight weeks of
baseline and implementation phase (February-March, 2017).
Implementation phase: We tested change ideas,
studied and acted upon these change ideas to achieve our aim. Three
Plan-Do-Study-Act (PDSA) cycles, each for ten days, were conducted in
morning shift (8 AM to 2 PM). During PDSA 1, doctors and nurses of
morning shift were assigned by preparing a separate triage roster and
designated them by using triage sticker. Throughout PDSA 2, we arranged
a separate emergency tray in triage by using check list. During PDSA 3,
we arranged training of doctors and nurses about POCQI module and
emergency triage assessment and treatment (ETAT); and displayed the
treatment protocol in triage [6-9]. During the implementation phase, a
corrected process flow chart was used (Web Fig. 5).
Balancing measure was overcrowding at triage area. Frequent feedback
with run charts of percentage of babies receiving emergency treatment
within 30 minutes and appraisal in weekly meetings were done to motivate
stakeholders and encourage compliance.
Post-intervention phase: Between April and June
2017, the QI team encouraged the implementation of the change ideas of
early initiation of emergency management, continued to monitor the
percentage of sick neonates receiving treatment within 30 minutes with
run chart and provided feedback to the treating residents and nursing
staffs. To identify opportunities for process improvement, the QI team
continued to meet with clinical teams weekly, audited cases of delayed
management and addressed logistic issues related to supplies and
equipment.
Pertinent maternal and neonatal data were documented
in case record forms. The time gap between the arrival of a sick neonate
in the triage and initiation of treatment was noted using a stop watch.
The primary outcome was percentage of sick babies getting emergency
early management at SNCU triage. Secondary outcomes were hospital
mortality, requirement of mechanical and non-invasive respiratory
support and requirement of ionotropic support.
Statistical analysis: Statistical analysis
was done by using SPSS for Windows version 16 software (SPSS Inc.,
Chicago, Illinois). Between groups, data for continuous variables were
evaluated using a t test for independent variables. Comparisons
of proportions were made using Chi-square testing.
Results
Among total 390 sick neonates, 356 were enrolled (56
in baseline phase, 88 in implementation phase and 212 in post
intervention phase) in this study (Web Fig. 1).
Demographic characteristics were comparable among baseline and post
intervention cohorts (Table I).
TABLE I Demographic Characteristics of Neonates Enrolled in the Study
|
Characteristics |
Baseline |
Implemen- |
Post inter- |
|
(n=56) |
tation Phase |
vention Phase |
|
|
(n=88) |
(n=212) |
|
Maternal characteristics |
|
*Maternal age, y |
28 (3) |
27 (5) |
28 (4) |
|
Preterm delivery |
18 (33.3) |
35 (39.7) |
98 (46.2) |
|
#Risk factors |
0 |
5 (5.7) |
13 (6.1) |
|
Maternal hypertension |
12 (22.2) |
14 (16) |
26 (12.3) |
|
Maternal diabetes |
6 (11) |
7 (8) |
19 (9) |
|
Vaginal delivery |
37 (66.6) |
52 (59) |
125 (59) |
|
Neonatal characteristics |
|
#Gestational age (wk) |
36 (1.3) |
37 (1.2) |
36 (1.6) |
|
#Birthweight (g) |
2312 (180) |
2380 (208) |
2346 (160) |
|
Male gender |
31 (55.5) |
56 (63.6) |
137 (64.6) |
|
AGA |
43 (77.7) |
53 (60.2) |
155 (73.7) |
|
SGA |
12 (22.2) |
33 (37.5) |
52 (24.5) |
|
LGA |
1 (0.1) |
2 (2.3%) |
5 (2.4) |
|
Significant hypothermia |
24 (44.4) |
17 (19.3) |
84 (40.7) |
|
Apnea/gasping |
18 (33.3) |
56 (63.6) |
82 (39) |
|
Severe respiratory distress |
20 (36) |
33 (37.5) |
87 (41) |
|
Central cyanosis |
5 (0.08) |
4 (4) |
59 (2.8) |
|
Shock |
12 (22.2) |
47 (53.4) |
88 (41.5) |
|
Convulsions/coma/encephalopathy |
18 (33.3) |
58 (66) |
80 (38.5) |
|
Data expressed in n(%); *mean (SD) and #median (IQR); AGA
(appropriate for gestational age); SGA (small for gestational
age); LGA (large for gestational age); #Risk factors for early
onset sepsis include: very low birth weight (<1500 g),
prematurity, prolonged rupture of membranes(>24 h), foul
smelling liquor, multiple (>3) per vaginum examinations in 24 h,
intrapartum maternal fever (>37.8ºC). |
 |
|
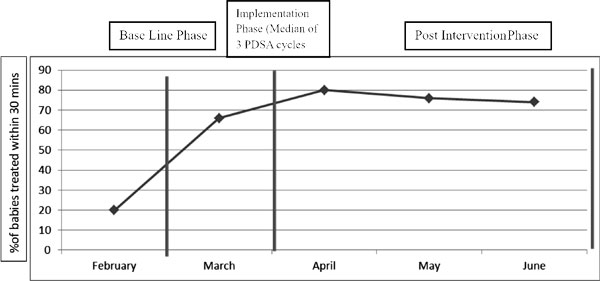
Fig. 1 Percentage of neonates
treated within 30 minutes in baseline phase, implementation
phase and in the post intervention phase.
|
During implementation phase, we registered successful
early initiation of management among 47%, 69% and 80% of sick neonates
following PDSA 1, PDSA 2 and PDSA 3, respectively (Web
Fig. 6). Throughout the time of post implementation
phase, 80%,76% and 74% of sick neonates received early emergency
treatment during each month of April, May and June of 2017,
respectively. (Fig. 1). In comparison to baseline
phase, the percentage of neonates receiving treatment within 30 minutes
of arrival at triage increased from 20% to 76% (P<0.001) and the
mean time of initiation of treatment decreased from 80.8 (20.9) to 19.8
(5.6) minutes (P<0.001) during post-implementation phase (Fig.
1 and Table II). Hospital mortality (33 vs 15%,
P=0.004) and need for ventilator support (44 vs 18%, P<0.001)
were also significantly lower among post- intervention cohort in
comparison to baseline cohort (Fig. 1 and Table
II). There was substantial improvement in early emergency management
during evening and night shift (42% and 33%, respectively) without
implementing PDSA cycles (Web Fig. 7).
TABLE II Outcome of Sick Neonates Enrolled in Baseline and Post-intervention Phase
|
Characteristics |
Baseline phase |
Post-intervention |
Odds ratio/ Mean |
P value |
|
(n=56) |
phase (n=212) |
difference (95% CI) |
|
|
Neonates treated within 30 min |
11 (20) |
161 (76) |
12.91(6.21-26.81) |
<0.001 |
|
Time of initiation of treatment* |
80.8 (20.96) |
19.8 (5.6) |
-61.0 (-64.18 - -57.8) |
<0.001 |
|
Hospital mortality |
18 (33.3) |
32 (15) |
0.37 (0.19-0.73) |
0.004 |
|
Total hospital stay (d)# |
16 (10-24) |
12 (8-22) |
– |
– |
|
Need for ventilator support |
24 (44.4) |
38 (18) |
0.29 (0.15-0.54) |
<0.001 |
|
Duration of ventilator support (d)# |
4 (2-6) |
3 (2-5) |
– |
– |
|
Need for ionotropic support |
18 (33.3) |
35 (16.5) |
0.41 (0.21-0.81) |
0.01 |
|
Need for >1 ionotropes |
12 (22.2) |
29 (13.6) |
0.58 (0.27-1.22) |
0.15 |
|
Values in No. (%), #Median (interquartile range)
or *mean (SD). |
Discussion
This QI effort was a stepwise introduction of
measures to initiate emergency management of sick neonates within 30
minutes driven by PDSA cycles. We showed improvement in mean time of
initiation of treatment, without crowding in the triage area which was
our key balancing measure. The mean time decreased by 60 minutes and the
percentage of neonates received treatment within 30 minutes increased
from 20% to 80%. This improvement was sustained throughout the
post-intervention phase.
Han, et al. [4] conducted a nine-year
retrospective cohort study of 91 infants and children who presented to
local community hospitals with septic shock and required transport to
central referral centre. They showed that when community physicians had
implemented therapies that resulted in successful shock reversal (within
a median time of 75 minutes), almost all of the infants and children
presenting with septic shock survived. That each hour of delay in
resuscitation was associated with a 50% increased odds of mortality.
Rivers, et al. [5] showed that implementation of early
goal-directed therapies in the emergency department, improved survival
outcomes in adult septic shock significantly. Study by investigators in
London also found that avoidable delays and inappropriate management
contributed to poor outcome among children with severe meningococcal
disease [10].
Booy, et al. [11] described a remarkable
improvement in outcome of meningococcal disease by dissemination of
recommended guidelines for managing meningococcal disease to area
community hospitals through educational outreach programs, facilitation
of early communication and management recommendations between the local
and referral hospital, and utilization of a mobile pediatric critical
care transport team. By implementing these change ideas there was an
impressive reduction of mortality from meningococcal disease in Southern
England from 23% to 2% in a span of just 6 years [11].
In our study, we implemented some simple measures in
a stepwise manner through PDSA cycles as per POCQI module [7]. Each PDSA
cycle helped us to test small interventions leading to valuable learning
and refinement of neonatal emergency management. Moreover, clinical team
was motivated with prominent display of run charts which served as an
instant display of outcome. This enabled team ownership, enthusiasm,
participation and an opportunity to improve. The percentage of babies
receiving early emergency management were increased remarkably in
evening and night shifts, though we did not assign any dedicated doctor
and nursing staff for triage in these shifts. Secondary outcomes like
in-hospital mortality, need for mechanical ventilation, and need for
ionotropic support also decreased significantly.
Our study has several limitations. Firstly, being a
single-center study, all the interventions implemented by us may not be
generalizable to other settings. Moreover due to lack of human resources
we were not able to assign nursing staff and doctors separately for
triage in evening and night shift. Secondary outcomes like mortality is
affected by a numerous factors other than delay in initiation of
treatment, we did not study those factors. Hence, to further establish
our study findings, further research is necessary with large sample size
incorporating all factors.
We decided to share our study findings with
appropriate authorities to motivate them and to ensure further logistic
support and human resources to implement these change ideas in other
shifts and health delivery facilities. Stepwise successful
implementation of PDSA cycles significantly increased the percentages of
sick newborns received early emergency management at SNCU triage and
thereby resulting in better survival among them. However, larger trial
over longer duration with continued surveillance is required to confirm
this fact.
Acknowledgement: D. TKS Mahapatra, NRS Medical
College, Kolkata; Dr VK. Paul, Member NITI Aayog, Government of India; Dr
Ashok Deorari, AIIMS, New Delhi and his team; and
Dr Deepak Chawla, Government Medical College and Hospital, Chandigarh
for their logistic support to complete this project successfully.
Contributors: AM and MB contributed equally to
this study. AM: study design and execution, preparation of manuscript
and critical review; MB, BM, SM, BA: study design and execution, data
collection and analysis, preparation of manuscript; BB: data analysis,
preparation of manuscript and critical review. All authors agreed and
approved the final version and vouch for the accuracy of the submitted
manuscript.
Funding: None; Competing interest:
None stated.
|
What is Already Known?
• Early initiation of emergency management at
triage reduces complications and mortality among sick neonates.
What This Study Adds?
• A quality improvement initiative focusing
on stepwise successful implementation of PDSA cycles
significantly increased the number of sick newborns receiving
early emergency management at SNCU triage, thereby resulting in
better survival.
|
References
1. West Bengal- WB Health.Vital Statistics. Available
from: https://www.wbhealth.gov.in/other_files/Health%20on%
20the%20March,%202015-2016.pdf Accessed February 24, 2018.
2. INAP-WHO Newborn CC. Available from:
https://www.newbornwhocc.org/INAP_Final.pdf. Accessed February 23,
2018.
3. Neonatal Health – Unicef India. Available from:
http:unicef.in/Whatwedo/2/Neonatal-Health. Accessed February 24,
2018.
4. Han YY, Carcillo JA, Dragotta MA, Bills DM, Watson
RS, Westerman ME, et al. Early reversal of pediatric-neonatal
septic shock by community physicians is associated with improved
outcome. Pediatrics. 2003;112:793-9.
5. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin
A, Knoblich B, et al. Early goal-directed therapy in the
treatment of severe sepsis and septic shock. N Engl J
Med. 2001;345:1368-77.
6. Family Health Bureau, Ministry of Health, Sri
Lanka. National Guidelines for Newborn Care. Volume iii. Available from:
http://fhb.health.gov.lk/web/index.php? optio=co_phocadownload&view=category&
download=
674:national-guidelines-for-newborncare-volume-111-pdf&id=10:intranatal-newborn-care&lang=en.
Accessed February 19, 2018.
7. POCQI –Learner Manual - WHO newborn CC. Available
from: https://www.newbornwhocc.org/POCQI-Learner-Manual.pdf..
Accessed February 19, 2018.
8. Clinical Protocols 2014- WHO newborn CC. Available
from: http://www.newbornwhocc.org/clinical_proto.html. Accessed
February 19, 2018.
9. National Neonatology Forum. NNF Guidelines 2011.
Clinical Practice Guidelines. New Delhi: National National Forum;
October, 2010.
10. Nadel S, Britto J, Booy R, Maconochie I, Habibi
P, Levin M. Avoidable deficiencies in the delivery of health care to
children with meningococcal disease. J Accid Emerg Med. 1998;15:298-03.
11. Booy R, Habibi P, Nadel S, de Munter C, Britto
J, Morrison A, et al. Reduction in case fatality rate from
meningococcal disease associated with improved healthcare delivery. Arch
Dis Child. 2001;85:386-90.
|
|
|
 |
|

