angaroo mother care (KMC) is an evidence-based
cost effective approach, and can avert up to 450,000 preterm deaths each
year if near-universal coverage is achieved [1,2]. Invest-ment in KMC
has benefits beyond survival including healthy growth and long term
development [3,4].
However, despite its known benefits, the adoption and
implementation of KMC has been low. Even at the places where KMC is
being practiced in the facility, the number of hours of KMC remain low.
Average duration of KMC varies from 3-5 h/day in previous Indian studies
[5,6]. Various potential barriers to KMC include issues with facility
resources and environment, negative impressions about staff attitude,
and lack of awareness about KMC benefits [7].
A recent study in our unit reported median (IQR) KMC
duration in eligible preterm infants of 3.14 (2.1-4.3) h/day. To address
this problem we used QI approach to target the bottle neck areas in a
step-wise manner. We formulated an aim statement to increase the
duration of KMC per day from a current baseline of 3 hours to 6 hours in
admitted eligible preterm mother- infant dyads.
Methods
Our hospital has a 10-bedded level III and a
20-bedded level II NICU in addition to 8 Kangaroo mother care and
rooming-in beds. Each eligible mother-infant dyad was a single
participant in the present study. All eligible preterm neonate admitted
in NICU were included. Sick neonates [defined as those requiring
invasive or non-invasive mechanical ventilation (NIMV) or shock (defined
as the presence of tachycardia (heart rate more than 180 beats/minute,
extremities cold to touch, and capillary fill time more than 3 seconds,
with or without pallor, lethargy or unconsciousness) or apnea (>4 apneas
in the last 24 h)], neonates receiving phototherapy, and for whom no
eligible relatives were available and/or the mother was sick or
discharged from the hospital were excluded.
A team comprising one faculty in-charge, one resident
physician, one nurse educator and two senior staff nurses was formed to
evaluate the barriers for improved KMC duration and to plan the
subsequent steps for promoting the same.
In baseline phase, data was collected in a
predesigned proforma for 10 days for ten eligible preterm infant-mother
dyads. We tried to evaluate various barriers faced by mother as well as
staff members for providing KMC of pre-specified duration by using
another proforma. The barriers were identified using fish bone analysis
(Web Fig. 1). The predominant barriers were
lack of adequate support to mother, absence of formal counselling on KMC
by the healthcare team, and other maternal factors including lack of
privacy, stress and fatigue. On one-to-one discussion with the mothers,
the authors found that they were spending nearly 5 hours of the day for
expression of breast milk and almost a similar duration for feeding the
baby (total 10 hours), and no KMC was being practiced during the night
hours.
A comprehensive KMC improvement package was planned.
This consisted of two main elements: one was education and sensitization
of health care providers and family members and secondly, a simultaneous
reinforcement of ongoing practice. We took some corrective steps which
included felicitation for both relatives as well as staff-nurses. These
changes were tested as a part of Plan-Do-Study-Act (PDSA) cycle. We
conducted three PDSA cycles (Web Table I).
A combined meeting of the nurse-educator, team leader
nurses, other staff nurses, and resident doctors was conducted every
week in the implementation phase for apprising every one of the current
situation. For sustenance of the improvement initiative, the combined
meeting was conducted on a monthly basis and the results were collected
on an ongoing basis and reviewed fortnightly, and continuous feedback to
given to all staff.
The primary outcome measure was the duration of KMC.
This was evaluated by staff nurse on duty by recording the exact hours
of KMC in each 8-hour shift and then adding total duration of 3
shifts/day) in eligible preterm infant-mother dyads. The duration was
then plotted on a run-chart. The outcome was evaluated daily in
implementation phase, and one day every fortnight in post-implementation
phase.
Data analysis: The data was coded and analyzed
statistically using STATA version 11.1 (Stata Corp, College station,
Texas, US). A P value of <0.05 was taken as significant.
Results
The baseline demographic characteristics of mother as
well as preterm infant were similar in both the phases (Baseline phase
and implementation phase) (Table I). The biggest barrier
to successful implementation of KMC was absence of formal KMC
counselling for the mothers and family members. We hypothesized that
educating them regarding benefit of KMC would be useful.
TABLE I Baseline Characteristics of Participants
Parameter
|
Baseline phase
(n=10) |
Implementation phase
(n=20) |
|
Maternal age, y |
29.4 (5.1) |
30.3 (4.1) |
|
Gestational age, wks |
30.9 (6.2) |
31.1 (2.3) |
|
Birthweight, g |
1359 (305) |
1199 (356) |
|
Primipara mother* |
5 (50) |
19 (95) |
|
Mother’s education#
|
7 (70) |
14 (70) |
|
Males |
6 (60) |
8 (40) |
|
GA<32 wk |
4 (40) |
7 (35) |
|
Small for GA |
5 (50) |
7 (35) |
|
Need for resucitation |
2 (20) |
6 (30) |
|
Data expressed as number (%) or mean (SD); *P<0.001;
#Graduate or above. |
As a part of PDSA Cycle 1 (first two weeks), four
nursing staff working in NICU in different shifts were identified and
were involved in comprehensive counselling and on KMC for the mothers
and their family members. This included creation of supportive
environment in NICU for KMC, and showing them videos and pictorial
charts on KMC in small groups. One-to-one counselling of mother and
family members on KMC and its benefits was done by the assigned bedside
nurse. Encouragement and acknowledgment of mothers and family members
for increasing the duration of KMC was done by the nurses. The mean
duration of KMC increased from 3.25 hours to 4.5 hours by the end of
first PDSA cycle (Web Fig. 2). The resident
doctors included emphasis of KMC duration as a part of daily treatment
order.
In PDSA Cycle 2 (3/font>rd
and 4th week) the overall
target of 6 hours was split as ensuring at least 2 hours in each shift
by the respective nursing staff. The staff nurses were felicitated for
ensuring maximum KMC hours in their shifts on weekly basis in periodic
meetings. We also ensured availability of more breast-pumps (total
number of electronic breast pumps was increased from 2 to 4) which
resulted in decrease in waiting time for mother’s expression of milk
with breast pumps. The average duration of KMC increased to more than 6
hours (at the end of 4th week). During the 5th week of the project the
mean duration of KMC declined slightly. This was postulated due to lack
of active participation of infants in KMC who were in respiratory
support. So in PDSA Cycle 3, the assigned nurses were made available
round the clock with babies and mothers/family members at the time of
KMC, especially who were on some kind of respiratory support like oxygen
therapy and non-invasive ventilation to build up their confidence and
alleviate anxiety and fear related to baby’s desaturation at the time of
KMC. Nurses provided constant positive re-enforcement and encouragement
to the mothers and the family members for doing KMC. At the end of 7
weeks, average number of hours of KMC increased from 4.1 to 7.2 hours.
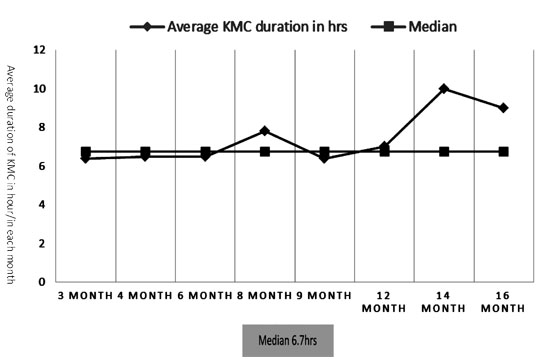
We were able to sustain improved average KMC duration
in the unit in post-implementation phase, even after 1 year of
completion of QI project. Fathers and other close family members are
allowed to give KMC in the unit even at night time, so that mothers can
get rest. Even after one year of implementation of study, the duration
of KMC among all eligible babies remains around 9 h/day (Fig.
1).
 |
|
Fig. 1 Sustenance of KMC in
post-implementation phase.
|
One of the balancing outcomes which the QI team found
during the study process was an increase in the breakage of temperature
probes of radiant warmer due to excessive dragging of probes while
babies were transferred from radiant warmer to caregiver for initiation
of KMC. However, this was subsequently sorted out by careful detachment
of probes from radiant warmer side by staff nurses each time KMC was
started for a baby.
Discussion
Maternal lack of time and supportive environment and
fatigue were the main barriers for practice of optimum KMC [7]. Hence,
allowing other family members for KMC addressed these issues. Active
involvement of family members not only scales- up facility based KMC,
but it is also known to sustain home-based KMC after discharge [8].
Although increasing staff support and implementing
temporary project staff is known to scale up KMC practices, the effect
seems transient and fades with withdrawal of support [8,9]. A unique
effort in our study was the utilization of existing resources and
infrastructure for strengthening KMC.
Audit-and-feedback is considered as one of the
backbones of quality improvement initiative for changing healthworker
behavior as well as an ongoing policy which formed an important
milestone in our study. We conducted weekly audit in our study to
evaluate the potential reasons for decreased KMC duration. In addition,
the concept of weekly declaration of champions encouraged the healthcare
providers. Similar role of healthcare champions has been described in
recent studies from Western India [5].
Our study was a single-center quality improvement
initiative. The limitation of the study was that the morbidity data was
not evaluated. The data on day of KMC initiation, details on KMC
continuation after discharge for each baby was not prospectively
collected. Mothers were not comfortable doing KMC while they were
walking or eating. Similarly the idea of pumping of both breasts
simultaneously to save time were not adopted by our mothers. We hence
resorted to active involvement of other family members for facilitating
KMC. Although we could reach our target of 6 hours as planned for this
initiative, this is still low as per the WHO standard. However, we feel
that with continuation of education in post-implementation phase further
improvement is expected.
We demonstrated feasibility and sustainability of a
simple quality improvement approach for increasing KMC duration in
eligible preterm neonates. This was achieved within existing resources
without addition of extra manpower by involving family members.

