|
|
|
Indian Pediatr 2018;55: 739-743 |
 |
Impact of Quality Improvement Program on
Expressed Breastmilk Usage in Very Low Birth Weight Infants
|
|
Anup Thakur 1,
Neelam Kler1,
Pankaj Garg1,
Anita Singh2 and
Priya Gandhi1
From 1Department of Neonatology, Institute
of Child health, Sir Ganga Ram Hospital, Rajinder Nagar, New Delhi; and
2Department of Neonatology, Sanjay Gandhi Postgraduate
Institute of Medical Sciences, Lucknow, Uttar Pradesh, India.
Correspondence to: Dr Anup Thakur, Consultant
Neonatologist, Institute of Child health,
Sir Ganga Ram Hospital, New Delhi, India.
Email: [email protected]
Received: January 27, 2017;
Initial review: May 29, 2017;
Accepted: July 12, 2018.
|
|
Objective: To improve the usage
of expressed breast milk in very low birth weight infants admitted in
the neonatal intensive care unit of a tertiary centre in India.
Methods: Between April 2015 and
August 2016, various Plan-do-act-study cycles were conducted to test
change ideas like antenatal counselling including help of brochure and
video, post-natal telephonic reminders within 4-6 hours of birth,
standardization of Kangaroo mother care, and non-nutritive sucking
protocol. Data was analyzed using statistical process control charts.
Results: 156 very low birth
weight infants were delivered during the study period, of which 31 were
excluded due to various reasons. Within 6 months of implementation, the
proportion of very low birth weight infants who received expressed
breast milk within 48 hours improved to 100% from 38.7% and this was
sustained at 100% for next 8 months. The mean time of availability and
volume of expressed breast milk within 48 hours, improved gradually from
73.3 h to 20.9 h and 4.7 mL to 15.8 mL, respectively. The mean
proportion of expressed breast milk once infant reached a feed volume of
100 mL/kg/day also improved from 61.3% to 82.3%.
Conclusion: Quality improvement
interventions showed promising results of increased expressed breast
milk usage in very low birth weight infants.
Keywords: Antenatal counselling,
Breastfeeding, Care bundle, PDSA cycle.
|
|
H
uman milk has immunerable benefits for infants,
especially very low birth weight (VLBW) infants [1]. Recent evidence
implicate that prematurity related morbidities are closely related to
specific critical periods following birth, during which the use of human
milk may be most important. In addition, the dose and exposure period of
human milk appears critical to confer its benefits [2]. Four
well-controlled studies in premature infants have linked the dose of
human milk (mL/kg/d) received throughout the Neonatal Intensive Care
Unit (NICU) stay with specific health outcomes during or after NICU stay
[3-6]. However, the usage of human milk in VLBW infants varies globally
and human milk banks are not widely available, especially in resource
limited settings. In such a scenario when donor human milk feeding is
not available, the only feasible option available to clinicians for
optimum nutrition of preterm infants is to make mothers own milk
available. Quality improvement (QI) programs through altered clinical
behavior and by delivering consistent good practice can improve usage of
human milk and therefore improve health outcomes of preterm infants [7].
Interventions such as antenatal consults, lactation counselling,
tracking motherís milk supply, staff education, and other evidence-based
bundles have been used to improve usage of human milk [8-13]. However,
no QI initiatives have been reported from India focussing on EBM usage
in VLBW infants.
In our unit, the usage of expressed breast milk (EBM)
in VLBW infants was low, and the proportion of EBM usage of total feeds
was only 52% [14], and the availability of first EBM after birth was
often delayed for days. This prompted us to start a QI program in our
hospital in collaboration with Institute of Healthcare Improvement
(IHI), Massachusetts and ACCESS health International, India with an
objective to improve usage of EBM in VLBW infants. The specific goals of
the project were to obtain EBM in >80% of VLBW infants within 48 hours
of admission to the NICU, improve volume of EBM obtained in first 48
hours (by 100%), to decrease the time of availability of first EBM by
20% of baseline and to improve proportion of EBM volume usage by more
than 20% of baseline.
Methods
The project was carried out in a tertiary-care center
with level III B NICU in India from April 2015 to August 2016. The
institute does not have a human milk bank and enteral feeding depends on
availability of motherís own milk; in case of unavailability of motherís
own milk, preterm formula is used. This project involved the systematic
implementation of evidence-based practices utilizing QI strategies and
thus did not require Institutional Review Board approval.
Data on all inborn infants with a birth weight of
£1500 g
admitted to the NICU were included. Driver diagram (Web Fig. 1)
was developed after internal discussions. The nature of intervention was
chalked out by a multi-disciplinary QI team. It consisted of two
consultant neonatologists, two neonatology residents, a dedicated
lactation counsellor, nurse in charge of NICU and delivery room, four
senior NICU nurse with extensive feeding expertise, two improvement
experts, and one project manager. This team underwent extensive
brainstorming sessions and performed the root cause analysis of less
usage of EBM in NICU (Web Fig. 2.). The QI team then
developed the Care bundles based on evidence based practices distilled
from literature search, and agreed upon or modified them for local
implementation. A summary of the components of the care bundle is
provided in Web Table I. The care bundle consisted of two
elements: promotion of early milk expression and ongoing support for
lactation and stress management.
In the first phase of the project, from April to June
2015, change ideas were tested by repeated PDSA cycles. Change ideas
were modified or discarded based on PDSA ramps. In the first PDSA ramp (Web
Fig. 3), the change idea of antenatal counselling was developed
and tested. Initially antenatal counselling was done in two cases at
random and EBM was not available in the first 48 hours in either of
them. This idea was discarded. In the second cycle, we developed and
tested a standardized format for antenatal counselling in three cases
and EBM within 48 hours was available in two of these. The mother who
failed to send EBM to the NICU gave the feedback that she forgot about
sending EBM. In the third cycle, we added the change idea of giving
telephonic reminders to the mother within 6 hours of delivery. We tested
these in another four cases and could get EBM within the stipulated time
in all cases. In the second phase from mid-June 2015, implementation of
these tested change ideas was started while ongoing PDSA were being
conducted. The QI team received a feedback from the mothers that a
pictorial illustration would help them better to pump EBM, so a brochure
and posters were developed and tested in the fourth cycle in July
2015.In the fifth cycle, we added on the change idea of showing videos
to mothers during antenatal counselling sessions. The completed PDSA
ramp 1 was implemented in August 2015. Similar to PDSA ramp 1, PDSA ramp
2 constituted of three consecutive PDSA cycles of developing and testing
a standardized KMC and NNS protocol followed by its implementation in
late August 2015. PDSA ramp 3 constituted of three consecutive PDSA
cycles in August to develop and test list-based tracking of mothers.
PDSA ramp 4 consisted of another three cycles of daily data entry of EBM
status in weight book by nurses, integration of data in excel sheet by
residents, followed by Excel-based daily counselling by consultants
before it was implemented in September 2015. PDSA ramp 5 consisted of
two PDSA cycles on change idea of fortnightly video-based group
counselling sessions of mothers in the NICU. PDSA ramp 6 was run in
December 2015 and in a planned experimentation design, change ideas of
daily team huddle, text messaging and admission brochure were tested.
The improvement activities are described in
Web
Box 1.
Process and Outcome Measures: The process
measures studied monthly were proportion of mothers counselled ante-natally
or post-natally for expression of breast milk and proportion of eligible
VLBW infants who received Kangaroo mother care and non-nutritive
sucking. The outcomes measures that were evaluated monthly for infants
born £1500 g
birth weight were percentage of infants who received EBM within first 48
hours of birth, time of availability of first EBM, volume of EBM
available in first 48 hours, and volume of EBM vs formula (in %)
once infant reached a feed volume of 100 mL/kg/day. The balancing
measure was proportion of normal term infants discharged on total breast
feeds.
Baseline data of each eligible infant from February
2015 to April 2015 was collected retrospectively from infantís daily
milk record. Following April 2015, after initiation of IA program all
data was collected prospectively.
Data analysis: Data were analyzed using QI
charts software. Statistical process control charts called Shewhartís
charts were used in our project to evaluate the effectiveness of
intervention over time [15-17]. The control limits on the charts (upper
and lower) establish the margins within which the measurement will be
found approximately 99% of the time. The observed change was considered
significant i.e. resulting from a special cause variation as per
rules for special cause [18]. P statistical process chart was used to
examine non-nutritive sucking, Kangaroo mother care, antenatal
counseling and percentage of VLBW infants who received EBM within first
48 hours of birth. X-bar chart was used to examine time of availability
of first EBM, volume of EBM available in first 48 hours and proportion
of EBM once infants reached a feed volume of at least 100 mL/kg/day.
Results
A total of 156 VLBW infants were delivered during the
study period, of which 31 were excluded from analysis as their mothers
required admission in ICU due to one of the postnatal complications like
seizure, shock or severe post-partum bleeding. One hundred and twenty
five eligible VLBW infants were finally included for analysis. The mean
(SD) gestational age and birth weights of the infants were 29.6 (2.6)
weeks and 1094 (243) g, respectively.
The proportion of mothers counselled ante-natally or
post-natally for expression of breast milk improved over time and was
sustained. The proportion of eligible infants who received Kangaroo
mother care and non-nutritive sucking remained above 90% in 12
consecutive data points (Web Fig. 4). Before
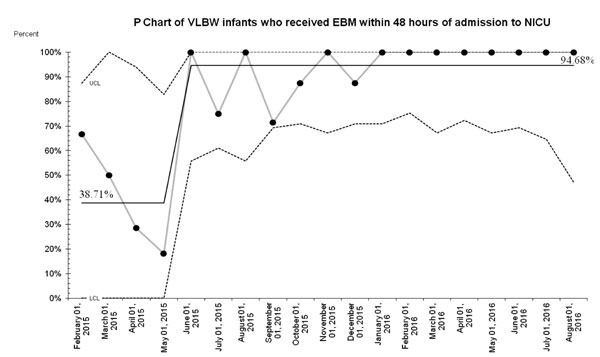
implementation of any component of care bundle, the proportion of VLBW
infants who received EBM within 48 hours of birth was 38.7%. Within 6
months of implementation, this improved to 100% and following the most
recent interventions, this was sustained at 100% for next 8 months (Fig.
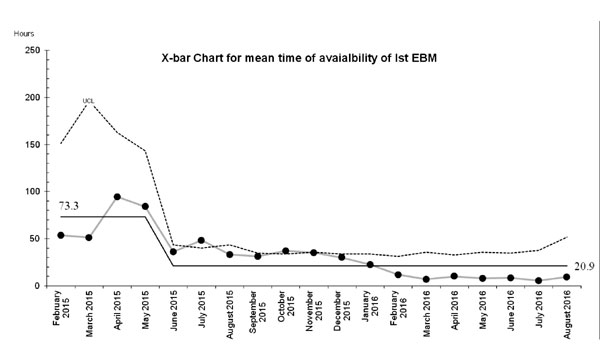
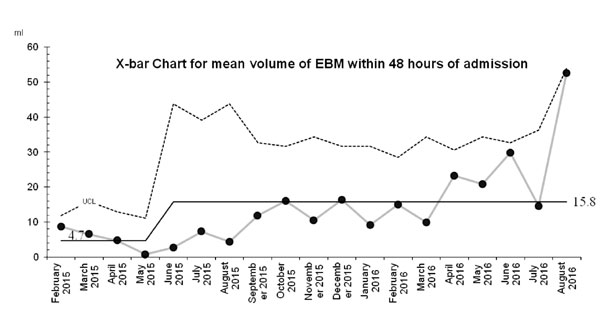
1a). The mean time of availability and mean volume of EBM within 48
h, before the implementation phase was 73.3 h and 4.7 mL, respectively.
After this phase, the mean time of availability of first EBM steadily
declined to 20.9 h and mean volume of EBM obtained within 48 h of birth
improved more than three folds to 15.8 mL (Fig. 1b, 2a).
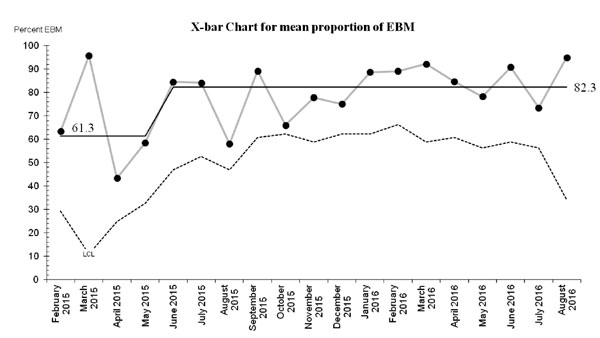
The mean proportion of EBM once infant reached a feed volume of 100 mL/kg/day
also improved from 61.3% to 82.3% (Fig. 2b). The balancing
measure-proportion of normal term infants discharged on total
breastfeeds did not show any significant change during the project.
 |
| (a) |
 |
| (b) |
|
Fig. 1 (a) P chart of VLBW
infants who received EBM within 48 hours of admission to NICU;
and (b) X-bar chart for mean time of availability of first
expressed breast milk (EBM).
|
 |
| (a) |
 |
| (b) |
|
Arrows denote points of implementation of
change ideas; June 2015-Antenatal counselling, reminders,
physical help by lactation counsellor; August 2015- KMC/NNS,
brochure/videos/postnatal daily counselling and list based
tracking; September 2015-excel sheet based daily counselling;
October 2015-video based counselling; December 2015-planned
experimentation including team huddle.
Fig. 2 (a) X-bar Charts for mean volume of
first expressed breast milk (EBM) within 48 hours of admission and
mean proportion of expressed breast milk (EBM).
|
Discussion
This quality improvement initiative resulted in
increase in proportion of VLBW infants who received EBM within first 48
hours of birth, decreased time of availability of first EBM, increased
volume of available EBM in first 48 hours and overall higher consumption
of EBM in VLBW infants.
Our results are consistent with other studies that
had used similar or different care bundles for achieving higher human
milk consumption in VLBW infants [8-13]. Sisk, et al. [8] in a
study evaluated the impact of lactation counselling on initiation of
milk expression and found that counselling mothers of VLBW infants
increases the incidence of lactation initiation and breastmilk feeding
without increasing maternal stress and anxiety. Murphy, et al.
[9] implemented similar interventions in addition to tracking of
motherís milk supply and physician education. The median time of first
maternal milk expression decreased significantly and there was
significant improvement in the proportion of infants receiving exclusive
motherís breast milk at 28 days and at discharge. Spatz, in 2004,
recommended 10 steps for promoting and protecting breastfeeding in
vulnerable infants [18-19].The steps involved various aspects of
lactation support including assisting the mother with the establishment
and maintenance of a milk supply, providing skin-to-skin care (Kangaroo
care) and opportunities for non-nutritive sucking at the breast, and
providing appropriate follow-up care. Fugate, et al. [20]
implemented the ten steps in a continuous quality improvement initiative
and achieved significant improvements in the percentages of mothers
expressing their milk within 6 hours of delivery, infants receiving
motherís own milk at initiation of feeds, and mothers with a
hospital-grade pump at discharge. The findings of QI initiative that we
conducted are similar to above published literature.
The care bundles that were used in our QI initiative
were tailor-made for our system and upscaled through multiple PDSA
cycles before implementation. The use of planned experimentations in
choosing some of the care bundles to improve EBM usage is unique to this
QI initiative. The outcome measure that improved quickly after
implementation was time of availability of first EBM. This happened
because the enthusiastic team members would initiate pumping mothersí
milk themselves as soon as motherís condition permitted. A dedicated
NICU lactation consultant and the NICU nursing team were key members of
the team. However, the volume of EBM and proportion of EBM of total
feeds not only depended on team memberís efforts but also on the
commitment of the mothers and physical as well as emotional state. When
the time of availability of first EBM consistently came down, we then
focussed on outcome measures of improving volume of EBM.
The strength of this QI project is that it represents
one of the first few published reports from India to demonstrate the
effectiveness of the systematic implementation of QI methods to improve
usage of human milk in very low birth weight infants. We used a
dedicated lactation consultant to lead the QI improvement project.
Nonclinical duties were therefore delegated to ancillary personnel. The
improvement project has some limitations. First, the care bundles that
were tested in various PDSA cycles were implemented in groups rather
than as individual interventions. This potentially limits our ability to
link the interventions with the outcome. This also led us to describe
our results in two phases. Phase 1 was the initial phase of the project
which had some PDSA testing going on, while phase 2 had both
implementation and testing going on con-currently. In our project, as no
baseline data was available, historical data was used to create baseline
along with first few data points while the project was getting up and
running. This is crude but can be useful as chances are that the
processes have not been improved much during this start up time frame.
Secondly, the outcomes of our study could have been possibly confounded
due to constant supervision and monthly reporting of data to IHI from
April 2015 to March 2016 but the fact that the results of the study were
sustained even after this phase, possibly mitigates this bias. Thirdly,
our study was conducted in a level 3B NICU and the study sample was well
educated so counselling and implementation of other change ideas could
be easier than would be expected in a different set-up. So, some
interventions may need to be modified as per the population and local
set-up. In addition, although no additional manpower was employed for
this QI Project nor was it funded but a replication of similar results
may require a dedicated QI team that takes up additional responsibility
without compromising other aspects of clinical care unless the entire
process is integrated in the system and becomes a culture of the unit.
We conclude that by systematic application of QI
methods EBM usage of motherís own milk in VLBW infants can be
significantly improved and sustained. Further research should focus on
replicating these findings in different settings, further expanding the
benefits to all neonates admitted in NICU who require EBM and evaluating
the impact of increased EBM, usage on clinical outcomes such as sepsis,
necrotizing enterocolitis, mortality and long term neurodevelopment.
Acknowledgements: Institute of Healthcare
Improvement (IHI), Massachusetts and ACCESS health International, India
for providing training, supervision and feedback during the project.
Contributors: AT, NK: conceptualized the
project; AT: developed the protocol; AT, PRG: had primary responsibility
of patient screening, enrolment and data collection; AT: performed the
data analysis; AT: wrote the manuscript; NK, PG: participated in
protocol development, supervising enrolment, outcome assessment and in
writing the manuscript; AS: participated in planning of project and
writing of manuscript.
Funding: None; Competing interests: None
stated.
|
What This Study Adds?
ē QI program can be implemented and sustained
even in resource-limited settings to improve usage of human milk
in very low birth weight infants.
|
References
1. Henderson G, Anthony MY, McGuire W. Formula milk
versus maternal breast milk for feeding preterm or low birth weight
infants. Cochrane Database Syst Rev. 2007;17:CD002972.
2. Meier PP, Engstrom JL, Patel AL, Jegier BJ, Bruns
NE. Improving the use of human milk during and after the NICU stay. Clin
Perinatol. 2010;37:217-45.
3. Schanler RJ, Lau C, Hurst NM, Smith EOB.
Randomized trial of donor human milk versus preterm formula as
substitutes for mothersí own milk in the feeding of extremely premature
infants. Pediatrics. 2005;116:400-6.
4. Schanler RJ, Shulman RJ, Lau C. Feeding strategies
for premature infants: Beneficial outcomes of feeding fortified human
milk versus preterm formula. Pediatrics. 1999;103:1150-7.
5. Vohr BR, Poindexter BB, Dusick AM, McKinley LT,
Higgins RD, Langer JC, et al. Persistent beneficial effects of
breast milk ingested in the neonatal intensive care unit on
outcomes of extremely low birth weight infants at 30 months of
age. Pediatrics. 2007;120:e953-9.
6. Vohr BR, Poindexter BB, Dusick AM, McKinley LT,
Wright LL, Langer JC, et al. Beneficial effects of breast milk in
the neonatal intensive care unit on the developmental outcome of
extremely low birth weight infants at 18 months of age. Pediatrics.
2006;118:e115-23.
7. Battersby C, Santhakumaran S, Upton M, Radbone L,
Birch J, Modi N, et al. The impact of a regional care bundle on
maternal breast milk use in preterm infants: outcomes of the East of
England quality improvement programme. Arch Dis Child Fetal Neonatal Ed.
2014 ;99:F395-401.
8. Sisk PM, Lovelady CA, Dillard RG, Gruber KJ.
Lactation counseling for mothers of very low birth weight infants:
effect on maternal anxiety and infant intake of human milk. Pediatrics.
2006:117:e67-75.
9. Murphy L, Warner DD, Parks J, Whitt J, Peter-Wohl
S. A quality improvement project to improve the rate of early breast
milk expression in mothers of preterm infants. J Hum Lact.
2014;30:398-401.
10. Pineda RG, Foss J, Richards L, Pane CA.
Breastfeeding changes for VLBW infants in the NICU following staff
education. Neonatal Netw. 2009;28:311-9.
11. Ward L, Auer C, Smith C, Schoettker PJ, Pruett R,
Shah NY, et al. The human milk project: a quality improvement
initiative to increase human milk consumption in very low birth weight
infants. Breastfeed Med. 2012;7:234-40.
12. Meier PP, Engstrom JL, Mingolelli SS, Miracle DJ,
Kiesling S. The Rush Mothersí Milk Club: breastfeeding interventions for
mothers with very-low-birth-weight infants. J Obstet Gynecol Neonatal
Nurs. 2004;33:164-74.
13. Verma A, Maria A, Pandey RM, Hans C, Verna M,
Sherwani F. Family-centered care of sick newborns. A randomized
controlled trial. Indian Pediatr. 2017;54:453-9.
14. Dogra S, Thakur A, Garg P, Kler N. Effect of
differential enteral protein on growth and neurodevelopment in
infants <1500 g: A randomized controlled trial. J Pediatr Gastroenterol
Nutr. 2017;64:e126-e32.
15. Amin SG. Control charts 101: A guide to health
care applications. Qual Manag Health Care. 2001;9:1-27.
16. Benneyan JC, Lloyd RC, Plsek PE. Statistical
process control as a tool for research and healthcare improvement. Qual
Saf Health Care. 2003;12:458-64.
17. Moen RD, Nolan TW, Provost LP. Improvement in
Quality In: Judy Bass, editor. Quality Improvement through
Planned Experimentation, 3rd ed. New York: McGraw-Hill; 2012.p.1-23.
18. Provost LP , Murray SK. Learning from Variation
in Data In: Jossey Bass, editors. The Healthy Care Data
Guide Learning from Data for Improvement,1st ed. San Francisco: Wiley
Inc; 2011.p.116-7.
19. Spatz DL. Ten steps for promoting and protecting
breastfeeding for vulnerable infants. J Perinat Neonatal Nurs.
2004;18:385-96.
20. Fugate K, Hernandez I, Ashmeade T, Miladinovic B,
Spatz DL. Improving human milk and breastfeeding practices in the NICU.
J Obstet Gynecol Neonatal Nurs. 2015;44: 426-38.
|
|
|
 |
|

