|
|
|
Indian Pediatr 2015;52: 753 -757 |
 |
Umbilical Cord Milking and Hematological
Parameters in Moderate to Late Preterm Neonates: A Randomized
Controlled Trial
|
|
Bimlesh Kumar, Amit Upadhyay,
*Sunil Gothwal, Vijay Jaiswal,
#Payas Joshi and
#Kirti Dubey
From Departments of Pediatrics and Obstetrics, LLRM
Medical College, Meerut, UP; and *Department of Pediatrics,
SMS Medical College, Jaipur, Rajasthan; India.
Correspondence to: Dr Amit Upadhyay, Department of
Pediatrics, LLRM Medical College, Meerut, India.
Email: au.llrm@gmail.com
Received: March 20, 2015;
Initial review: May 02, 2015;
Accepted: July 15, 2015.
(CTRI/2014/12005278)
|
Objectives: To investigate the effect of
umbilical cord milking on hematological parameters at 6 weeks of age in
late preterm neonates.
Design: Randomized controlled trial.
Setting: A tertiary care center of Northern
India during 2013-14.
Participants: 200 moderate to late preterm
neonates randomly allocated to early cord clamping or umbilical cord
milking group (100 in each).
Intervention: In milking group, 25 cm length
of cord was milked towards the baby thrice after separating (within 30
s) it from placenta.
Main outcome measures: Hemoglobin and serum
ferritin at 6 weeks of age.
Results: Mean (SD) serum ferritin [428.9
(217.6) vs. 237.5 (118.6) ng/mL; P< 0.01] and hemoglobin
[12.1 (1.5) vs. 10.4 (1.2) gm/dL; P<0.01] at 6 weeks were
significantly higher in umbilical cord milking group. In early neonatal
period, hemodynamic and hematological parameters were not significantly
different. Higher incidence of jaundice with higher phototherapy rates
(33% vs. 9%; P<0.01) were noted in umbilical cord milking
group.
Conclusion: In preterm neonates, umbilical
cord milking at birth enhances iron stores at 6 weeks of age. Higher
phototherapy rates with this intervention are a matter of concern.
Keywords: Anemia, Ferritin, Hemoglobin, Prematurity.
|
|
D
elayed cord clamping, in which the cord is
clamped only after a short delay (30 to 180 s) after birth, improves
iron status, reduces anemia and need for blood transfusion, and also
provides higher amount of placental stem cells to the infant without
causing any harm to the mother [1,2]. Despite the evidence and
recommendations for this intervention, there is reluctance by the
neonatologists and obstetricians to adopt it because of possible
conflict with immediate newborn resuscitation [3]. An alternative to
this technique is umbilical cord milking, which is also a process of
transferring extra blood from umbilical cord to the baby by milking or
stripping the umbilical cord towards the baby. Recent studies have
demonstrated that it results in comparable increase in hemoglobin (Hb)
in extreme premature and term neonates [4,5]. Considering insufficient
data regarding use of umbilical cord milking in moderate to late preterm
neonates, we designed this trial with the objective to investigate its
effect on iron status at 6 weeks in moderate to late preterm infants.
Methods
This study was a single center randomized controlled
trial, conducted at Department of Pediatrics and Obstetrics of a
tertiary care institute in Northern India from September 2013 to August
2014. Trial was approved by the Institutional ethical committee.
Informed written consent was taken before the delivery from expectant
mother and/or her spouse while mother was in labour room or Operation
theater. Moderate to late preterm neonates (32 0/7 to 36 6/7 weeks)
delivered either vaginally or by lower segment cesarean section at our
institute and families living within 5 km radius of institution premises
were included in the study. Gestational age was determined by last
menstrual period (LMP) and by ultrasound of first trimester, if LMP was
not known. Neonates were excluded if they had umbilical cord length less
than 25 cm, or were non-vigorous at birth. Multiple births (twins,
triplets), those born to Rh negative or retrovirus positive mothers,
hydrops fetalis and those with major congenital anomalies, cord prolapse
or cord anomalies like true knots were also excluded. Babies born to
mothers with complications such as placental abruption, placental
implantation disorders (placenta previa or accreta) or chorioamnionitis
were excluded only if they were born limp.
The sample size was based on a previous trial done in
our institute which showed mean (SD) hemoglobin level in the
intervention arm as 11.9 (1.6) g/dL and in the control arm as 10.9 (1.0)
g/dL, respectively [5]. To detect a mean increase in hemoglobin by 1 g/dL
in neonates with umbilical cord milking, the sample size in each group
was estimated as 85 for a two-tailed value of 0.05 and power of 90%.
Considering a 15% attrition rate, the total sample size was upscaled to
100 babies in each group. We used an online generated random number
list, and assigned even numbers to early cord clamping (control) group
and odd numbers to milking of cut cord (intervention) group. The numbers
were written on small slips and placed in serially numbered opaque
sealed envelopes. Sealed envelope was opened by a delivery room staff
nurse, just after the delivery after ensuring baby is not limp and had
no true knot. Standardized protocol for execution of each intervention
was followed where all members of neonatal care team including
obstetricians involved in this study were trained through separate live
demonstrations for each intervention. Cord milking was also demonstrated
with an online video [6]. In UCM (Intervention) group, just after
delivery, umbilical cord was clamped and cut immediately (within 30 s)
at placental end leaving cord length of at least 25 cm from the
umbilicus of the baby. Attending neonatologist placed the infant under
radiant warmer where cord was held upright and milked thrice towards
baby at a speed of 10 cm/s, and then clamped at 2-3 cm from umbilicus.
In control group, cord was clamped and cut immediately at 2-3 cm from
umbilicus. The neonatal resident recorded the time elapsed by a
wall-mounted clock in delivery room. If this co-ordination of delivery
and assessment for inclusion took 30 sec or more, babies were excluded.
Similar standard care was provided in both the groups. As per our
obstetric department protocol, oxytocin was routinely given soon after
delivery. It was given intramuscular in vaginal and intravenous in
cesarean deliveries.
Relevant maternal details were obtained from case
records. All enrolled infants were connected to a multi-parameter
monitor and relevant data were collected by team leader who attended the
delivery and subsequent data were collected at designated time by the
doctor in neonatal intensive care unit. Infants were followed up at 6
weeks of postnatal age. Primary outcomes were hemoglobin and serum
ferritin at 6 weeks of age. The secondary outcomes were: hemodynamic
parameters (heart rate, respiratory rate and mean blood pressure),
clinical parameters (respiratory distress, need for oxygen,
polycythaemia and jaundice requiring phototherapy) and laboratory
parameters (hemoglobin and hematocrit at 12 h and 48 h and serum
bilirubin level at 48 h). Hemoglobin was measured by Cyan method while
serum ferritin was measured by one step enzyme immunoassay sandwich
method with a final florescent detection using ferritin kit (Biomeriux
India).
Analysis of continuous data was done by unpaired t
test and categorical data was compared using chi square or Fisher exact
test as applicable. P value of less than 0.05 was considered
significant. Analysis was done using STATA 11.0 software.
Results
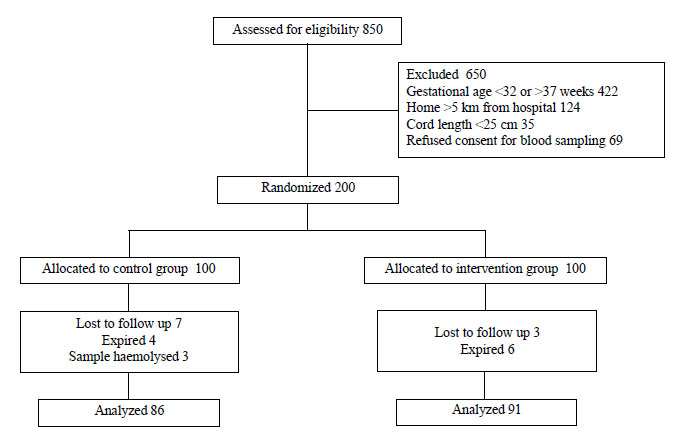
Fig. 1 shows the flow of study participants.
Out of 200 enrolled neonates, 177 completed the trial. Baseline
characteristics in two groups were comparable (Table I)
except maternal Hb which was more in intervention group by 0.3 mg/dL.
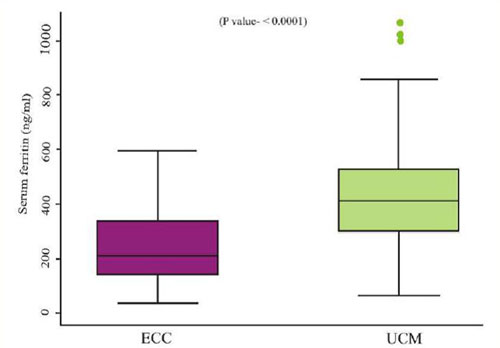
The mean (SD) serum ferritin and hemoglobin at 6 weeks were higher in
the intervention group as compared to control group (Table II,
Fig. 2). Mean blood pressure at 30 min, 12 h and 48 h
after birth was higher in intervention group, but was not statistically
significant (Table III). In immediate neonatal period,
hemoglobin and hematocrit were slightly higher in intervention group,
but it was not statistically significant (Table III). No
significant difference was observed in heart rate and respiratory rate
between two groups. Serum bilirubin level at 48 h was significantly
higher in intervention group with significantly higher phototherapy
rates (33% vs. 9%; P<0.01). In two babies in intervention
group, serum bilirubin reached closed to exchange blood transfusion
level but improved with intensive phototherapy without any complication.
Ten infants in intervention group and five infants in control group
developed respiratory distress, and required oxygen and admission in
Neonatal Intensive Care Unit (NICU).
 |
|
Fig. 1 Flow of participants in the
study.
|
TABLE I Baseline Characteristics in Two Study Groups
Characteristics
|
Early cord camping group |
Umbilical cord milking group |
95% CI of difference |
P value |
|
Maternal |
|
Hemoglobin (g/dL) |
9.5 (0.9) |
9.8 (1.0) |
0.01 to 0.5 |
0.04 |
|
Weight (kg) |
62.9 (3.7) |
63.5 (4.7) |
63.8 to 62.6 |
0.29 |
|
Smokinga |
14 (14%) |
12 (12%) |
— |
0.67 |
|
Gestational age (wk) |
34.5 (1.5) |
34.7 (1.3) |
0.2 to 0.6 |
0.29 |
|
Mode of delivery a(Vaginal ) |
61 (61%) |
56 (56%) |
— |
0.47 |
|
Use of oxytocin a |
100 (100%) |
100 (100%) |
— |
1 |
|
Neonatal |
|
Birth weight (g) |
2354 (274) |
2397 (268) |
33 to 118 |
0.27 |
|
Sex (male) a |
54 (54%) |
52 (52%) |
—- |
0.78 |
|
APGAR Score at 1min |
6.9 (0.3) |
6.9 (0.3) |
6.9 to 6.8 |
0.82 |
|
Small for gestational age a |
10 (10%) |
8 (8%) |
— |
0.62 |
|
Exclusive breastfeeding rates at 6 wk a |
55 (63.9%) |
55 (60.4%) |
— |
0.63 |
|
Weight at 6 wk (g) |
3239 (244) |
3291 (179) |
12 to 114 |
0.11 |
|
Value in mean (SD) or a No. (%). |
TABLE ÌI Comparison of Hematological Parameters in Two Study Groups
|
Parameters |
ECC Group (n=100) |
UCM Group (n=100) |
95% CI of difference |
P value |
|
Hemoglobin (g/dL) |
|
12 hr |
16.0 (2.7) |
16.7 (2.3) |
0.02 to 1.4 |
0.04 |
|
48 hr |
15.4 (2.7) |
15.6 (2.7) |
0.7 to 0.9 |
0.67 |
|
6 week |
10.4 (1.2) (n=86) |
12.1 (1.5) (n=91) |
1.3 to 2.1 |
<0.001 |
|
Packed cell volume (%) |
|
12 hr |
48.2 (8.2) |
50.1 (6.9) |
0.2 to 4.0 |
0.07 |
|
48 hr |
46.5 (7.2) |
47.1 (7.7) |
1.5 to 2.7 |
0.58 |
|
Serum ferritin (ng/mL) at 6 wks. |
237.5 (118.6) (n=86) |
428.9 (217.6) (n=91) |
139.1 to 243.9 |
<0.001 |
|
Serum bilirubin at 48 hr |
8.7 (2.5) |
13.0 (3.5) |
3.5 to 5.2 |
<0.01 |
|
Values in Mean (SD); ECC: early cord clamping; UCM:
umbilical cord milking. |
 |
|
Fig. 2 Box and Whisker plot for serum
ferritin levels at 6 weeks.
|
TABLE III Hemodynamic Outcome Variables
|
Parameters |
ECC Group (n =100) |
UCM Group (n =100) |
95% CI of difference |
P value |
|
Mean blood pressure (mmHg) |
|
30 min |
48 (10.2) |
50 (11.4) |
0.9 to 5.1 |
0.18 |
|
12 h |
48 (9.5) |
49 (10.4) |
1.8 to 3.7 |
0.49 |
|
48 h |
47 (9.6) |
48 (10.1) |
2.4 to 3.1 |
0.79 |
|
Heart rate |
|
30 min |
147 (10.1) |
149 (12.7) |
1.7 to 4.7 |
0.36 |
|
12 h |
146 (10.3) |
148 (13.4) |
1.6 to 5.9 |
0.29 |
|
48 h |
145 (11.7) |
147 (13.7) |
1.9 to 5.1 |
0.38 |
|
Respiratory rate |
|
30 min |
50 (8.5) |
52 (10.2) |
0.7 to 4.6 |
0.14 |
|
12 h |
49 (9.1) |
51 (10.4) |
1.1 to 4.4 |
0.23 |
|
48 h |
48 (9.9) |
49 (11.2) |
1.9 to 3.9 |
0.49 |
|
Values in Mean (SD); ECC: early cord clamping; UCM:
umbilical cord milking. |
Discussion
This study demonstrated that in moderate to late
preterm neonates, umbilical cord milking improved hematological
parameters (hemoglobin and ferritin) in early infancy. There was concern
about higher incidence of jaundice requiring phototherapy in milking
group. No other significant adverse effects were noted with umbilical
cord milking.
The main limitation of the study was that it was an
open-label trial as blinding was not possible because of the nature of
two interventions. For hemodynamic monitoring, only vital parameters
like heart rate, respiratory rate and BP was measured. Circulating
volume was not measured as it was not feasible in our settings. A short
duration of follow up was also one of the limitations.
Many trials have demonstrated the benefits of either
delayed cord clamping and/or umbilical cord milking on the hematological
status immediately after birth which persists into early infancy
[4,5,7-11]. In view of various studies and a Cochrane review [12]
demonstrating the benefits of delayed cord clamping, delayed cord
clamping has almost become a standard of care. However, it may not be
feasible in all deliveries, especially in neonates who require
resuscitation at birth. Umbilical cord milking also increases the
placental and cord blood transfusion to the newborn, and is feasible
even in those requiring resuscitation. Hosono, et al. [13]
reported the first randomized controlled trial on 40 very preterm
infants (26-29 weeks), and demonstrated higher hemoglobin, decreased
number of transfusions and shorter duration of ventilation or
supplemental oxygen in the milked group as compared to early cord
clamping. A randomized controlled trial from our center on 200 term
babies also reported that umbilical cord milking after birth leads to
higher hemoglobin and better iron status at 6 weeks of age as compared
to infants who received early cord clamping [5]. Earlier studies
[8,13,14] evaluated milking while the baby was still attached to
placenta, while we have milked the cord after cutting it leaving 25 cm
length. The transfer of blood to the infant in this procedure may not be
the same as that when cord milking is done with placenta still attached.
However, there is no trial evaluating this comparison. Nakagawa, et
al. [14] have earlier reported increase in incidence of jaundice
requiring phototherapy in neonates who received delayed cord clamping.
Another recent study [16] reported significantly longer duration of
phototherapy with delayed cord clamping. Some other trials in term
babies have not shown increase in serum bilirubin or need for
phototherapy [5,7,17]. This could be due to inability of relatively
immature liver in late preterm to handle the extra blood transfused
through these maneuvers.
We conclude that in moderate to late preterm babies,
umbilical cord milking improves hematological parameters at 6 weeks
postnatal age, but there seems to be a higher need for phototherapy with
umbilical cord milking. Umbilical cord milking may be considered in
moderate to late preterm neonates as a routine or in settings where
delayed cord clamping is not feasible or when the neonate is likely to
require resuscitation at birth.
Contributors: BK and PJ collected, analyzed and
interpreted the data for the study, and drafted the manuscript. AU, SG,
VJ and KD conceptualized and designed the study, analyzed the data and
revised the manuscript. AU, SG, VJ and KD cross checked the data and
helped in review of literature. Critical review and final approval of
manuscript was performed by all authors. AU will act as guarantor of the
study.
Funding: None; Competing interests: None
stated.
|
What is Already Known?
•
Delaying of cord clamping at birth improves hematological
parameters in infancy. Umbilical cord milking also has the
potential to improve hematological parameters by transfer of
more blood from placenta to the infant.
What This Study Adds?
•
Umbilical cord milking helps in improving hematological
status at 6 weeks of postnatal life in moderate to late preterm
neonates.
|
References
1. Gupta R, Ramji S. Effect of delayed cord clamping
on iron stores in infants born to anemic mothers: A randomized
controlled trial. Indian Pediatr. 2002; 39:130-5.
2. Mathew JL. Timing of umbilical cord clamping in
term and preterm deliveries and infant and maternal outcomes: A
systematic review of randomized controlled trials. Indian Pediatr. 2011;
48:123-9.
3. Mercer JS, Erickson-Owens DA. Is it time to
rethink cord management when resuscitation is needed? J Midwifery Womens
Health. 2014; 59:635-44.
4. Katheria A, Blank D, Rich W, Finer N. Umbilical
cord milking improves transition in premature infants at birth. PloS.
One. 2014; 9:e94085.
5. Upadhyay A, Gothwal S, Parihar R, Garg A, Gupta A,
Chawla D,et al. Effect of umbilical cord milking in term and near
term infants: randomized control trial. Am J Obstet Gynecol. 2013;
208:120.e1–6.
6. Taylor V. (for Prof. William Tarnow-Mordi).
Correct umbilical cord "milking" technique. Australian Placental
Transfusion Study, West Mead Hospital. Sydney, Australia. Available
from: http://www.videos. med.usyd.edu.au/unitube/videos/file19.
Accessed May 15, 2015
7. Van Rheenen P, de Moor L, Eschbach S, de Grooth H,
Brabin B. Delayed cord clamping and haemoglobin levels in infancy: A
randomised controlled trial in term babies. Trop Med Int Health.
2007;12:603-16.
8. Rabe H, Jewison A, Alvarez RF, Crook D, Stilton
D, Bradley R,et al. Milking compared with delayed cord clamping
to increase placental transfusion in preterm neonates: a randomized
controlled trial. Obstet Gynecol. 2011;117:205-11.
9. Grajeda R, Pérez-Escamilla R, Dewey KG. Delayed
clamping of the umbilical cord improves hematologic status of Guatemalan
infants at 2 month of age. Am J Clin Nutr. 1997;65:425-31.
10. Lanzkowsky P. Effects of early and late clamping
of umbilical cord on infant’s haemoglobin level. BMJ. 1960; 2:1777-82.
11. Chaparro CM. Timing of umbilical cord clamping:
Effect on iron endowment of the newborn and later iron status. Nutr Rev.
2011;69:S30-6.
12. McDonald SJ, Middleton P. Effect of timing of
umbilical cord clamping of term infants on maternal and neonatal
outcomes. Cochrane Database Syst Rev. 2008; CD004074.
13. Hosono S, Mugishima H, Fujita H, Hosono A, Minato
M, Okada T, et al. Umbilical cord milking reduces the need for
red cell transfusions and improves neonatal adaptation in infants born
at less than 29 weeks’ gestation: A randomised controlled trial. Arch
Dis Child Fetal Neonatal Ed. 2008; 93:F14-9.
14. Erickson-Owens DA, Mercer JS, Oh W. Umbilical
cord milking in term infants delivered by cesarean section: a randomized
controlled trial. J Perinatol. 2012;32:580-4.
15. Nakagawa M, Ishida Y, Nagaoki Y, Ohta H, Shimabukuro
R, Hirata M,et al. Correlation between umbilical cord
hemoglobin values and rates of jaundice requiring phototherapy in
healthy newborns. Pediatr Int. 2014 Dec 23. [Epub ahead of print]
16. Ranjit T, Nesargi S, Rao PN, Sahoo JP, Ashok C, Chandrakala
BS, et al. Effect of early versus delayed cord clamping on
hematological status of preterm infants at 6 wk of age. Indian J Pediatr.
2015; 82:29-34.
17. Jaiswal P, Upadhyay A, Gothwal S, Singh D, Dubey
K, Garg A, et al. Comparison of two types of intervention to
enhance placental redistribution in term infants: Randomized control
trial. Eur J Pediatr. 2015 Mar 24. [Epub ahead of print].
|
|
|
 |
|

