Ashutosh Halder
Jaganath Pahi
Mandakini Pradhan
Amita Pandey
Ratni Gujral*
S.S. Agarwal
From
the Department of Medical Genetics and
Radiology*, Sanjay Gandhi Post Graduate Institute of Medical Sciences, Raebareli Road, Lucknow 226 014, India.
Reprint requests: Dr. Ashutosh Halder, Assistant Professor, Department of Medical Genetics, SGPGIMS, Lucknow 226 014, India.
Manuscript received: September 17, 1997; Initial review completed: November 10, 1997;
Revision accepted: March 19, 1998
The term iniencephaly implies deficiency of occiput in the region of foramen magnum, spina bifida of considerable extent and retroflexion (extreme extension) of the spine. In most cases the cranial cavity is well formed and skin over the retroflexed region is uninterrupted. Howkins and
Lawrie(1) in 1939 classified iniencephaly
into simple iniencephaly (clausus-no encephalocele and apertus-with encephalocele) and anencephaly with spinal retroflexion. However, the etiopathological distinction between these two entities was not established(2) until recently where anencephaly is considered by some(3,4) as associated CNS malformation with iniencephaly. The incidence of iniencephaly has been estimated to be between 1
in 900(5) to 1 in
2200(6)
deliveries; whereas
from India it has been reported to be 1 in 60,000 deliveries(7). We have come across 19 cases of iniencephaly in over 61/2
years period among 102 malformed fetuses referred to our center for fetal autopsy. The
referral diagnosis in 13 of them was anencephaly or multiple congenital anomalies, i.e., incorrect. This paper presents detailed demographic, clinical, radiologic and necropsy findings of the 19 iniencephaly cases. Our data supports that simple iniencephaly and anencephaly with spinal retroflexion (here, we like to designate as iniencephaly with anencephaly) are same entity and not a rare malformation around Lucknow.
Subjects and Methods
Nineteen iniencephaly/iniencephaly with anencephaly were referred to the Genetic Center over 61/2 years period from March, 1991 to October, 1997. Four cases were diagnosed antenatallyas iniencephaly (3 cases) or iniencephaly with anencephaly (1 case) before termination of pregnancy by antenatal ultrasonography; 2 cases were referred correctly as iniencephaly after delivery by clinical examination whereas 13 cases were labelled as multiple congenital anomalies or anencephaly even after delivery (i.e., unable to recognize the condition).
A detailed external examination, chromosomal analysis (one from each group), anthropologic measurements, necrography, computerised tomography (two from each group) and protocol based necropsy were performed as per standard procedure. Body weight, organ weight and other measurements were compared with the standards described by Wigglesworth and Singer(8). Gestational age was calculated from last menstrual period and ultrasonographic femur length, and after delivery with foot length. Fetal sex was noted. Cases were divided into two groups: Group A
-
Simple Iniencephaly, 8 cases (clausus
-
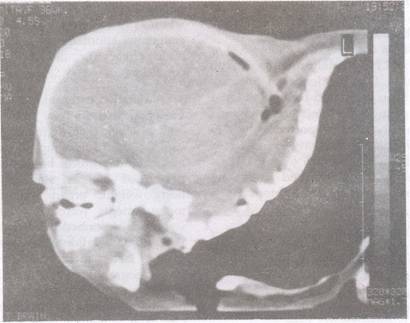
7 cases (Fig. 1a);
apertus
-
1 case) and Group B - Iniencephaly with anencephaly, 11 cases
(Fig. 2a).
 |
Fig. 1(a) Clinical photograph (lateral)
|
Information was collected on birth order, month of conception,
ethnic back- ground, consanguinity, parental age at conception, periconceptional events, maternal drug exposure, maternal illness, family history of birth defects and maternal past obstetric history. The results are compared between the two groups.
 |
|
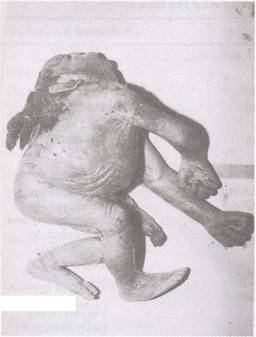
Fig.
1(b) CT (saggital) of simple iniencephaly (clausus) showing exaggerated retroflexion and cervicothoracic vertebral anomalies. |
|
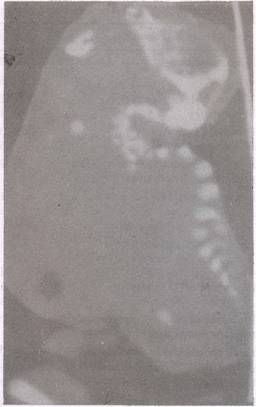 |
Fig. 2. (a) Clinical photograph (lateral),
|
Fig. 2(b). CT (saggital) of iniencephaly with anencephaly showing
anencephaly in addition to cervicothoracic vertebral anomalies and retroflexion as in Group A. |
Results
Among 19 cases of iniencephaly/iniencephaly with anencephaly, 8 were simple iniencephaly (7 clausus and 1 apertus) and eleven were iniencephaly with anencephaly. All 19 cases fulfilled 3 major diagnostic criteria, namely, occipital bone defect, spinal rachischisis and
cervicothoracic spinal retroflexion. Detailed observations on demographic characteristics of the two groups are given in Table I. There was excess of females in both the groups. There was no parental consanguinity. The mean parental age at conception was quite similar in the 2 groups
(Table
I).
The number of 1st trimester spontaenous abortions (missed abortions) was also com- parable between the two groups. There was one precurrence of NTD (anencephaly; female) in Group A whereas the figure for Group B was 4 (anencephaly-one, anencephaly with limb defect-one and lower spina bifida, not specified-two; 3 were fernale). Most of the cases were from Hindu middle class vegetarian families around
Lucknow
(Table
I). There was no seasonal
effect on conception between the
groups (winter was the commonest). There was no history of exposure to drugs or
radiation or infection in early pregnancy in either group. Nine pregnancies were associated with polyhydramnios (3/8 in Group A and 6/11 in Group B) and one complicated with pregnancy induced hypertension (Group B). All cases demonstrated disturbance of growth as characterized by reduced weight and organ hypoplasia. The detailed observations on associated anomalies are given in Table II. The differences were insignificant. Craniospinal CT was carried out in 4 cases (2 from each group). It provided more clear bony demarcation of occipitocervical region in comparison to necrogram. CT findings in Group A (Fig.
1b) were widely separated sutures of vault
bones, large foramen magnum, defective formation of base of skull and sella turcica,
well formed facial bones, severe abnormality of spine (cervical vertebrae
-
reduced in number, hypoplastic, deformed, fused and without arch; thoracic vertebrae
-
multiple congenital anomalies), widened neural canal, absence of spinal cord in upper portion and hypoplasia of cerebellum and vermis in 3 (including Dandy Walker malformation in 2; most cases were noninformative due to degenerative changes in brain or anencephaly). The CT findings in Group B (Fig. 2b) were similar except there were no vault bones, no brain tissue and marked hypoplasia of facial bones.
Chromosomal analysis did not reveal any abnormality in 2 cases (one from each group).
TABLE I
Demographic Characteristics of the Two Groups.
|
Parameters / Characters |
Group B |
Group A |
|
Number of
cases |
8 |
11 |
|
Females |
6 |
9 |
|
Maternal
Mean Age (yr) |
28.75 |
27.1 |
|
SD
(range) |
4.86 (20-35) |
3.98 (22-32) |
|
Paternal
Mean Age (yr) |
33.25 |
30.54 |
|
SD
(range) |
5.2 (25.40) |
3.04 (25-35) |
|
Primipara (prediction for precurrence impossible) |
3 |
5 |
|
Precurrence of NTD in sibs |
1 in one family anencephaly; F |
4 in 4 families
* anencephaly-F; * anencephaly and limb defect-M;
* spina bifida,
2 cases F+F. |
|
History of NTD in family |
1 in one family spina befida;
F |
Nil
|
|
Precurrence of other congenital malformations in sibs |
Nil |
1 in one
family Heart disease: F |
|
Early
spontaneous abortion (1st trimester, unidentifiable sex) |
3 in 2
mother |
3 in 1 mothers |
|
Vegetarian |
7 |
8 |
|
Winter conception (LMP in December/early January) |
2 |
5 |
Differences are insignificant statistically. F=Female; M=Male;
LMP=Date of last menstrual period.
Discussion
Iniencephaly is a developmental error occurring in early pregnancy prior to closure of cephalic neural folds at 24 days gestational age(8). It is characterized by arrest as well as imperfect development of base of skull (portion of neural tube) and vertebral column (cervicothoracic region mainly). At the early stage of embryo, paravertebral sclerotome
(mesoderm) differentiates into two parts, a ventral mass (forms the vertebral bodies, pedicles and
their cranial homologous) and a dorsal mass (forms neural arches and vault bones of the cranium). In iniencephaly, one or both of these masses are hypoplastic or ill developed.
TABLE II
Details of Associated Malformations
Parameters/Associated
Findings |
Simple iniencephaly
(n
=
8) |
Aneniniencephaly
(n
=
11) |
|
Hydrops |
0 |
2 |
|
Thymic
hyperplasia* |
1 |
4 |
|
Diaphragmatic hernia/Eventration |
2 |
4 |
|
CVS malformation |
3
(VSD-2, ASD-1) |
3 (Hypoplastic Lt. heart and atrialisation of Rt. Ventricle) |
|
Pulmonary hypoplasia*
|
5 |
8 |
|
Hepato-biliary malformation |
0 |
1 (unlobulated liver & bile duct opens in stomach) |
|
Renal malformation |
1 (horse-shoe) |
2 (excess lobulation; dilated pelvicalaceal junction) |
|
Adrenal hypoplasia &/or atrophy* |
3 |
8 |
|
GIT malformation |
2 |
3 |
|
Omphalocele/Exomphalos |
2 |
4 |
|
Inguinal hernia |
0 |
2 |
|
Dandy Walker malformations |
2 |
Not applicable |
* On basis of organ weight compared with standard(8) of same age
The distinction between the two groups may relate to the time of onset and duration
of insult. Primate and human neural tube closure was believed in past as a continuous process that begins in the cervical region of the embryo and proceeds rostally as well as caudally(9). However, in recent years evidence is accumulating in favor of multi-site initiation of neural tube closure in humans and NTD represents the failure of one or more of 5 closure sites(10,11). In simple iniencephaly, the defect found in occipitocervical region (more pronounced in apertus) indicates site 1 (mid cervical)
and probably site 4 (caudal end of rhombencephalon) closure defect whereas in Group B (iniencephaly with anencephaly) where vault and facial bones as well as lower vertebrae, in addition to occipitocervical region, are involved, favours all 5 sites (site 2
-
between prosencephalon and mesencephalon; site 3- at stomodeum; site 5- most caudal end of neural tube) closure defect hypothesis.
Exagerated spinal retroflexion is due to absence of neural arches. Malformations/ deformations and hypoplasia, for example, pulmonary hypoplasia,
diaphragmatic hernia, omphalocele, etc. are due to lack of space (increased pressure) in thoracic and abdominal cavity(2) which is because of retroflexion and crowding of ribs (result of vertebral malformation).
Anencephaly and other CNS malformations are often associated with this condition(3,4) along with other visceral malformations(12). CNS malformations like cerebeller vermis hypoplasia are common in Group A and we had seen these in 3 cases; the remaining cases were noninformative.
The literature on iniencephaly is Cautious on the relationship between simple iniencephaly and iniencephaly with anencephaly. In this study, which is possibly the largest series in literature, we have observed that both the conditions fulfil the basic diagnostic criteria, namely, occipital bone defect, cervicothoracic spinal rachischisis and hyprextension of spinal column, both show female preponderance, both are common in NTD prone areas, both have similar systemic malformations and similar precurrence of NTD among sibs (indicates presence of similar underlying genetic contribution) thus favouring them as the same entity. The cause of female preponderence is not known. It may be due to incomplete penetrance and/or male lethality. These need to be evaluated in future with special attention to chromosome X.
We conclude from this study that both the entities are same, part of neural tube defect, could be of heterogenous etiology and are not rare around Lucknow, India.
