|
|
|
Indian Pediatr 2021;58:951-954 |
 |
Comparison of Clinical Features and Outcome
of Dengue Fever and Multisystem Inflammatory Syndrome in
Children Associated With COVID-19 (MIS-C)
|
|
Gurdeep Singh Dhooria, Shruti Kakkar, Puneet A Pooni, Deepak Bhat,
Siddharth Bhargava, Kamal Arora, Karambir Gill, Nancy Goel
From Department of Paediatrics, Dayanand Medical College and
Hospital, Ludhiana, Punjab.
Correspondence to: Dr Gurdeep Singh Dhooria, Professor, Department of
Pediatrics, Dayanand Medical College and Hospital, Ludhiana, Punjab.
Email:
[email protected]
Received: April 17, 2021;
Initial review: April 20,2021;
Accepted: July 20, 2021.
Published online: July 23, 2021;
PII:S097475591600355
|
Objective:
To identify clinical
and laboratory features that differentiate dengue fever patients from
MIS-C patients and determine their outcomes. Methods: This
comparative cross-sectional study was done at a tertiary care teaching
institute. We enrolled all hospitalized children aged 1 month - 18 years
and diagnosed with either MIS-C and/or dengue fever according to WHO
criteria between June and December, 2020. Clinical and laboratory
features and outcomes were recorded on a structured proforma.
Results: During the study period 34 cases of MIS-C and 83 cases of
Dengue fever were enrolled. Mean age of MIS-C cases (male, 86.3%) was
7.89 (4.61) years. MIS-C with shock was seen in 15 cases (44%), MIS-C
without shock in 17 cases (50%) and Kawasaki disease-like presentation
in 2 cases (6%). Patients of MIS-C were younger as compared to dengue
fever (P=0.002). Abdominal pain and erythematous rash were more
common in dengue fever. Of the inflammatory markers, mean C reactive
protein was higher in MIS-C patients [100.2 (85.1) vs 16.9 (29.3) mg/dL]
(P<0.001). In contrast, serum ferritin levels were higher in
dengue fever patients (P=0.03). Mean hospital stay (patient days)
was longer in MIS- C compared to dengue fever (8.6 vs 6.5 days; P=0.014).
Conclusions: Clinical and laboratory features can give important
clues to differentiate dengue fever and MIS-C and help initiate specific
treatment.
Keywords: Diagnosis, Evaluation, Inflammatory markers,
Management.
|
|
M
ultisystem
inflammatory syndrome in
children (MIS-C), an inflammatory condition following severe acute respiratory
syndrome coronavirus 2 (SARS-CoV-2), has manifestations similar
to toxic shock syndrome or Kawasaki disease [1,2]. Dengue fever
can have clinical presentations similar to MIS-C with presence
of fever, erythematous rash, vomiting, abdominal pain and
develop- ment of shock in severe cases. Correct diagnosis and
appropriate management are critical to reduce mortality in both
the conditions.
We conducted this study to identify clinical
and laboratory features that differentiate dengue fever from
MIS-C patients admitted in a tertiary care center and determine
their outcomes.
METHODS
In this cross-sectional study, we evaluated
all hospitalized children aged 1 month to 18 years diagnosed
with MIS-C and/or dengue fever admitted in the department of
pediatrics, at our center from June to December, 2020. All
patient data were entered in a structured proforma. Patients
were followed up till discharge. Written informed consent was
taken from all participants and the study was approved by the
institutional ethics committee.
All patients with fever for more than three
days and fulfilling the World Health Organization (WHO) criteria
for MIS-C [1] were included. SARS-CoV-2 infection was diagnosed
by nasopharyngeal swab, real time reverse transcription
polymerase chain reaction (RT-PCR) for SARS-CoV-2 infection
using TRUPCR SARS-CoV-2 (3B BLACK BIO, Kilpest India Ltd) and/or
rapid antibody test for SARS-CoV-2 (n=50) using Elevate
Anti-SARS-CoV-2 (IgG and IgM) (Roche Diagnostics GmbH).
Additionally, history of contact with a COVID-19 (coronavirus
disease 2019) positive patient was also considered positive as
per the WHO criteria.
Only confirmed case of dengue fever based on
serological evidence by IgM ELISA or by NS1 antigen positivity
were included. Patients with dengue infection were classified
into two groups viz., dengue with warning signs and severe
dengue, according to WHO classi-fication [5]. Dengue
antibody test for IgM detection was done using an IgM
antibody-capture enzyme-linked immunosorbent assay (MAC-ELISA)
(PanBio, Standard Diagnostics Inc). Dengue NS1 antigen was
detected with the ELISA technique (J Mitra & Co Pvt Ltd).
Patients were serially monitored clinically
and by laboratory parameters and managed as per standard
guidelines. We collected demographic data; past medical history,
co-morbidities, clinical signs and symptoms, results of imaging,
cardiac, and laboratory testing for signs of inflammation
(elevated C-reactive protein (CRP), erythrocyte sedimentation
rate (ESR), fibrinogen, d-dimer, ferritin, lactic acid
dehydrogenase (LDH), or interleukin 6 (IL-6), elevated
neutrophils, reduced lymphocytes and low albumin) and organ
involvement, at presentation and throughout the hospital stay.
The information with respect to need for respiratory and
inotropic support, medications like steroids and intravenous
immune globulin (IVIG), duration of hospital stay and survival
was also collected. Clinical patterns of MIS-C patients
including those with or without shock and coronary involvement
were also noted. Left ventricle dysfunction was graded on
2D-echo as: normal function (EF
>55%), mild
dysfunction (EF 41-55%), moderate dysfunction (EF 31-40%), and
severe dysfunction (EF £30%)
[6]. The American Heart Association criteria for Kawasaki
disease were used [7].
To achieve a power of 80% and a level of
significance of 5% (two sided), for detecting a true difference
of 4 days (7.9-3.8 days) in mean duration of hospital stay
between MIS-C and dengue fever cases from previous studies [3,4]
assuming a pooled standard deviation of 5 days, minimum sample
size of 24 for each group was calculated.
Statistical analysis: Comparison of
quantitative variables was done using Student t-test and
Mann–Whitney U test for independent samples for
parametric and non-parametric data, respectively. For comparing
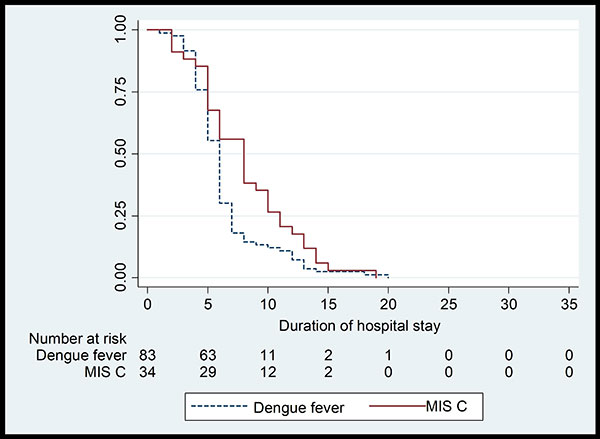
categorical data, chi-square test was used. Kaplan–Meier
analysis was used to estimate the duration of hospital stay in
the three groups, with the end point as time of discharge.
Statistical analyses were performed using SPSS version 24.0.
P<0.05 was considered statistically significant.
RESULTS
Of the 34 MIS-C cases, MIS-C with shock was
seen in 15 (44%) children, MIS-C without shock in 17 (50%)
children and Kawasaki like presentation in two children (6%). Of
the 83 cases of dengue fever, 51(61%) cases had severe dengue by
WHO classification. Mean (SD) age of children with dengue fever
was 10.07 (4.43) years compared to MIS-C, 7.18 (4.81) years (P=0.002).
MIS-C patients had more frequent symptoms of fever, conjunctival
injection, swelling of hand and feet, diarrhea and altered
sensorium. Whereas, abdominal pain and erythematous rash were
more commonly noted in dengue fever patients (Table I).
Clinical bleeding was seen only in dengue fever patients (7%).
Mean (SD) hematocrit was significantly higher in dengue fever
compared to MIS-C patients [38.6% (8.1%) vs. 29.1% (6.9%); P<0.001].
Mean platelet count and total leukocyte count was significantly
lower in dengue fever compared to MIS-C patients.
Table I Clinical Profile, Management and Outcome of Children With MIS-C and Dengue Fever
| Group |
MIS- C |
Dengue |
|
(n=34) |
(n=83) |
| Age a |
|
|
| 0-5 y |
12(35) |
12 (14) |
| 6-10 y |
16 (47) |
35 (42) |
| 11-18 y |
6 (18) |
36 (43) |
| Male gender |
28 (82) |
62 (75) |
| Signs/ symptoms |
|
|
|
Fever at admissionb |
34 (100) |
60 (72) |
| Diarrheaa |
4 (12) |
0 |
|
Abdominal painc |
12 (35) |
47 (57) |
| Vomiting |
17 (50) |
57 (69) |
|
Erythematous rashb |
9 (26) |
55 (66) |
|
Swelling of hand and feetb |
10 (29) |
0 |
| Respiratory distress |
14 (41) |
38 (46) |
|
Altered sensoriumc |
8 (24) |
6 (7) |
|
Conjunctival injectionb |
7 (21) |
0 |
| Myalgiab |
6 (18) |
68 (83) |
| Signs of capillary leak |
13 (38) |
36 (43) |
| Hypotension at admission |
15 (44) |
33 (39) |
| Imaging |
|
|
|
USG-moderate ascitis |
10 (59) |
15 (71) |
| X-ray pleural effusion |
10 (29) |
28 (34) |
|
LV dysfunctionb |
7 (21) |
0 |
| Management |
|
|
| Non-invasive ventilation |
6 (18) |
18 (22) |
|
Mechanical ventilationa |
6 (18) |
2 (2) |
| Inotropes |
13 (38) |
22 (27) |
|
Platelet transfusionc |
0 |
10 (12) |
| Patient outcome |
|
|
| PICU admission |
11 (32) |
21 (25) |
| Discharged |
31 (98) |
81 (98) |
|
All values in no. (%). MIS-C: multi-system inflammatory
syndrome in children associated with COVID-19; USG:
ultrasonography, IVIG: intravenous Immunoglobulin, LMWH
- low molecular weight heparin, PICU: pediatric
intensive care unit. Steroids, intravenous
immunoglobulin, low molecular weight heparin and aspirin
were used in 22, 11, 8 and 8 children with MIS-C and
none with dengue fever. aP<0.01; bP=0.001; cP<0.05. |
Of the inflammatory markers, mean CRP was
higher in MIS-C patients than dengue fever patients. Mean IL-6
levels, D-dimer and fibrinogen levels were also higher in MIS-C
patients. In contrast, mean serum ferritin levels were higher in
dengue fever patients. Left ventricular dysfunction was present
only in MIS-C patients (Table II and
Web Fig 1).
Need for mechanical ventilation was more in MIS-C cases as
compared to dengue fever cases. Intravenous immunoglobulin
(IVIG) infusion, steroids, low molecular weight heparin and
aspirin were used only in MIS-C cases (Table I).
Table II Laboratory Profile and Outcomes of Children With MIS-C and Dengue Fever
| Laboratory parameters |
MIS- C (n=34) |
Dengue (n=83) |
| Serum values |
|
|
| CRP (mg/L)a |
100 (85) |
17 (29) |
|
Ferritin (ng/mL)b |
2878 (5876) |
6136 (6600) |
|
D-Dimer (ng/mL)b
|
1619 (1313) |
733(291) |
|
Interleukin-6 ( pg/mL) |
677 (1505) |
11 (15) |
|
Fibrinogen (mg/dL)c
|
547 (98) |
238 (121) |
|
Hemoglobin (g/dL)a
|
9.7 (2.3) |
12.9 (2.7) |
| Leukocyte count (×109/L)a |
16.6 (12) |
7 (5.7) |
| Platelets (×109/L)a |
173.4 (134.7) |
48.1 (42) |
| AST (U/L) |
524 (1633) |
641 (1359) |
| ALT (U/L) |
236 (569) |
277 (531) |
|
Albumin (g/dL)b |
3 (1.1) |
3.5 (0.8) |
| LV ejection fraction (%) |
52 (13) |
60 (0) |
| PRISM II score |
9 (8) |
8 (6) |
| Hospital stay (d) |
8.1 (4.1) |
6.5 (3.3) |
|
Data prepented as mean (SD). MIS-C: Multi-system
inflammatory syndrome in children associated with
COVID-19; CRP-C-reactive protein; AST-aspartate
transaminase; ALT-alanine transaminase; LV: Left
ventricular;PRISM score II-Pediatric risk of mortality
score. aP<0.001;bP<0.05;cP<0.01. |
 |
|
Fig. 1 Kaplan-Mayer graph
showing mean duration of hospital stay in children with
dengue fever and multisystem inflammatory syndrome in
children associated with COVID-19 (MIS-C).
|
Kaplan-Meier survival curve with discharge as
end point showed significantly longer duration of hospital stay
in MIS-C patients [8.58 days (95% CI 7.13 - 10.03)] compared to
dengue fever patients [6.54 days (95% CI: 5.78 - 7.21)] (P=0.014)
(Fig. 1).
Repeat 2D-echocardiography was done before
discharge in all patients with LV dysfunction/ Kawasaki disease
like presentation. Only two children (5.9%) showed cardiac
dysfunction, one case each with mild and moderate dysfunction.
Both the cases showed resolution during follow-up.
DISCUSSION
The study compares the clinical and
laboratory differences and outcomes of children hospitalized
with MIS-C and dengue fever. Patients with dengue fever were
significantly older as compared to MIS-C. Inflammatory marker
levels of CRP, IL-6, D dimer and fibrinogen were significantly
higher in MIS-C as compared to dengue fever patients.
All studies on MIS-C have reported
hyper-inflammatory state as a primary hallmark [8,9]. The
massive release of inflammatory mediators seen with exaggerated
activation of the immune system is similar to cytokine storm
syndrome [10]. It has been hypothesized that severe dengue is
also caused by a cytokine storm inducing systemic inflammatory
effects [11].
Although post-COVID MIS-C can present with
lower platelet counts but the severe thrombocytopenia (<50 x10 9/L)
as seen in dengue fever, is not common [8]. Also,
hemoconcentration is uncommon in MIS-C patients, making it an
important differentiating feature of dengue fever from MIS-C.
Leukopenia followed by thrombo-cytopenia, capillary leak and
hemoconcentration is very classic and pathognomonic of dengue
fever.
Cornelia, et al. [12] showed presence of
hyper-ferritinemia could discriminate between dengue and other
febrile diseases. Other dengue studies also found an association
between increased ferritin levels and severity of disease
[12,13]. We also found serum ferritin levels to be higher in
dengue fever patients than MIS-C patients.
In the present study, most patients requiring
invasive ventilation were in MIS-C group (18%) as compared to
dengue patients (2%). Other studies have also shown similar
results. [9,14].
The differentiation between dengue fever and
MIS-C is important in contemporary times because of entirely
different management strategy for the two conditions. Dengue
fever patients being managed with aggressive fluid management of
crystalloids and colloids with inotropic support and platelet
transfusions wherever needed. On the other, such aggressive
fluid management in MIS-C patients would be detrimental in
patients with cardiac dysfunction that is often present in MIS-C
patients with shock. Moreover, vital role of intravenous
immuno-globulin and steroids in management of MIS-C patients can
never be overemphasized.
The study has few limitations. Firstly, the
study is an experience from a single center. The diagnosis of
dengue fever was based on serology in one third of cases.
Studies have shown that COVID-19 cases may be misdiagnosed as
dengue fever when relying on DENV IgM, which can remain positive
months after COVID-19 infection [15].
To conclude, the presence of conjunctival
injection, swelling of hand and feet, diarrhea, and altered
sensorium in a febrile child with laboratory evidence of
hyper-inflammation (highly raised CRP, leukocytosis, raised D-
dimers are pointers more in favor of MIS-C. Whereas, vomiting,
myalgia and erythematous rash along with hyperferritinemia,
hemoconcentration, leukopenia and severe thrombocytopenia are
more common in dengue fever patients.
Acknowledgements: Namita Bansal,
Statistician for analyzing the data and for preparation of
tables and graphs. Dr Jatinder Goraya for his advice and
support.
Note: Additional material related
to this study is available with the online version at
www.indianpediatrics.net
Ethics clearance: Institutional ethics
committee; No: DMCH/R&D/2020/168 dated November 09, 2020.
Contributors: GSD, PAP: conceived
and designed the study: SK, NG, KG: recruited the subjects,
collected the data; KA, SB, GSD: literature review, initial
draft of manuscript; PAP, DB, GSD: contributed to manuscript
writing; and PAP, DB, GSD: finalized the manuscript. All authors
approved the manuscript submitted.
Funding: None; Competing interests:
None stated.
|
WHAT THIS STUDY ADDS?
• We provide clinical and laboratory indicators that
can give clues to differentiate dengue fever from MIS-C
patients.
|
REFERENCES
1. Multisystem inflammatory syndrome in
children and adolescents with COVID-19. Scientific brief:
World Health Organization. 15 May 2020. Accessed April 15,
2021. Available from: https:
//www.who.int/publications-detail/multisysteminflammatory-syndrome-in-children-andadole
scents-with-covid19
2. Alsaied T, Tremoulet AH, Burns JC, et
al. Review of cardiac involvement in multisystem
inflammatory syndrome in children. Circulation.
2021;143:78-88.
3. Ahmed M, Advani S, Moreira A, et al.
Multisystem inflammatory syndrome in children: A systematic
review. E Clin Med. 2020;26:100527.
4. Mishra S, Ramanathan R, Agarwalla SK.
Clinical profile of dengue fever in children: A study from
southern Odisha, India. Scientifica (Cairo).
2016;2016:6391594.
5. World Health Organization. Dengue
Guidelines for diagnosis, treatment, prevention and control:
New edition 2009. Accessed April 15, 2021. Available from:
https://www. who.int/rpc/guidelines/9789241547871/en/
6. Tissot C, Singh Y, Sekarski N.
Echocardiographic evaluation of ventricular function-for the
neonatologist and pediatric intensivist. Front Pediatr.
2018;6:79.
7. McCrindle BW, Rowley AH, Newburger JW,
et al; American Heart Association Rheumatic Fever,
Endocarditis, and Kawasaki Disease Committee of the Council
on Cardiovascular Disease in the Young; Diagnosis,
Treatment, and Long-Term Management of Kawasaki Disease: A
Scientific Statement for Health Professionals From the
American Heart Association. Circulation. 2017;135:e927-e999.
8. Feldstein LR, Rose EB, Horwitz SM, et
al. Overcoming COVID-19 Investigators; CDC COVID-19 response
team. Multisystem inflammatory syndrome in U.S. children and
adolescents. N Engl J Med. 2020;23:334-46.
9. Rowley AH. Understanding
SARS-CoV-2-related multi-system inflammatory syndrome in
children. Nat Rev Immunol. 2020;20:453-54.
10. Alunno A, Carubbi F, Rodríguez-Carrio
J. Storm, typhoon, cyclone or hurricane in patients with
COVID-19 ? Beware of the same storm that has a different
origin. RMD Open. 2020;6:e001295.
11. Srikiatkhachorn A, Mathew A, Rothman
AL. Immune-mediated cytokine storm and its role in severe
dengue. SeminImmunopathol. 2017;39:563-74.
12. van de Weg CA, Huits RM, Pannuti CS,
et al. Hyperferritinaemia in dengue virus infected patients
is associated with immune activation and coagulation
disturbances. PLoSNegl Trop Dis. 2014;8:e3214.
13. Chaiyaratana W, Chuansumrit A,
Atamasirikul K, Tangnararatchakit K. Serum ferritin levels
in children with dengue infection. Southeast Asian J Trop
Med Public Health. 2008;39:832-36.
14. Jain S, Sen S, Lakshmivenkateshiah S,
et al. Multisystem inflammatory syndrome in children with
COVID-19 in Mumbai, India. Indian Pediatr. 2020;57:1015-19.
15. Lokida D, Lukman N, Salim G, et al. Diagnosis of COVID-19
in a dengue-endemic area. Am J Trop Med Hyg. 2020;103:1220-22.
|
|
|
 |
|

