|
T he American Academy of
Pediatrics recommends noise levels of less than 45 A-weighted
decibels (dBA) in neonatal intensive care units (NICU) [1]. High
noise level adversely affects the physiological parameters,
behavior, and sleeping patterns of neonate. In a pilot study, we
found that the mean (SD) noise level in our NICU was 57.60
(3.95) dBA. There is a paucity of well-conducted studies
evaluating the effect of earmuffs on noise reduction and
stabilization of physiological parameters, such as heart rate
(HR), respiratory rate (RR), pulse oximeter saturation (SpO2),
and blood pressure in preterm neonates, and the available
studies have shown conflicting results [2-4].
A Cochrane review on the effect of noise
reduction on very low birth weight infants could find only one
single-center randomized controlled trial on 34 newborns [5].
The authors reported better weight gain and neuro-development
among infants who were randomized to wearing silicone earplugs
[6]. Some RCTs have included a reduction in both light and noise
levels, making it difficult to assess the effect of noise
reduction alone [7,8]. Previous studies have compared only the
average values of the physiological parameters [2-4,7-11].
Relying solely on averages could be misleading because averages
do not adequately reflect transient but harmful spikes nor do
they capture fluctuation of the physiological parameters. We
hypothesized that the application of earmuffs on preterm
neonates, nursed in incubators in a NICU, would reduce spikes
and fluctuations in their physiological parameters.
METHODS
We conducted a prospective, cross-over study
in a level III NICU in a tertiary care institute in Northwest
India. The institute ethics committee approved the study
protocol. The study was done in accordance with the Helsinki
declaration and with the Indian Council of Medical Research
(ICMR) national ethical guidelines. We included preterm neonates
(<37 weeks gestation) who required incubator care, but were
otherwise clinically stable. Kangaroo mother care was
intermittently provided but they were unable to consistently
maintain body tempe-rature outside an incubator. Infants who
were ill, sedated, encephalopathic, had scalp electrodes, or had
syndromes associated with deafness were excluded. Written
informed consent was obtained from either parent. Baseline data
included the demographic and clinical profile of enrolled
neonates.
In the ‘control’ period, we recorded HR, RR,
and SpO 2 at
60-second intervals for 2-hour duration by a multichannel
monitor (IntelliVue MX800, Philips) without the
application of earmuffs, thus providing 120 data points for each
parameter. This was followd by a two-hour washout period.
Following this, in the ‘intervention’ period, we recorded data
on the same neonates for 2-hour duration with the application of
earmuffs (Minimuffs, Natus Medical Inc.), which reduce noise by
7 dBA, as per manufacturer. Each subject acted as its own
control.
At the start of the control and the
intervention periods, we measured the sound level inside the
incubator using the Bruel and Kjaer precision integrating sound
level meter type 2230, fitted with microphone type 4155. We
collected data at a time when we anticipated the least number of
nursing/clinical activities so that other stressful conditions
could be avoided.
We defined a ‘spike of tachycardia’ in two
ways- either as any data point of HR
³160 beats
per minute (bpm) or any data point of HR
³180 bpm; a
‘spike of tachypnea’ as RR ³60
breaths per minute; and a ‘spike of hypoxemia’ as SpO2<90%.
We recruited a sample size of convenience of 60 consecutive
eligible subjects.
Statistical analysis: Normality of
distribution was determined by Shapiro-Wilk test and the QQ
plot. We compared proportions between the periods by the McNemar
test and distributions by the Wilcoxon signed rank-sum test for
skewed distributions. Using the data point as the unit of
observation, we compared the proportion of spikes between the
two periods. Using the subject as a unit of observation, we
compared the median number of spikes. We calculated the
coefficient of variation (CoV) of each parameter for each
subject and compared the median CoV. Using 120 data points for a
given parameter, we calculated the area under the curve (AUC)
using a differential function for each subject in each period,
and compared the median AUC between the groups.
RESULTS
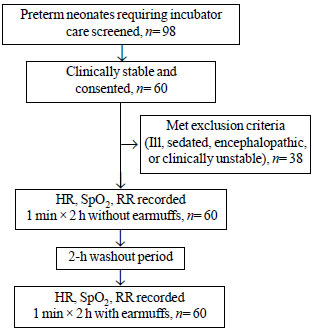
We enrolled 60 eligible subjects (31 males) (Fig.
1). The study population had a mean (SD) gestation of 31
(2.5) weeks, birthweight of 1348 (408.3) grams and current
weight of 1239 (404.9) grams. Median (range) Apgar scores at 5
minutes was 9 (8, 9) and postnatal age was 7 (4, 10) days.
Twenty five (41.7%) subjects were small for gestational age and
the remainder were appropriate for gestational age and 25
(41.7%) were delivered vaginally. The mean (SD) noise level
inside the incubator during the control and intervention periods
was 57.6 (3.9) and 57.3 (3.5) dBA, respectively (P=0.27).
 |
|
Fig. 1 Flow diagram of the study
population.
|
The number of spikes as a proportion of all
individual observations was significantly higher in the control
period compared to the intervention period for all three
parameters (P<0.01) (Table I). There were
statistically significant reductions in the median number of
spikes of tachycardia, tachypnea and hypoxia in the intervention
period compared to the control period (P values of <0.01,
0.01 and <0.01, respectively) (Table II).
Table I Spikes of Physiological Parameters Among Individual Observations in Preterm Neonates
With and Without Earmuffs (N=60)
| Physiological
parameters |
Without
earmuffs |
With earmuffs |
| (number of spikes) |
(n= 7200 |
(n= 7200 |
|
observations) |
observations) |
|
Heart rate ³160 bpm |
1769 (24.5) |
1037 (14.4) |
|
Heart ratee ³180 bpma
|
168 (2.3) |
70 (0.97) |
| Respiratory rate ³60 per min |
1491 (20.7) |
1162 (16.1) |
| Oxygen
saturation <90% |
117 (1.6) |
41 (0.5) |
|
Values in no. (%). Bpm-beats per minute. All P<0.01; aP<0.001. |
Table II Spikes of Physiological Parameters per Subject in Preterm Neonates With and Without Earmuffs (N=60)
| Physiological parameters |
Without |
With earmuffs |
| (no. of spikes per subject) |
earmuffs |
(n= 60) |
|
(n=60) |
|
|
Tachycardia (rate ³160 bpm)a
|
20.5 (2.25, 37.75) |
2.5 (2.5, 18) |
|
Tachycardia (rate ³180 bpm)b |
0 (0, 4) |
0 (0,0) |
| Tachypneac |
18 (2, 40) |
11.5 (11.5, 25) |
| Hypoxemiaa |
0 (0, 1.75) |
0 (0, 0) |
| Values in median (IQR).
aP<0.01; bP<0.001; cP=0.01. |
We compared the median CoV of each parameter
between the two periods (Web Table I). There was a
significantly higher variability of HR (P=0.03) and SpO2
in the control vs intervention periods (<0.01). There were
significantly higher median AUC for HR (P=0.01) and RR,
whereas, for SpO2,
there was almost no difference (P=0.97).
DISCUSSION
We evaluated earmuffs for their effect on
three critical physiological parameters. One of the study’s
challenges was that the data was collected at 1-minute intervals
for two hours during each period. Hence, we examined the data
from various perspectives – observations above a pre-defined
threshold, the variability of the observations per subject, and
an integral of all the observations for each subject. The
application of earmuffs resulted in lower HR and RR and higher
SpO 2; less abnormal
spikes, and less variability of these parameters.
Although SpO2 showed
higher fluctuation in the control compared to the intervention
period, its AUC was similar in both periods because the dips
from baseline were compensated for by the peaks, thus
maintaining AUC constant.
Our results are concordant with some previous
studies. In a non-RCT, Abujarir, et al. [10] applied earmuffs,
identical to ours, to neonates admitted in one area of the NICU
and did not apply in another area. HR, systolic blood pressure
(BP), RR, SpO2
significantly improved among neonates wearing earmuffs, but mean
BP, diastolic BP, and temperature did not. In the RCT by
Abdeyazdan, et al. [2], environmental sound levels were higher
than in our unit, and there was a significant difference in mean
SpO2, RR and HR
between the groups with and without earmuff. Other authors also
report that infants with earmuffs have greater mean SpO2
values, less fluctuation in SpO2,
and sleep more [11].
A few research groups did not find a benefit
of earmuffs [3,4]. Duran, et al. [4] evaluated earmuffs,
identical to those in our study, in a prospective cross-over
study on 20 clinically stable preterm VLBW neonates older than 7
days and nursed in incubators [4]. They reported no significant
differences in body temperature, HR, RR, SpO2,
and BP. Bott, et al. [3] found no effect of earmuffs on
intermittent hypoxia [3].
There are studies that looked at outcomes
other than immediate physiological outcomes. Li, et al. [12]
reported 100 preterm ventilated neonates randomly allocated to
earmuffs and no earmuffs groups. The group wearing earmuffs had
significantly lower incidence of hearing loss, periventricular
hemorrhage and leukomalacia, and better developmental indices on
follow-up. The only study included in the Cochrane meta-analysis
reported better weight gain and neurodevelopmental outcomes, but
no effect on physiological parameters [5,6].
A limitation of our study was that the
sequence of cross-over was not randomly allocated. We did not
perform a formal sample size calculation. Also, we did not
maintain a record of the handlings and procedures done on
preterm neonates during data collection, as we had chosen a
period of the day expected to have minimal inter-ventions. We
did not measure non-invasive BP, because frequent non-invasive
BP (NIBP) recording was not clinically indicated in our stable
population and would have itself been stressful. Intermittent
NIBP recording serves a limited purpose as it is unable to
capture the BP record continuously.
We conclude that applying earmuffs protects
premature infants from noise-induced adverse changes in
physiological parameters. The application of earmuffs decreases
the number of spikes of tachycardia, tachypnea and hypoxemia;
and decreases the variability of HR and SpO2.
Routine use of earmuffs may be considered to improve the
physiological stability of preterm infants nursed in incubators
in the NICU.
Note: Additional material related to this
study is available with the online version at
www.indianpediatrics.net.
Ethics clearance: PGIMER Institute
Ethics Committee; No. 41520/14/910, dated March 24, 2014.
Contributors: AK: substantial
contributions to the design of the work, acquisition and
analysis of data, and drafted the work; SK: substantial
contributions to the conception of the work, interpretation of
the data for the work, and revised the manuscript critically for
important intellectual content; SM: substantial contributions to
the design of the work, and revised it critically for important
intellectual content; SD: substantial contributions to the
concept and design of the work, analysis and interpretation of
the data, and drafted and revised the work for important
intellectual content. All authors approved the final version of
manuscript, and are accountable for all aspects related to the
study.
Funding: None; Competing interest:
None stated.
| |
|
WHAT THIS STUDY ADDS?
•
This study shows that
application of earmuffs among stable preterm neonates
nursed in incubators results in significantly less
spikes and less variability of physiological parameters.
|
REFERENCES
1. Noise: a hazard for the fetus and
newborn. American Academy of Pediatrics. Committee on
Environmental Health. Pediatrics. 1997;100:724-7.
2. Abdeyazdan Z, Ghassemi S, Marofi M.
The effects of earmuff on physiologic and motor responses in
premature infants admitted in neonatal intensive care unit.
Iran J Nurs Midwifery Res. 2014;19:107-12.
3. Bott TS, Urschitz MS, Poets C, et al.
A randomized controlled trial on the effect of earmuffs on
intermittent hypoxia and bradycardia in preterm infants.
Klin Padiatr. 2015;227:269-73 [German].
4. Duran R, Ciftdemir NA, Ozbek UV, et
al. The effects of noise reduction by earmuffs on the
physiologic and behavioral responses in very low birth
weight preterm infants. Int J Pediatr Otorhinolaryngol.
2012;76:1490-3.
5. Almadhoob A, Ohlsson A. Sound
reduction management in the neonatal intensive care unit for
preterm or very low birth weight infants. Cochrane Database
Syst Rev. 2020;1:CD010333.
6. Abou Turk C, Williams AL, Lasky RE. A
randomized clinical trial evaluating silicone earplugs for
very low birth weight newborns in intensive care. J
Perinatol. 2009;29:358-63.
7. Aita M, Johnston C, Goulet C, et al.
Intervention minimizing preterm infants’ exposure to NICU
light and noise. Clin Nurs Res. 2013;22:337-58.
8. Mann NP, Haddow R, Stokes L, et al.
Effect of night and day on preterm infants in a newborn
nursery: Randomised trial. Br Med J (Clin Res Ed).
1986;293:1265-7.
9. Abdeyazdan Z, Ghasemi S, Marofi M, et
al. Motor responses and weight gaining in neonates through
use of two methods of earmuff and receiving silence in NICU.
Scientific World Journal. 2014;2014:864780.
10. Abujarir RS, Greer, W Al Thani M, et
al. The impact of earmuffs on vital signs in the neonatal
intensive care unit. J Neonatal-Perinatal Medicine.
2012;5:25-9.
11. Zahr LK, de Traversay J. Premature
infant responses to noise reduction by earmuffs: Effects on
behavioral and physiologic measures. J Perinatol.
1995;15:448-55.
12. Li WG, Jiang HB, Gan T, et al. Effect of noise on the
auditory system and the intelligence development of premature
infants treated in the neonatal intensive care unit. Zhongguo
Dang Dai Er Ke Za Zhi. 2009;11:976-9 [Chinese].
|

