|
|
|
Indian Pediatr 2020;57:926-928 |
 |
Validation of the
Testicular Workup for Ischemia and Suspected Torsion (TWIST)
Score in the Diagnosis of Testicular Torsion in Children With
Acute Scrotum
|
|
Pradyumna Pan
From Pediatric Surgery Unit, Ashish Hospital and Research Centre,
Jabalpur, Madhya Pradesh, India.
Correspondence to: Dr Pradyumna Pan, Pediatric Surgery Unit, Ashish
Hospital and Research Centre, Jabalpur, Madhya Pradesh, India.
Email: [email protected]
Received: November 04, 2019;
Initial review: January 23, 2020;
Accepted: August 22, 2020
|
Objective: To validate the
Testicular Workup for Ischemia and Suspected Torsion (TWIST) score for
the evaluation of children presenting with acute scrotum. Methods: This
prospective study calculated TWIST score in patients of acute scrotum
admitted to a pediatric surgery unit. The scoring system consisted of
testicular swelling (2 points), hard testicle (2), absent cremasteric
reflex (1), nausea/vomiting (1) and high-riding testis (1). All the
patients were examined by a pediatric surgeon. Results: Among 96
children with acute scrotum, 68 (70.8%) patients had testicular torsion.
In the testicular torsion group, the mean (SD) TWIST score was 5.7 (1.2)
and in no torsion group, it was 1.46 (0.67). In the testicular torsion
group, the number of patients with low, intermediate, and high risk was
0, 13, and 55, respectively and in without testicular torsion these were
21, 7, and 0, respectively. Conclusions: TWIST score has high
predictive value for testicular torsion, and can be used for clinical
diagnosis of testicular torsion.
Keywords: Color doppler, Management, Orchidectomy, Spermatic
cord torsion.
|
|
T
esticular torsion is the most common
pediatric urological emergency, affecting 3.8 per 100,000 males
younger than 18 years annually [1]. Around 10-5% of these are
children with acute scrotal disease [2], and results in a 42%
orchiectomy rate for boys undergoing testicular torsion surgery.
Testicular salvage requires timely detection and treatment, and
torsion should be excluded in all patients with acute scrotum.
Doppler ultrasound (DUS) has been considered as the primary
imaging method for the assessment of testicular torsion with
high sensitivity and specificity [3]. However, for those with
testicular torsion, the use of DUS can prolong the time in
testicular ischemia and delay surgery. The availability of
radiological imaging and the expertise of its operators and
evaluators are also limited in many settings. Barbosa, et al.
[4] developed a Testicular Workup for Ischemia and Suspected
Torsion (TWIST) score based on clinical parameters
[4]. Typically, there is a 4-8 hour window before permanent
ischemic damage to testes occurs. Treatment delays may be
associated with reduced fertility or may require orchiectomy.
The purpose of this study is to study the utility of the TWIST
scoring system for testicular torsion in boys presenting to the
emergency room (ER) with an acute scrotum.
METHODS
This observational study was carried over a
period of two years (May, 2017 to April, 2019) in a tertiary
referral centre. Institutional review board and ethical
committee approval were obtained. Participants included were
males aged 0 days to 18 years, presenting to ER with chief
complaint of testicular pain and/or swelling. Patients were
excluded if their pain was due to trauma, if symptoms were
present for greater than one week, there was a history of
testicular disease or surgery, and if a diagnosis of testicular
torsion had already been confirmed or excluded.
The TWIST score is based on the sum (ranging
from 0 to 7) of the following findings: testicular swelling (2
points), hard testicle (2 points), absent cremasteric reflex (1
point), nausea or vomiting (1 point), and high riding testicle
(1 point) [4]. The risk stratifying scores for those at low risk
for testicular torsion is 0 to 2 points, inter-mediate risk was
3 to 4 points, and high risk for testicular torsion is 5 to 7
points [4]. The primary conclusion was a diagnosis of testicular
torsion by TWIST score, con-firmed by surgical exploration as
the final diagnosis. Testicular loss was defined as either
surgical orchiectomy or determination of significant atrophy at
6 months post-operative ultrasound. A more than 50% difference
in volume compared with the contralateral testis or absence of
blood flow on Doppler was considered to represent testicular
loss [5].
The TWIST score was performed by a single
pediatric surgeon in all patients, and surgery was carried out
by the same surgeon. The same sonologist did the DUS evaluation
in all patients. Indication of surgery was impaired blood flow
in DUS, and inability to rule out testicular torsion in the
presence of intermediate TWIST score. All patients for whom
surgery was indicated were immediately transferred to the
operating room for scrotal exploration. All patients who
underwent surgical exploration had confirmed diagnoses of
testicular torsion.
RESULTS
A cohort of 96 males with acute scrotum was
studied. The mean age of the patients in the study group was
10.1 (3.8) years (range 1 month-16 year). The TWIST score
component and other clinical features are shown in Table
I.
Table I Clinical Features of Children With Acute Scrotum (N=96)
|
Characteristic |
Torsion
|
Non torsion |
|
(n=68) |
(n=28) |
|
Testicular pain |
65 (95.6) |
26 (92.9) |
|
Nausea and vomiting |
65 (95.6) |
26 (92.9) |
|
Abdominal pain |
21 (30.9) |
9 (32.2) |
|
Tenderness |
29 (42.7) |
7 (25.0) |
|
Testicular swelling |
27 (39.7) |
7 (25.0) |
|
High riding testes |
55 (80.9) |
0
|
|
Absent cremasteric reflex |
65 (95.6) |
0 |
|
Hard testicle |
41 (60.3) |
6 (21.4) |
|
Erythema |
16 (23.5) |
1 (3.6) |
|
All values in no. (%); *P<0.01, #P<0.01, P=0.02. |
Table II Testicular Workup for Ischemia and Suspected Torsion (TWIST) Score
in Children With Acute Scrotum (N=96)
|
Risk group |
Twist |
Testicular |
No testicular
|
|
score |
torsion (n=68) |
torsion (n=28)
|
|
Low |
0-2 |
0
|
21 (75) |
|
Intermediate |
3-4 |
13 (19.2) |
7 (25) |
|
High |
5-7 |
55 (80.8) |
0 |
|
All values in no. (%). |
In the testicular torsion group, the mean
TWIST score was 5.7 (1.2 ) (range 3-7), and in no torsion group,
it was 1.46 (0.67 ) (range 0-4). In testicular torsion group,
the number of patients with low, intermediate, and high risk was
0, 13, and 55, respectively, while the number of patients
without testicular torsion was 21, 7, and 0 in low,
intermediate, and high-risk groups, respectively (Table
II). Doppler ultrasound was obtained in all study subjects,
which diagnosed testicular torsion in 65 patients. Three
patients had equivocal ultrasound, showing no definite torsion
with a lack of vascular flow, and neither increased blood flow
to the epididymis. These patients were surgically proven to have
testicular torsion on exploration. Thus, 68 (70.8%) patients
were found to have testicular torsion. The 6-month follow-up DUS
showed 46 equal sized and normal blood flow testes on both
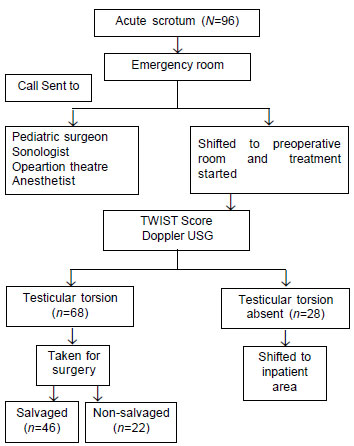
sides, with a salvage rate of 67.6% (Fig. 1).
 |
|
Fig. 1 Flowchart of
patients with acute scrotum enrolled in the study.
|
DISCUSSION
This current study validates the TWIST score,
which risk stratifies patients presenting with an acute scrotum
for testicular torsion. There were no patients with torsion in
the low-risk category (0-2 twist score), and 100% of patients in
the high-risk category (5-7 twist score) had torsion. In this
analysis, the TWIST score was found to be an excellent
diagnostic tool in the diagnosis of testicular torsion, which is
comparable to other studies [4,6,7]. In this study, all low-risk
and high-risk patients (73.9 %) could have avoided the use of an
ultrasound scan.
The original TWIST study included no patients
with torsion (0/51) in the low-risk category and all 22 patients
with torsion in the high-risk category [4]. Barbosa, et al.
[4] found that only 20% of patients are in the
intermediate-risk group and recommended that DUS is required
only in this group. The testicular torsion scoring systems are
now being tested in non-urologic medical providers [8] and
reducing time delays, costs and reliance on DUS [9]. The TWIST
score is intended to categorize patients requiring an
ultrasound. This score is not designed to substitute doppler
sonography [4]. Sheth, et al. [6] assessed TWIST score in
non-pediatric surgery-trained emergency room caregivers
diagnosing testicular torsion and found it equally effective.
The absence of cremasteric reflex and high riding rotated testes
are sufficiently reliable for the diagnosis of testicular
torsion, as also reported by other authors [10,11].
In this analysis, the main limitations were
the small number of cases observed. The TWIST score was evalua-ted
by a single examiner. At least two examiners should have perform
the physical examination, thus providing information on
inter-observer variation.
In conclusion, this study has demonstrated
that the TWIST score is reliable to identify testicular torsion
in patients with acute scrotum. Since this study was conducted
in one hospital, studies in multiple settings will support the
internal validity of this method.
Ethics clearance: Institutional Ethics
Committee; No. 17/ASH/Study 03/2017, dated January 01, 2017.
Contributors: PP: developed the concept
and designed the study, collected and analyzed the data, drafted
the manuscript.
Funding: None; Competing interest:
None stated.
|
WHAT THIS STUDY ADDS?
TWIST score categorizes
the patient with acute scrotum, and may be useful in
situations where ultrasound facility is not available.
|
REFERENCES
1. Zhao LC, Lautz TB, Meeks JJ, Maizels M.
Pediatric testicular torsion epidemiology using a national
database: Incidence, risk of orchiectomy and possible measures
toward improving the quality of care. J Urol. 2011;186: 2009-13.
2. McAndrew HF, Pemberton R, Kikiros CS,
Gollow I. The incidence and investigation of acute scrotal
problems in children. Pediatr Surg Int. 2002;18:435-37.
3. Yazbeck S, Patriquin HB. Accuracy of
doppler sonography in the evaluation of acute conditions of the
scrotum in children. J Pediatr Surg.1994;29:1270-72.
4. Barbosa JA, Tiseo BC, Barayan GA, Rosman
BM, Torricelli FC, Passerotti CC, et al. Development and
initial validation of a scoring system to diagnose testicular
torsion in children. J Urol. 2013;189:1859-64.
5. Figueroa V, Pippi Salle JL, Braga LH,
Romao R, Koyle MA, Bagli DJ, et al. Comparative analysis
of detorsion alone versus detorsion and tunica albuginea
decompression (fasciotomy) with tunica vaginalis flap coverage
in the surgical management of prolonged testicular ischemia. J
Urol. 2012; 188:1417-22.
6. Sheth KR, Keays M, Grimsby GM, Granberg
CF, Menon VS, DaJusta DG, et al. Diagnosing testicular
torsion before urological consultation and imaging: Validation
of the TWIST score. J Urol. 2016;195:1870-6.
7. Frohlich LC, Darian NP, Cilento BC, Lee
LK. Prospective validation of clinical score for males
presenting with an acute scrotum. Acad Emerg Med.
2017;24:1474-82.
8. Afsarlar CE, Ryan SL, Donel E, Baccam TH,
Jones B, Chandwani B, et al. Standardized process to
improve patient flow from the emergency room to the operating
room for pediatric patients with testicular torsion. J Pediatr
Urol. 2016;12:233-36.
9. Boettcher M, Krebs T, Bergholz R, Wenke K,
Aronson D, Reinshagen K. Clinical and sonographic features
predict testicular torsion in children: A prospective study. BJU
Internat. 2013;112:1201-6.
10. Ciftci AO, S enocak ME, Tanyel FC,
Büyükpamukçu N. Clinical predictors for differential diagnosis
of acute scrotum. Eur J Pediatr Surg. 2004;14:333-8.
11. Tariq OA, Mohammed A, Abdelrahman A,
Vishwanatha K, Prem C, Abdulla A, et al. Suspected
testicular torsion in children: Diagnostic dilemma and
recommendation for a lower threshold for initiation of surgical
exploration. Res Report Urol. 2018;10:241-9.
|
|
|
 |
|

