Mortality
in children with epilepsy is significantly higher than the
general population [1]; although, most deaths in children with
epilepsy are not related to seizures or epilepsy [2]. The higher
risk is explained by several factors: respiratory illness with
underlying neurological condition that presents with seizures,
systemic comorbidities, indirect factors as well as deaths
presumably or demonstrably due to seizures. Sudden unexpected
death in epilepsy (SUDEP), which belongs to the last group, has
gained prominence as a cause of death in epilepsy in recent
years.
DEFINITION
SUDEP is
defined as a “sudden unexpected witnessed or unwitnessed,
non-traumatic, non-drowning death in a patient with epilepsy
with or without evidence of a seizure and excluding documented
status epilepticus in which post-mortem examination does not
reveal a toxicological or anatomical cause of death [3].’’ This
definition requires a postmortem examination to diagnose SUDEP,
which is not available in the majority of instances. Hence,
criteria have been described for definite, probable and possible
SUDEP [4] (Box I).
|
Box I Classification and Definition of Subtypes
of Sudden Unexpected Death in Epilepsy (SUDEP) |
Definite SUDEP
• Sudden, unexpected, witnessed
or unwitnessed, non-traumatic and non-drowning death,
occurring in benign circumstances, in an individual with
epilepsy, with or without evidence for a seizure, and
excluding documented status epilepticus in which
postmortem examination does not reveal a cause of death.
Probable SUDEP
• Same as definite SUDEP
but without autopsy. The victim should have died
unexpectedly while in a reasonable state of health,
during normal activities, and in benign circumstances,
without a known structural cause of death.
Possible SUDEP
• SUDEP cannot be ruled out but a
competing cause of death is present. If a death is
witnessed, a cutoff of death within one hour from acute
collapse is suggested.
|
BURDEN
The incidence
rates of SUDEP in children have been reported to be 0.36-0.43
per 1000 person-years [5-7]. Although SUDEP rates have been
reported to be lower in children compared to adults, the
American Academy of Neurology (AAN) practice guidelines on SUDEP
established the incidence rate of SUDEP in children with
epilepsy to be 0.22/1000 patient–years (95% CI 0.16-0.31) after
a systematic review of 12 class I studies [8]. Due to
imprecision in incidence data results, random-effect
meta-analysis was further performed. SUDEP was found to affect 1
in 4,500 children with epilepsy in one year, making the risk of
SUDEP rare.
Risk
Predictors
There are very
few studies assessing risk factors in childhood SUDEP and most
of the data is derived from larger studies in adults.
•
The presence
and frequency of generalized tonic-clonic seizures (GTCS) is an
important risk predictor for SUDEP [8].
•
The relative
risk of SUDEP is 7.7 times higher in patients with onset of
epilepsy between 0-15 years compared to onset after the age of
45 years [9].
•
All-cause
mortality, including SUDEP, is also higher in children with
developmental delay [10].
•
Children
with uncontrolled seizures have a higher risk [11].
•
SUDEP has
also been shown to increase with the duration and severity of
seizures, with 15-fold risk with more than 50 GTCS per year,
nocturnal seizures and the occurrence of GTCS [12], as well as
prolonged tonic state leading to post-ictal immobility [13].
•
Postictal
generalized EEG suppression beyond 50 seconds also may have a
predictive role in SUDEP and is associated with sleep, shorter
duration of clonic phase, symmetric tonic extension posturing
and terminal burst-suppression after a seizure [14].
•
Symptomatic
epilepsy has a higher risk of SUDEP compared to idiopathic
generalized epilepsy.
Patients with Dravet syndrome are also at a higher risk
of death [15].
SUDEP shares certain features
with the syndrome of sudden infant death (SIDS), suggesting
possible common mechanisms. SIDS is sudden and unexpected death
that occurs in infants below the age of one year. Both SIDS and
SUDEP are diagnoses of exclusion, and autopsy findings are
usually not revelatory. Deficiency in arousal response to rise
in carbon dioxide in both syndromes may contribute to death,
suggesting that these two entities may lie on a continuum [16].
PATHOPHYSIOLOGY
The
pathophysiology of SUDEP is not well elucidated and is believed
to arise from an interaction between predisposing factors and
triggers. Predisposing factors include effects of long-standing
seizure disorder such as altered autonomic function, etiology of
epilepsy (e.g. symptomatic, familial), factors related to
drug therapy such as abrupt withdrawal or polypharmacy etc.
A triggering seizure leads to preterminal events including
cardiac, respiratory, autonomic and cerebral dysfunction. The
various mechanisms (Fig. 1) include the following:
Cardiac dysfunction:
Sudden cardiac arrest is a proposed mechanism with certain ion
channel abnormalities being implicated in both epilepsy and
cardiac arrhythmia. The most widely implicated is the sodium
channel abnor-mality, which may also explain the higher rates of
SUDEP in Dravet syndrome [17]. Another link is the association
between long QT syndrome and familial epilepsies, both of which
are channelopathies.
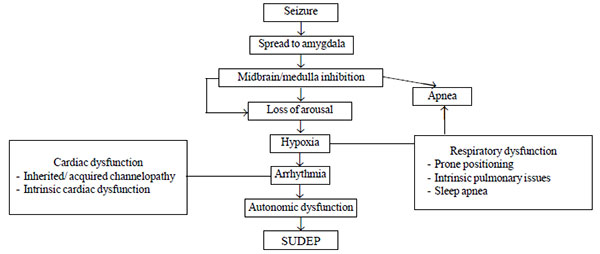 |
| Fig. 1 Various pathophysiological
mechanisms leading to sudden unexpected death in
epilepsy (SUDEP). |
Respiratory dysfunction:
Severe peri-ictal hypoxia occurs in one-fourth of patients with
SUDEP [17]. Autopsy changes of pulmonary edema have also been
observed in SUDEP cases, but this is likely an effect than a
cause of SUDEP.
Autonomic dysfunction:
Various autonomic abnor-malities have been described in patients
with refractory epilepsy and include lower parasympathetic and
higher sympathetic tone, increased vasomotor tone and impaired
heart rate variability [18]. Changes in ictal heart rate also
suggest autonomic dysfunction, with tachycardia occur-ring in up
to 60% of seizures and bradycardia in 6% of focal seizures
[17,19]. As per the Mortality in epilepsy monitoring units study
(MORTEMUS), an initiative that assessed cases of SUDEP and
near-SUDEP in patients admitted for video-EEG monitoring,
post-ictal centrally mediated cardiac and respiratory depression
associated with post-ictal generalized EEG suppression was a
strong mechanism leading to SUDEP [20]. The switch from
parasympathetic to sympathetic state, combined with sympathetic
over-drive that accompanies the state of drug withdrawal that
accompany seizures may be a possible precipitant.
Channelopathies:
Channelopathies are disorders characterised by dysfunction of
ion channels. Traditio-nally channelopathies have been
considered genetic defects eg., long QT syndrome and
Dravet syndrome. In inherited channelopathies, the same ion
channel abnormalities are expressed in the heart as well as the
brain. Hence, these epilepsies are associated with an
arrythmia-prone cardiac condition.
Recently,
there is an emerging concept of acquired channelopathy i.e.,
channel dysfunction in patients with chronic epilepsy. Animal
studies have shown that epilepsy alters the expression of
sodium, potassium, calcium and cationic channels in the heart.
In these acquired cardiac channelopathies, epilepsy increases
the pro-arrhythmic state increasing predisposition to sudden
death [21].
Cerebral dysfunction:
SUDEP occurs more often in sleep and almost all cases are
nocturnal and associated with the prone position. Various
neurotransmitter abnormalities have been reported in association
with SUDEP including low serotonin state [22] and excessive
opioid [23] and adenosine activity. Brainstem serotonin
modulates respiratory drive and has also been implicated in
sudden infant death syndrome [24]. It may contribute to SUDEP by
a similar mechanism.
INTERVENTIONS FOR PREVENTION
As
uncontrolled epilepsy is a known risk factor, effective epilepsy
treatment to reduce frequency and duration of seizures as well
as GTCS should be targeted. Nocturnal supervision was found to
be protective in one case-control study [25] and may be combined
with seizure detection devices, but clinching evidence in SUDEP
prevention is lacking. It is of potential benefit in children
with uncontrolled or nocturnal seizures. In India, nocturnal
supervision of children is generally culturally acceptable as
co-sleeping of children with their parents is common. A blanket
‘back to sleep’ advice to avoid prone positioning may be
recommended, with the caveat that it is the post-ictal turning
prone which is usually responsible. Hence parents should be
counseled to turn the child to a lateral position and avoid
prone position after the seizure. The use of lattice or safety
pillows may reduce the contribution of prone position to
post-ictal cardiorespiratory distress.
In terms
of preventive drug therapy, it has been observed in mouse models
of SUDEP that selective serotonin reuptake inhibitors (SSRI)
such as fluoxetine may decrease apnea risk [26]. Serotonergic
neurons in the brainstem are believed to be responsive to rise
in CO2 and fall in pH levels in
the blood and thereby stimulate respiration and arousal. In a
retrospective study on adults with focal seizures [27], it was
noted that patients on SSRIs (for co-morbid mental health
problems) had a reduced likelihood of post-ictal oxygen
desaturation as compared to patients who were not on SSRIs.
Recently, two randomized controlled trials have been completed
to evaluate the role of fluoxetine to prevent post-seizure
apneas and desaturation; however, the results have not been
published yet. Massive release of endogenous opioids and
adenosine is induced by seizures and helps in seizure
termination [28]. However, this surge can also lead to
post-ictal apnea. Naloxone is currently under a randomized trial
for this purpose. Adenosine antagonists may also be beneficial
for this purpose.
These therapies; however, are
still in the emerging phase and currently being tried in adults.
More evidence is needed before the data can be extrapolated to
children.
Parental
Counseling
Counseling of
caregivers and sensitization towards SUDEP is imperative.
Caretakers should be educated regarding the importance of
adherence to treatment, nocturnal supervision, especially to
avoid prone position after seizures, as well as basic life
support training imparted to willing caregivers. However,
whether all patients with epilepsy should be counseled about the
risk of SUDEP or only high-risk patients remains a matter of
debate, and scientific data till date does not permit the
establishment of evidence-based guidelines for the same.
However, disclosure of SUDEP risk to all epilepsy patients has
been endorsed by multiple neurological societies, including a
joint task force of the American Epilepsy Society and the
Epilepsy Foundation and the American Academy of Neurology (AAN)
[29], and in India by the joint consensus document on parental
counseling by Association of Child Neurology (AOCN) and Indian
Epilepsy Society (IES) [30]. In a study on parental views
regarding the counseling of SUDEP risk, parents generally
expressed a preference for receiving routine SUDEP counseling at
the time of the diagnosis of epilepsy [31]. In another study
from Malaysia (32% of participants were of Indian origin), 70.9%
of parents felt that receiving SUDEP information was positive
[32]. Most parents did not report any impact on their own
functioning. However, increasing numbers over time reported an
impact on the child’s functioning. In a study from UK, 74% of
pediatric neurologists conveyed SUDEP information to a select
group of patients only. In contrast, 94% of parents of children
with epilepsy expected the physician to provide SUDEP
information [33].
In India, many neurologists and
pediatricians feel that imparting the knowledge of SUDEP may
increase parental anxiety and stress levels, which may be
unwarranted as the complication is so rare. However, it is also
known that many parents are afraid their child would die when
they witness the child having a seizure for the first time. The
information that the risk of death is very low may be
reassuring. Also, the knowledge of this condition may improve
drug compliance, as seen in studies from outside India. In an
Indian study of SUDEP counseling of adults with epilepsy and
their caregivers, it was shown to increase drug adherence
without any increase in anxiety or stress levels in either the
patients or their caregivers [34]. More experience is needed in
this field to understand parental perceptions and reactions.
CONCLUSION
SUDEP is an
under-recognized but important threat in patients with epilepsy.
It is important to assess SUDEP risk in all epilepsy patients,
particularly in those with generalized tonic-clonic convulsions,
nocturnal seizures, as well as co-morbid developmental delay.
Appropriate antiepileptic drug therapy with stress on
compliance, early surgical referral for surgically remediable
epilepsies, avoiding post-seizure prone positioning, and
caretaker counseling and support will go a long way in the
prevention of this condition.
Contributors:
DG performed the literature review and wrote the first draft
which was critically revised by SS. Both authors approved the
final version of the submitted manuscript.
Funding:
None;
Competing interest: None stated.
REFERENCES
1. Appleton R. Mortality in
paediatric epilepsy. Arch Dis Child. 2003;1091-4.
2. Gaitatzis A, Johnson AL,
Chadwick DW, Shorvon SD, Sander JW. Life expectancy in people
with newly diagnosed epilepsy. Brain. 2004;127:2427-32.
3. Nashef L. Sudden
unexpected death in epilepsy: Terminology and definitions.
Epilepsia. 1997;38:S6-8.
4. Nashef L, E. So P.
Ryvlin T. Tomson. Unifying the definitions of sudden unexpected
death in epilepsy. Epilepsia. 2012;53:227-33.
5. Sillanpää M, Shinnar S.
Long-term mortality in childhood-onset epilepsy. N Engl J Med.
2010;363:2522-9.
6. Weber P, Bubl R,
Blauenstein U, Tillmann BU, Lütschg J. Sudden unexplained death
in children with epilepsy: A cohort study with an eighteen-year
follow-up. Acta Paediatr. 2005;94:564-7.
7. Sillanpää M, Shinnar S.
SUDEP and other causes of mortality in childhood-onset epilepsy.
Epilepsy Behav. 2013;28:249-55.
8. Harden C, Tomson T,
Gloss D, Buchhalter J, Cross JH, Donner E, et al.
Practice Guideline Summary: Sudden Unexpected Death in Epilepsy
Incidence Rates and Risk Factors. Report of the Guideline
Development, Dissemi-nation, and Implementation Subcommittee of
the American Academy of Neurology and the American Epilepsy
Society. Neurology. 2017;88:1674-80.
9. Berg AT, Nickels K,
Wirrell EC, Geerts AT, Callenbach PM, Arts WF, et al.
Mortality risks in new-onset childhood epilepsy. Pediatrics.
2013;132:124-31.
10. Shinnar S, Pellock JM.
Update on the epidemiology and prognosis of pediatric epilepsy.
J Child Neurol. 2002; 17: S4-S17.
11. Nickels KC, Grossardt
BR, Wirrell EC. Epilepsy-related mortality is low in children: A
30-year population-based study in Olmsted County, MN. Epilepsia.
2012;53:2164-71.
12. Hesdorffer DC, Tomson
T, Benn E, Sander JW, Nilsson L, Langan Y, et al.
Combined analysis of risk factors for SUDEP. Epilepsia.
2011;52:1150-9.
13. Tao JX, Yung I, Lee A,
Rose S, Jacobsen J, Ebersole JS. Tonic phase of a generalized
convulsive seizure is an independent predictor of postictal
generalized EEG suppression. Epilepsia. 2013;54:858-65.
14. Lamberts RJ, Gaitatzis
A, Sander JW, Elger CE, Surges R, Thijs RD. Postictal
generalized EEG suppression: An inconsistent finding in people
with multiple seizures. Neurology. 2013; 81:1252-6.
15. Skluzacek JV, Watts KP,
Parsy O, Wical B, Camfield P. Dravet syndrome and parent
associations: The IDEA League experience with comorbid
conditions, mortality, management, adaptation, and grief.
Epilepsia. 2011;52:95-101.
16. Buchanan GF. Impaired
CO2-induced
arousal in SIDS and SUDEP. Trend Neurosci. 2019:42:242-50.
17. Moseley BD, Wirrell EC,
Nickels K, Johnson JN, Ackerman MJ, Britton J.
Electrocardiographic and oximetric changes during partial
complex and generalized seizures. Epilepsy Res. 2011;95:237-45.
18. Mukherjee S, Tripathi
M, Chandra PS, Yadav R, Choudhary N, Sagar R, et al.
Cardiovascular autonomic functions in well-controlled and
intractable partial epilepsies. Epilepsy Res. 2009;85:261-9.
19. Zijlmans M, Flanagan D,
Gotman J. Heart rate changes and ECG abnormalities during
epileptic seizures: Prevalence and definition of an objective
clinical sign. Epilepsia. 2002;43:847-54.
20. Ryvlin P, Nashef L,
Lhatoo SD, Bateman LM, Bird J, Bleasel A, et al.
Incidence and mechanisms of cardio-respiratory arrests in
epilepsy monitoring units (MORTEMUS): A retrospective study.
Lancet Neurol.
2013;12:966-77.
21. Li MCH, O’Brien
TJ,Todaro M, Powell KL. Acquired cardiac channelopathies in
epilepsy: Evidence, mechanisms and clinical significance.
Epilepsia. 2019:60: 1753-67.
22. Toczek MT, Carson RE,
Lang L, Ma Y, Spanaki MV, Der MG, et al. PET imaging of
5HT1A receptor binding in patients with temporal lobe epilepsy.
Neurology. 2003;60:749-56.
23. Tortella FC, Long JB,
Holaday JW. Endogenous opiate systems: Physiological role in the
self-limitation of seizures. Brain Res. 1985;332:174-8.
24. Paterson DS,
Trachtenberg FL, Thompson EG, Belliveau RA, Beggs AH, Darnall R,
et al. Multiple serotonergic abnormalities in sudden
infant death syndrome. JAMA. 2006;296:254-32.
25. Langan Y, Nashef L,
Sander JW. Case-control study of SUDEP. Neurology.
2005;64;1131-3.
26. Faingold CL, Tupal S,
Randall M. Prevention of seizure-induced sudden death in a
chronic SUDEP model by semichronic administration of a selective
serotonin reuptake inhibitor. Epilepsy Beh. 2011;22:186-90.
27. Bateman LM, Li CS, Lin
TC, Seyal M. Serotonin reuptake inhibitors are associated with
reduced severity of ictal hypoxemia in medically refractory
partial epilepsy. Epilepsia. 2010;51:2211-4.
28. Volpicelli JR, Alterman
AI, Hayashida M, O’Brien CP. Naltrexone in the treatment of
alcohol dependence. Arch Gen Psych. 1992;49:876-80.
29. Maguire MJ, Jackson CF,
Marson AG, Nolan SJ. Treatments for the prevention of sudden
unexpected death in epilepsy (SUDEP). Cochrane Database Syst
Rev. 2016;7:CD011792.
30. Srivastava K, Sehgal R,
Konanki R, Jain R, Sharma S, Mittal R. Association of Child
Neurology-Indian Epilepsy Society Consensus Document on Parental
Counseling of Children with Epilepsy. Indian J Pediatr.
2019;86:608-16.
31. Ramachandrannair R,
Jack SM, Meaney BF, Ronen GM. SUDEP: What do parents want to
know? Epilepsy Beh. 2013;29:560-4.
32. Fong CY, Lim WK, Kong
AN, Lua PL, Ong LC. Provision of sudden unexpected death in
epilepsy (SUDEP) information among Malaysian parents of children
with epilepsy. Epilepsy Behav. 2017;75:6-12.
33. Gayatri NA, Morrall MC,
Jain V, Kashyape P, Pysden K, Ferrie C. Parental beliefs
regarding the provision and content of written sudden unexpected
death in epilepsy (SUDEP) information. Epilepsia.
2010;51:777-82.
34. Radhakrishnan DM,
Ramanujam B, Srivastava P, Dash D, Tripathi M. Effect of
providing sudden unexpected death in epilepsy (SUDEP)
information to persons with epilepsy (PWE) and their caregivers
experience from a tertiary care hospital. Acta Neurol Scand.
2018;138:417-24.

