|
|
|
Indian Pediatr 2019;56: 885-887 |
 |
Investigating the Muzaffarpur Outbreaks in the Backdrop of
Western Uttar Pradesh Experience: The Way Forward
|
|
Vipin M Vashishtha
Director and Consultant Pediatrician, Mangla Hospital
and Research Center, Shakti Chowk, Bijnor, Uttar Pradesh, India.
Email:
vipinipsita@gmail.com
|
|
The death of more than 130 children in Muzaffarpur, Bihar during the
summer months of 2019 due to Acute encephalitis syndrome (AES) has
raised an intense debate on the probable etiology of the killer disease.
The recurrent outbreaks of the disease are reported since 1995, and
several attempts have already been made by the different teams to clinch
the exact etiology [1,2]. The key recent investigations were performed
by three sets of expert-groups – John, et al. [3], the Natioal
Center for Disease Control (NCDC), India, and Centre for Disease Control
(CDC), United State (US) group [4], and by the pediatrician
in-charge of Shri Krishna Medical College Hospital (SKMCH), Muzaffarpur
[5]. While the first two groups identified litchi toxins, namely
methylene cyclopropylglycine (MCPG) and methylene cyclopropy-lalanine
(MCPA or hypoglycin A), responsible for the development of an acute
hypoglycemic encephalopathy (AHE) amongst malnourished, poor, rural
children [3,4], the latter suggested extremely high environmental
temperature and humidity in the region resulting in ‘heat stroke’ that
led to encephalopathy [5]. Due to the lack of documented hyperpyrexia in
all the cases, and early morning onset of symptoms, there were few
takers for the heat stroke theory. The litchi-toxins theory was more
acceptable and the Bihar State Health Ministry started following the
preventive measures as suggested by the groups who put forward this
theory. The number of cases and deaths declined sharply in the following
four years, 2015 to 2018 only to resurface in a much significant number
in 2019.
A previous similar recurrent epidemic in many
districts of Western Uttar Pradesh (UP), the so-called ‘Saharanpur
encephalitis’ [6], was investigated by an independent group of
investigators and the etiology was identified as toxicity due to oral
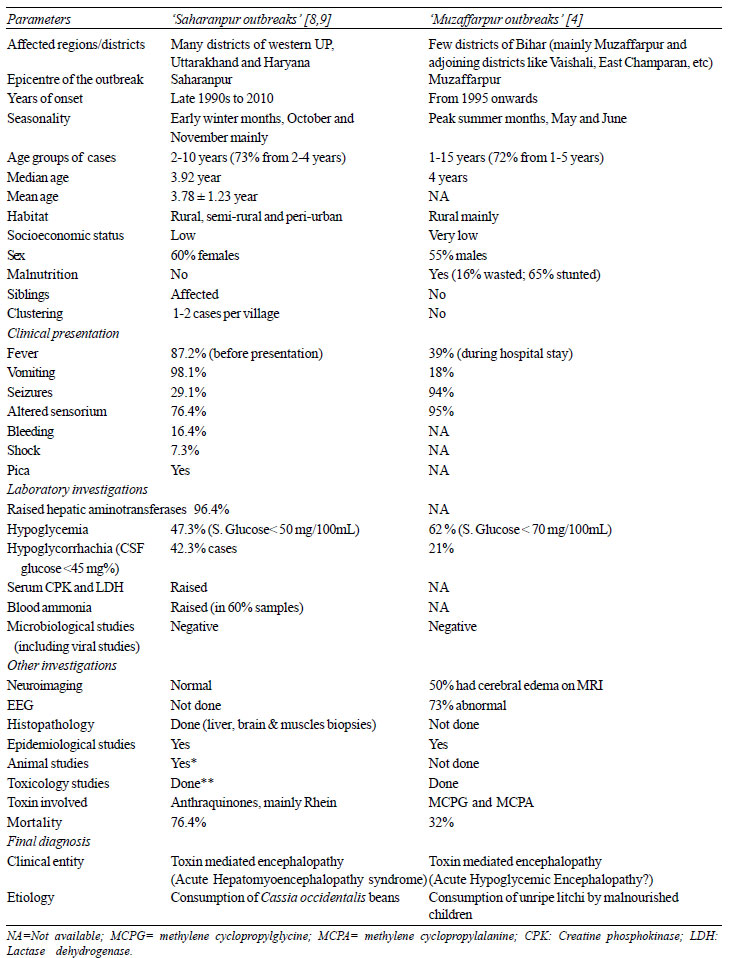
ingestion of a local weed [7]. There are many similarities between the
western UP and Muzaffarpur outbreaks; yet the approach, investigations
and the outcomes are quite different (Table I).
|
TABLE I Comparative Analysis of
Investigations of Western UP Aka ‘Saharanpur’ and ‘Muzaffarpur’
Outbreaks
|
 |
In the Western UP outbreak, step-wise investigation
approach was adopted and as a first step a proper ‘case definition’ with
exclusion and inclusion criteria was formed. Based on its strict
application, the disease was initially identified as an encephalopathy
[6]. The next step was the histopathological examination of few target
organs, which hinted toward toxin-mediated necrosis of liver and muscles
(thus the term (acute hepato-myoencephalopathy (HME) syndrome) [6,7].
The differences in approaches in the two outbreak investi-gations are
presented in (Table I).
With the re-emergence of the outbreak in Muzaffarpur
this year, the debate on the exact etiology has reignited. While the
role of any microbiological agent as the main trigger has been abandoned
by most investigators, the focus is now on the litchi toxins and heat
stroke as probable theories. Despite many ‘missing links’ like
inconsistent findings of hypoglycemia and hyperthermia, lack of profuse
vomiting (a hallmark of MCPA toxicity), ‘mismatched’ seasonality
(paucity of unripe fruits at the peak of the outbreaks when the entire
crop is matured), no clarity on toxic levels (LD50) of toxins that cause
dose-dependent toxicity, occurrence in children too young to eat the
fruit, lack of hepatic dysfunctions despite mitochondrial involvement,
flawed selection of controls in case-control study, lack of study of
toxins in the body fluids of healthy siblings and peers living in the
same household or village, the doubtful role of rapid correction of
hypoglycemia on prevention of deaths, the litchi toxin theory was
considered as the most plausible one.
A detailed case-control study in western UP helped in
identifying the putative toxin which turned out to be anthraquinone
derivatives contained in the beans of the weed, Cassia occidentalis
[7]. Previous published literature confirmed the biological
plausibility of causation in vertebrates. The cause-effect relationship
of the Cassia occidentalis with acute HME syndrome in Wistar rats
was subsequently demonstrated [8]. These detailed studies also helped in
further outbreaks like the one in Sylhet, Bangladesh (2007-08) [9] and
another in Malkangiri, Orissa (2016).
Currently, the outbreak investigations in India are
at the crossroads. The need is to conduct investigations which
are detailed and comprehensive, and performed in a coordinated and
step-wise manner without any fixed notion.
References
1. Yewale VN. Misery of mystery of Muzaffarpur.
Indian Pediatr. 2014;51:605-6.
2. Vashishtha VM. Encephalitis outbreaks in
Muzaffarpur: Five blind men describing an elephant! Indian Pediatr.
2014; 51:936.
3. John TJ, Das M. Acute encephalitis syndrome in
children in Muzaffarpur: hypothesis of toxic origin. Curr Sci
2014;106:1184-5.
4. Shrivastava A, Kumar A, Thomas JD, Laserson KF,
Bhushan G, Carter MD, et al. Association of acute toxic
encephalopathy with litchi consumption in an outbreak in Muzaffarpur,
India, 2014: A case-control study. Lancet Glob Health. 2017;5:e458-e466.
5. Sahni GS. Recurring epidemics of acute
encephalopathy in children in Muzaffarpur, Bihar. Indian Pediatr
2012;49:502-03.
6. Vashishtha VM, Nayak NC, John TJ, Kumar A.
Recurrent annual outbreaks of a hepato-myo-encephalopathy syndrome in
children in western Uttar Pradesh, India. Indian J Med Res. 2007;125:523-33.
7. Vashishtha VM, Kumar A, John TJ, Nayak NC.
Cassia occidentalis poisoning causes fatal coma in children in
western Uttar Pradesh. Indian Pediatr 2007; 44:522-5.
8. Panigrahi G, Tiwari S, Ansari KM, Chaturvedi RK,
Khanna VK, Chaudhari BP, et al. Association between children
death and consumption of Cassia occidentalis seeds: clinical and
experimental investigations. Food Chem Toxicol. 2014;67:236-48.
9. Gurley ES, Rahman M, Hossain MJ, Nahar N, Faiz MA,
Islam N, et al. Fatal outbreak from consuming Xanthium strumarium
seedlings during time of food scarcity in northeastern Bangladesh. PLoS
One. 2010;5:e9756.
|
|
|
 |
|

