|
|
|
Indian Pediatr 2018;55:
909-910 |
 |
Milky
Mesentery: Acute Abdomen with Chylous Ascites
|
|
Aakanksha Goel, Manish Kumar Gaur and Pankaj Kumar Garg
From Department of Surgery, University College of
Medical Sciences and Guru Teg Bahadur Hospital, Shahdara, Delhi, India.
Correspondence to: Dr Aakanksha Goel, House No 1 Sukh
Vihar, Delhi 110 051, India.
Email:
[email protected]
Received: July 21, 2017;
Initial Review: December 26, 2017;
Accepted: May 24, 2018.
|
Background: Clinical presentations of intestinal
lymphangiectasia include pitting edema, chylous ascites, pleural
effusion, diarrhea, malabsorption and intestinal obstruction. Case
Characteristics: An 8-year-old male child presented to the emergency
department with clinical features of peritonitis, raising suspicion of
appendicular or small bowel perforation. Intervention/Outcome:
Diagnosis of chylous ascites with primary intestinal lymphangiectasia
made on laparotomy. Message: Acute peritonitis may be a
presentation of primary intestinal lymphangiectasia and chylous ascites.
Keywords: Acute abdomen, Intestinal lymphangiectasia,
Peritonitis.
|
|
A
lthough lymphangiectasia is common in the neck
and axilla, it rarely involves intra-abdominal organs [1]. Intestinal
lymphangiectasia is characterized by dilatation of intestinal lymphatics
[2,3]. The clinical presentations of intestinal lymphangiectasia include
pitting edema, chylous ascites, pleural effusion, diarrhea,
malabsorption and intestinal obstruction. Acute peritonitis is a rare
presentation, and it may mimic other surgical pathologies [4,5].
Case Report
An 8-year-old male child presented to the emergency
department with periumbilical pain, vomiting and fever. There was no
history of tuberculosis or typhoid fever, and no history of trauma or
surgery. On examination, he was febrile with temperature of 39°C. The
abdomen was distended with diffuse tenderness and guarding. The total
leucocyte count was 22,500/mm 3.
Serum amylase was 23 units/L. Ultrasonography revealed a multiloculated
intra-abdominal collection. The presence of severe pain and fever
accompanied with clinical features of peritonitis, and sonological
evidence of abdominal collection raised the suspicion of appendicular or
small bowel perforation with sepsis. X-Ray of the chest and
abdomen were unremarkable, there was no evidence of free
intra-peritoneal air. In the absence of availability of emergency
computed tomography scan, the patient was taken up for emergency
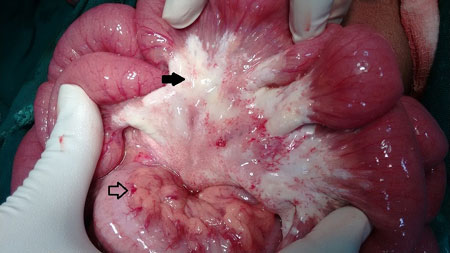
laparotomy for the acute abdomen. Laparotomy revealed 150 ml of milky
white ascitic fluid and chalky white plaques in the mesentery. A few
mesenteric lymph nodes were seen (Fig. 1). The small bowel
and the appendix appeared grossly normal. A clinical diagnosis of
chylous ascites with dilated mesenteric lymphatics (lymphangiectasia)
was made. The chylous fluid was drained and a thorough peritoneal lavage
was done. Biopsies were taken from the mesenteric lymph nodes and
peritoneum.
 |
|
Fig. 1 Chalky white plaques in
mesentery due to dilated lymphatics (bold arrow). Normal fatty
yellow mesentery (lined arrow).
|
Histopathological report was negative for
tuberculosis and malignancy. The ascitic fluid was rich in triglycerides
(254 mg/dL) and demonstrated chylomicrons and lymphocytes on biochemical
analysis. Culture and gram stain were negative. Serum LDL, HDL and
triglyceride values were normal. The postoperative period was
uneventful. The abdominal drain was removed on post-operative day 2 with
no significant output. He was discharged on a high protein and low fat
diet, and was asymptomatic at 1-year post-surgery follow up.
Discussion
Intestinal lymphangiectasia is classified as primary
or secondary, based on the underlying etiology. Primary intestinal
lymphangiectasia represents a congenital disorder of mesenteric
lymphatics, whereas secondary is associated with diseases like
constrictive pericarditis, lymphoma, pancreatitis, trauma, intestinal
malignancy, or may be acquired after surgery [6]. Intestinal
lymphangiectasia is often associated with chylous ascites which may
easily be mistaken as purulent fluid. The most common cause of chylous
ascites in the pediatric population is congenital lymphatic
malformation, others being malignancy, tuberculosis, trauma, cirrhosis
and post-surgery [7]. The principal mechanisms for formation of chylous
ascites are related to disruption of the lymphatic system, from any
cause.
Dietary long-chain triglycerides are converted into
monoglycerides and free fatty acids and absorbed as chylomicrons in the
small bowel lymphatic system, which is responsible for high triglyceride
content and the milky appearance of lymph. Medium chain triglycerides,
constituting approximately one-third of dietary fat, on the other hand,
are absorbed directly by the portal venous system, which is the
rationale for their use in the conservative management of chylous
ascites [7].
Loss of chyle into peritoneal cavity can lead to
serious consequences because of the loss of essential proteins, lipids,
immunoglobulins, vitamins, electrolytes, and water. In most cases,
patients respond to low fat and high protein diet, enriched with
medium-chain fatty acids and no surgery is required. It is very
important to replenish fluid and electrolyte losses and treat vitamin
deficiencies [4]. Emergency exploratory laparotomy is mostly done only
in cases with acute chylous peritonitis for a preoperative suspicion of
bowel perforation; however, it gives the opportunity to evacuate the
peritoneal fluid, wash the abdominal cavity, and in certain cases, treat
the cause.
In case of chronic or debilitating ascites associated
with poor weight gain, hypoproteinemia and abdominal distension,
elective surgical treatment to treat the lymphatic fistula is
indispensible. Preoperative lymphangiography or lymphoscintigraphy is
helpful in identifying the anatomical location of the leakage or the
presence of a fistula in such presentations [8]. In our case, the
diagnosis of primary intestinal lymphangiectasia was established by the
presence of chylous ascites (rich in triglycerides and chylomicrons),
and the classical appearance of white chalky mesentery in the absence of
any secondary cause.
Contributors: All authors have designed,
contributed and approved the manuscript.
Funding: None, Competing interest: None
stated.
References
1. Pandey D, Garg PK, Jana M, Sharma J.
Retroperitoneal lymphangiectasia. ANZ J Surg. 2016;86:517-8.
2. Isa HM, Al-Arayedh GG, Mohamed AM. Intestinal
lymphangiectasia in children. Saudi Med J. 2016;37:199-204.
3. Rashmi MV, Murthy BN, Rani H, Kodandaswamy CR,
Arava S. Intestinal lymphangiectasia - a report of two cases. Indian J
Surg. 2010;72:149-51.
4. Fang F, Hsu S, Chen C, Chen T. Spontaneous chylous
peritonitis mimicking acute appendicitis/ : A case report and review of
literature. World J Gastroenterol. 2006;12:154-6.
5. Vettoretto N, Odeh M, Romessis M, Pettinato G,
Taglietti L, Giovanetti M. Acute abdomen from chylous peritonitis: Case
report and literature review. Eur Surg Res. 2008;41:54-7.
6. Suresh N, Ganesh R, Sankar J, Sathiyasekaran M.
Primary intestinal lymphangiectasia. Indian Pediatr. 2009;46:903-6.
7. Al-busafi SA, Ghali P, Deschênes M, Wong P.
Chylous ascites: Evaluation and management. ISRN Hepatol.
2014;2014:240473.
8. Campisi C, Bellini C, Eretta C, Zilli A, Rin E da,
Davini D, et al. Diagnosis and management of primary chylous
ascites. J Vasc Surg. 2006;43:1244-8.
|
|
|
 |
|

