|
|
|
Indian Pediatr 2018;55: 9 07-908 |
 |
Laser Treatment of a
Tracheal Inflammatory Myofibroblastic Tumor
|
|
D Vijayasekaran 1,
S Thirunavukkarasu2
and S Ramesh3
From Departments of 1Pulmonology, 2ENT and
Airway Surgery, and 3Anesthesiology; Kanchi Kamakoti CHILDS
Trust Hospital, Chennai, India.
Correspondence to: Dr D Vijayasekaran, No. 4, Third Street, Dr
Subbarayan Nagar, Kodambakkam, Chennai 600 024.
Email: [email protected]
Received: June 05, 2017;
Initial review: July 05, 2017;
Accepted: July 23, 2018.
|
Background: Inflammatory myofibroblastic tumors
of the trachea are rare childhood quasi-neoplastic lesions. Case
characteristics: 7-year-old boy with recurrent episodes of cough,
breathing difficulty and wheeze, initially treated as asthma.
Intervention: CT chest and flexible bronchoscopy revealed a mass
lesion of the trachea, which was excised by diode laser through the
ventilating bronchoscope. Histopathology confirmed it as the
inflammatory myofibroblastic tumor. Message: Use of laser ensured
complete endotracheal excision of the tumor.
Keywords: Bronchoscopy, Diode Laser, Inflammatory pseudotumor.
|
|
I
nflammatory myofibroblastic tumors (IMT) are
quasi-neoplastic rare childhood tumors with a benign clinical course.
Since IMT can occur at any anatomical site (both pulmonary and
extrapulmonary) with diffuse inflammatory infiltrate in histopathology,
IMTs have been named with varying terminologies like plasma cell
granuloma, fibrous histiocytoma, xanthogranuloma and inflammatory
pseudotumor [1,2]. Pulmonary IMT is predominantly located within the
lung parenchyma rather than presenting as endobronchial lesion [3]. We
report a child with IMT of the trachea and its endotracheal excision.
Case Report
A 7-year-old male child presented with recurrent
episodes of cough and breathing difficulty, and occasional wheeze. The
child had been treated as asthma for more than a year, without clinical
improvement, and was subsequently, the child was referred to us.
The detailed clinical evaluation revealed that his
symptoms were progressive in the last 6 months, with no history of
hemoptysis, and no family history of asthma or atopy. His vital signs
and laboratory investigations were within normal limits. Chest
radiography showed bilateral hyperinflation. Multidetector computed
tomography (MDCT) showed a mass lesion with calcification, at the
anterolateral aspect of the trachea.
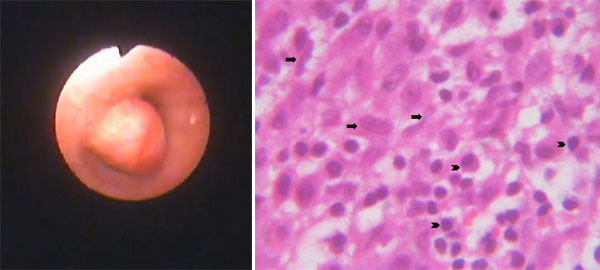
Flexible bronchoscopic examination showed a mass
lesion attached to the anterior wall of lower trachea (Fig. 1).
The lesion was a smooth-surfaced, sessile about 0.7 cm x 0.5 cm in size
causing near total obstruction of trachea. Biopsy was done by rigid
bronchoscopy which was suggestive of inflammatory fibromyoma of the
trachea.
 |
|
Fig. 1 Bronchoscopy view and HPE of
inflammatory myofibroblastic tumor and photomicrograph showing a
lesion composed of elongated spindle cells (arrow) admixed with
inflammatory cell population (arrow head) in the background (H&E
x 400).
|
Under total intravenous anesthesia using ventilating
bronchoscope, diode laser excision of the mass was done.
Histopathological examination of the specimen showed squamous lining
epithelium and spindle cells admixed with inflammatory cell population.
Immunohistochemical findings were positive for Vimentin, anaplastic
lymphoma kinase (ALK) and Desmin which were consistent with inflammatory
myofibroblastic tumor (Fig. 1).
Discussion
Tracheal tumors are easily treatable when diagnosed
in the early stages. Due to the low incidence and the variability of
clinical presentation, the diagnosis and treatment of tracheal IMT are
often delayed. If a child does not respond to asthma management,
alternatives like endobronchial mass lesions need to be considered.
Although IMT have been described in virtually every
anatomic location, there are only few documented reports with tracheal
localization [4]. The index case presented with slowly progressive
symptoms mimicking asthma but other studies have reported acute
presentation with severe respiratory distress mimicking as foreign body
[5].
Based on the location in the pulmonary system, IMTs
are divided into two groups as parenchymal and airway IMTs. Most IMTs
manifest as a solitary lesions in the lung parenchyma, and only 10% of
these develop within the airway. The analysis of bronchoscopically
treated IMT of the tracheobronchial tree in the age group of 16-45 years
revealed that roughly half of them (43%) were confined to the trachea
[6].
The index case started his symptoms from 6 years of
age. Though IMT are reported in adults, these are the most common
benign lung tumor in children under 16 years of age [7]. Though initial
CT reported as papilloma, which is a common tracheal tumor, excision
biopsy confirmed as IMF. Endobronchial excision was made possible by
rigid bronchoscopy diode laser. Transportability, cost, penetration
depth (0.3-1.0 mm) and effective photocoagulation of the diode laser are
the advantageous features. In endobronchial surgery, the advantages of
various lasers have repeatedly been debated but in our experience diode
laser appears to be more precise and less invasive [8]. The
immuno-histochemistry of the specimen was typically reactive to vimentin
(99% specific), desmin (69% specific) with ALK-1 expression (highly
specific), which were all consistent with IMT (Fig. 1)
[9].
As IMF is considered to have low-grade malignant
potential, bronchoscopic excision of the tumor with the diode laser
appears to have advantages in resource-poor settings [10]. The
appropriate surgical intervention will ensure a normal life if such
children are referred early.
Contributions: DVS: conception and design
of the study; TNS: surgical management and final version; SR:
anaesthetic management.
Funding: None; Competing Interest:
None stated.
References
1. Özgül MA, Toru Ü, Acat M, Özgül G, Çetinkaya E,
Dinçer HE, et al. A rare tumor of trachea: Inflammatory
myofibroblastic tumor diagnosis and endoscopic treatment. Respir Med
Case Rep. 2014;13:57-60.
2. Aihole JS. LokanathH, Munianjinappa NB. Primary
pleural inflammatory pseudotumor in a Child. Indian Pediatr.
2018;55:341-2.
3. Liu L, Kong X, Lu X, Cao D. Pediatric
endobronchial inflammatory myofibroblastic tumor: A case report and
review of the literature. Clin Pract. 2016;6:853.
4. Venizelos I, Papathomas T, Anagnostou E, Tsanakas
J, Kirvassilis F, Kontzoglou G. Pediatric Inflammatory myofibroblastic
tumor of the trachea: A case report and review of the literature.
Pediatr Pulmonol. 2008;43:831-5.
5. Ray A, Suri JC, Bhattacharya D, Gupta A.
Bronchoscopy resection of endobronchial inflammatory myofibroblastic
tumor: A case report and systematic review of the literature. Lung
India. 2014;31:172-5.
6. Sivanandan S, Lodha R, Agarwala S, Sharma, Kabra
SK. Inflammatory myofibroblastic tumor of the trachea. Pediatr Pulmonol.
2007; 42:847-50.
7. Oztuna F1, Pehlivanlar M, Abul Y, Tekinbas C,
Ozoran Y, Ozlu T. Adult inflammatory myofibroblastic tumor of the
trachea: Case report and literature review. Respir Care. 2013;58:e72-6.
8. Arroyo HH, Neri L, Fussuma CY, Imamura R. Diode
Laser for Laryngeal Surgery: A Systematic Review. Int Arch Otolaryngol.
2016;20:172-9.
9. Palaskar S, Koshti S, Maralingannavar M, Bartake
A. Inflammatory myofibroblastic tumor. Contemp Clin Dent. 2011;2:274-77.
10. Fabre D1, Fadel E, Singhal S, de Montpreville V,
Mussot S, Mercier O, et al. Complete resection of pulmonary
inflammatory pseudotumors has excellent long-term prognosis. J Thorac
Cardiovasc Surg. 2009;137:435-40.
|
|
|
 |
|

