|
|
|
Indian Pediatr 2018;55:885-892 |
 |
Management of Childhood
Functional Constipation: Consensus Practice Guidelines of Indian
Society of Pediatric Gastroenterology, Hepatology and Nutrition
and Pediatric Gastroenterology Chapter of Indian Academy of
Pediatrics
|
|
Surender Kumar Yachha
1,
Anshu Srivastava1,
Neelam Mohan2,
Lalit Bharadia3
and Moinak Sen Sarma1;
for
the Indian Society of Pediatric Gastroenterology,
Hepatology and Nutrition Committee on Childhood Functional Constipation,
and Pediatric Gastroenterology Subspecialty Chapter of Indian Academy of
Pediatrics
From 1Department
of Pediatric Gastroenterology, SGPGIMS, Lucknow; 2Department
of Pediatric Gastroenterology, Hepatology and Liver Transplantation,
Medanta Hospital, Gurgaon; and 3Fortis Escorts
Hospital, Jaipur; India.
List of other collaborators in Appendix 1.
Correspondence to: Dr Surender Kumar Yachha,
Professor and Head, Department of Pediatric Gastroenterology, Sanjay
Gandhi Postgraduate Institute of Medical Sciences, Lucknow 226 014,
India.
Email: [email protected]
Published online: June 13, 2018.
PII:S097475591600121
|
|
Justification: Management
practices of functional constipation are far from satisfactory in
developing countries like India; available guidelines do not
comprehensively address the problems pertinent to our country.
Process: A questionnaire-based
survey was conducted among selected practising pediatricians and
pediatric gastroenterologists in India, and the respondents agreed on
the need for an Indian guideline on the topic. A group of experts were
invited to present the published literature under 12 different headings,
and a consensus was developed to formulate the practice guidelines,
keeping in view the needs in Indian children.
Objective: To formulate practice
guidelines for the management of childhood functional constipation that
are relevant to Indian children.
Recommendations: Functional
constipation should be diagnosed only in the absence of red flags on
history and examination. Those with impaction and/or retentive
incontinence should be disimpacted with polyethylene glycol (hospital or
home-based). Osmotic laxatives (polyethylene glycol more than 1 year of
age and lactulose/lactitol less than 1 year of age) are the first line
of maintenance therapy. Stimulant laxatives should be reserved only for
rescue therapy. Combination therapies of two osmotics, two stimulants or
two classes of laxatives are not recommended. Laxatives as maintenance
therapy should be given for a prolonged period and should be tapered off
gradually, only after a successful outcome. Essential components of
therapy for a successful outcome include counselling, dietary changes,
toilet-training and regular follow-up.
Keywords: Lactulose, Laxatives, Polyethylene
glycol, Rescue therapy.
|
|
F
unctional constipation is a common problem in
children. Although some guidelines exist for management of childhood
constipation, there are no such guidelines for Indian children. In order
to understand the existing practices and magnitude of the problem, a
questionnaire was prepared with 22 questions and circulated to
practicing pediatricians and pediatric gastroenterologists in India from
October to December, 2014 using Monkey Survey tool. All the respondents
felt the need for an Indian guideline. To accomplish this goal, a group
of pediatric gastroenterologists and surgeons searched the published
literature under 12 headings. A two-day deliberation was held on 19-20
September, 2015 at Jaipur, attended by selected pediatricians, pediatric
gastroenterologists and pediatric surgeons (Annexure 1).
Each expert presented the existing literature, which was discussed
inclusive of experiences and a consensus opinion was reached on
different issues.
Functional constipation constituted 30% of pediatric
gastroenterology office practice, 4-5% of all referrals to pediatric
gastroenterology tertiary care centers and 0.8-1% of all pediatric cases
in medical colleges. At the end of the meeting, it was decided to
include these recommendations as a guideline on the evaluation and
management of functional constipation in children in India. A writing
group was designated for the same. The draft was sent by email to all
experts and their suggestions were incorporated in the final guidelines.
Definitions
Normal stool frequency: There are very few
studies on normal stool frequency and consistency in Indian children.
The average stool frequency of Indian children is as follows: <1 month
age: 3-4 times/day; 1 month to 1 year age: 1.5-2 times/day; 1 to 2 year
age: 1-2 times/day, mostly formed; older than 2 year age: 1 time/day
[1,2].
Constipation: A delay or difficulty in defecation
sufficient to cause significant distress to the patient is defined as
constipation. When the duration of constipation is less than 4 week, it
is labeled as acute constipation and when the duration is more, it is
labeled as chronic constipation.
Based on the North American Society of Pediatric
Gastroenterology, Hepatology and Nutrition (NASPGHAN) guidelines, Rome
III criteria [3,4] and expert opinion, the definition recommended for
application in Indian children is given in Box 1.
|
Box 1 Definition of Constipation for Use
in Indian Children
• Duration of more than 4 weeks for all ages;
and
• Presence of
³2
of the following: (a) defecation frequency
£2
times per week, (b) fecal incontinence
³1
times per week after the acquisition of toileting skills, (c)
history of excessive stool retention, (d) history of
painful or hard bowel movements, (e) presence of a large
mass in the rectum or on per abdomen examination, (f)
history of large-diameter stools that may obstruct the toilet
(This may not be elicitable for majority of Indian children who
do not use the Western type of toilet).
|
Based on normal stool frequency of >1/day in Indian
children of older than 2 year, physicians should be guided more by the
stool consistency and other features of functional constipation rather
than stool frequency. Stool frequency of
£2/week as defined in
Western guidelines may not be necessarily applicable in Indian children
and may miss a substantial number of children with constipation if this
criterion is taken in isolation. Collateral manifestations in the form
of irritability, decreased appetite and/or early satiety may be
observed, which improve after defecation.
The terms soiling/encopresis should not be used.
Instead, the term ‘fecal incontinence’ should be used. This is defined
as passage of stools in the undergarment. Fecal incontinence is
classified as: (a) Constipation-associated fecal incontinence and
(b) non-retentive fecal incontinence: diagnosed only if there is
no constipation and normal anal sphincter tone, and symptoms last for
more than 2 months in a child with a developmental age of
³4 years.
Refractory constipation: Constipation not
responding to optimal conventional treatment for at least 3 months,
despite good compliance [5]. These patients should be referred to a
pediatric gastroenterologist for evaluation.
History and Examination
History and examination are relevant in making a
diagnosis of constipation, differentiating functional and organic
constipation, looking for precipitants of functional constipation and
eliciting issues relevant to management like incontinence, impaction,
past treatment, treatment compliance and response to treatment. Clinical
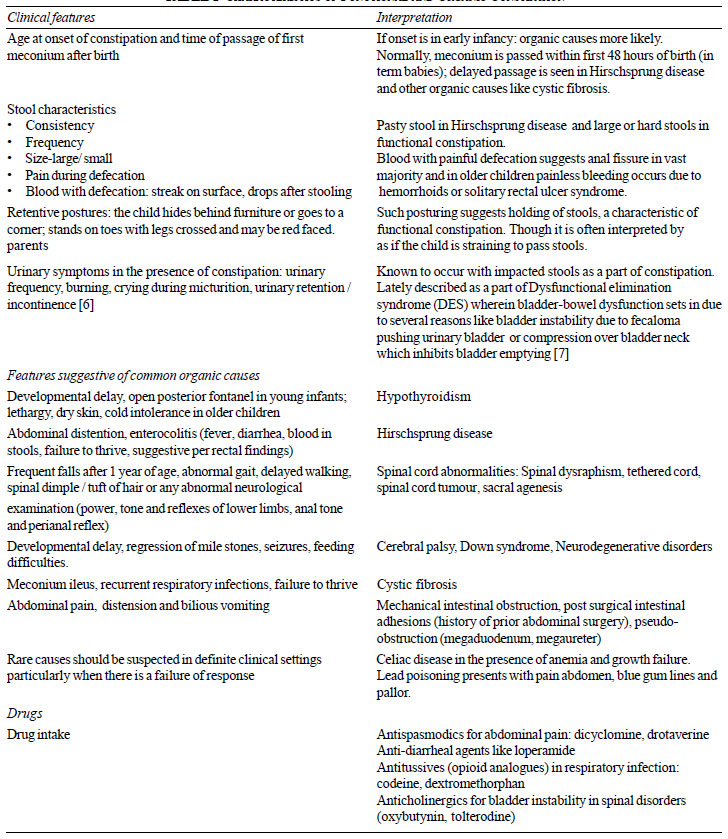
features and their interpretation are shown in Table I.
|
TABLE I Characteristics of Functional
and Organic Constipation
|
 |
Dietary history: Details of diet should be taken:
intake of fruits and vegetables and refined foods (e.g., bakery
products), beverages etc. in older children, nature of feeds (breast
vs top feeds) and details of supplementary feeds in younger babies.
Exclusive and prolonged milk intake with minimal solids in young infants
is a major factor causing functional constipation in India (unanimous
opinion). These children are at an increased risk of iron deficiency
anemia.
Important precipitating factors of functional
constipation: The following are the most common factors which
initiate constipation in children
[8]: (a) premature initiation of toilet training
(normally toilet training should start not before 24 months in a
developmentally normal child) (b) drugs (Table I)
and inter-current illnesses, (c) quick and abrupt transition of
diet e.g. liquid to solid, breastfeeding to bottle feeding and (d)
change in local environment (start of schooling) and psychosocial
factors.
Evaluation
Patients should be examined thoroughly with proper
growth assessment to rule out an organic etiology (Table I).
Lower abdomen should be palpated for fecoliths (soft or hard indentable
masses). In the absence of abdominal fecoliths, anal fissure or anal
malformations, digital rectal examination (index finger in an older
child or little finger in an infant) helps in the following: (a)
presence of fecal impaction (seen in 50-70% children with functional
constipation and is diagnosed in the presence of a hard mass (fecal
mass) in the lower abdomen or presence of large, hard stools (fecolith)
on Digital rectal examination (DRE), (b) diagnosis of
Hirschprung’s disease (empty rectum, gush of stools/air on withdrawal of
finger), and (c) sacral mass lesion (palpable mass). DRE is not
essential in all cases or at all visits. It is recommended in the
following instances: (a) red flag symptoms or signs, (b)
onset <6 months of age, (c) non-responders despite good
compliance to therapy, and (d) patients presenting with fecal
incontinence to differentiate between constipation related and
non-retentive incontinence [9-11].
Red flags suggestive of organic constipation:
delayed passage of meconium, onset in early infancy, ribbon or
pellet stools, bilious vomiting, uniform abdominal distension, failure
to thrive, recurrent lower respiratory infections, cold intolerance,
neuro-developmental delay or regression, gush of stools on DRE, anal
malformations, abnormal neurological examination (paraspinal, lower
limbs and anorectal reflexes). Details are given in Table I.
Investigations: 95% children with
constipation have functional constipation and do not need any
investigations. Children with red flags (as above) suggestive of organic
etiology or those who are diagnosed as functional constipation but fail
to respond to therapy need diagnostic evaluation. A plain erect Xray
abdomen or barium enema is not required as a routine investigation in
all cases. [12-14].
Management of Functional Constipation
The following points should be addressed: patient
counseling, toilet training, modifications in diet, drug management, and
follow-up.
Patient Counseling
Salient pathophysiological aspects inclusive of
objective of treatment should be explained to the parents. Parents
should be clearly explained the cause of functional constipation,
preferably with a diagram. Any precipitating factors identified should
be eliminated or modified by appropriate advice (e.g. in a child
with exclusive milk feeding, (semi) solid diet supplementation should be
instituted; drugs causing constipation should be stopped; any
psychosocial factor operating needs to be addressed).
Toilet-training
Toilet training should not be started before 24
months of age; however, there is a variation in recommended age of
training between 3-4 years. Follow the ‘Rule of 1’: Toilet
training to be done by one person, one routine (5 min after each major
meal), one place, one word e.g. pooh/potty etc. In a child with
constipation: (a) make the child sit in the toilet, 2-3 times a
day for 5-10 minutes after meals (within 30 minutes of meal intake), (b)
make the defecation painless by treating anal fissures, if present, (c)
sit in squatting position in the Indian toilet or with foot rest in
English toilet/potty seat to have appropriate angulation of knees and
thighs to facilitate expulsion of stools, (d) reward system
(positive reinforcement) helps in motivating the child and avoiding
child-parent conflict.
Diet, Fiber and Water Intake
There are no well-conducted randomized controlled
studies of diet and treatment of constipation. Daily fiber requirement
is 0.5 gm/kg/day. Adequate intake of fiber-rich diet (cereals, whole
pulses with bran, vegetables, salad and fruits) is recommended at the
initial counseling. High fiber diet chart should be given to parents (as
per local practice). Restrict milk and encourage intake of semi-solids
and solids in younger children. Ensure adequate intake of water. Normal
activity is recommended.
Medical Therapy
It consists of initial phase of disimpaction in
patients with fecal impaction and a maintenance phase with laxatives.
Disimpaction
Rationale of disimpaction: Completely clear the
colon so that no residual hard fecal matter is retained. Thereafter the
maintenance laxative therapy can keep the bowel moving and empty so that
there is no retention. This enables rectum to achieve the normal
diameter and tone for proper anorectal reflexes and pelvic floor
coordination to facilitate normal stool expulsion
Options for Disimpaction: There are two ways of
disimpaction (Table II) (a) one-time hospital based
(100% success) (b) home based in split doses (68-97% success)
[14,15,17]. Rarely rectal enemas can be used as supplementary therapy to
clear the heavily hard loaded colorectal region. Oral route is preferred
as it non-invasive, has better patient acceptability, cleans the entire
colon and is equally effective as rectal disimpaction. Manual evacuation
of rectum is rarely required in patients failing oral and rectal
disimpaction but it should be performed under anaesthesia. Children
undergoing disimpaction should be reviewed within one week of
disimpaction to assess for re-impaction. Maintenance therapy should be
started only after effective disimpaction.
|
Agent |
Dosage |
Side effect |
Comments |
|
Oral agents |
|
Polyethylene glycol*(at home) |
1.5-2 g/ kg/ d in two divided |
Loose stools, bloating/ |
– |
|
doses for 3-6 d** only |
flatulence, nausea, vomiting |
|
|
depending upon the clarity of |
|
|
|
rectal effluent |
|
|
|
Polyethylene glycol solution |
25 mL/ kg/ h oral or by |
Nausea, vomiting, abdominal |
Caution: during one-time |
|
for lavage (in hospital) |
nasogastric tube in young |
cramps, rarely electrolyte |
disimpaction, watch for |
|
children |
abnormality, pulmonary |
bloating, abdominal |
|
End point is clear rectal |
aspiration |
distension or fluid overload |
|
effluent |
|
|
|
Young children may require |
|
|
|
intravenous fluids to maintain |
|
|
|
hydration |
|
|
|
Rectal agents |
|
Enemas (once per day) [15] |
|
|
|
Saline
|
Neonate <1 kg: 5 mL; >1 kg: 10 mL
>1y: 6 mL/kg, once or twice/day |
|
Not usually practised except
in special situations |
|
Phosphate soda |
2-18 y: 2.5 mL/kg, max 133 |
Hyperphosphatemia |
|
|
(Proctoclysis enema 100 mL) |
mL/dose |
Hypocalcemia |
|
|
PEG is a metabolically inert, large molecular weight soluble
polymer with capacity to retain intraluminal water. PEG is
available with or without electrolytes and as PEG 3350 or
4000.With the available evidence, PEG 3350 or 4000 and PEG with
or without electrolytes are all equally effective in
disimpaction [16]; *For one-time disimpaction there are Indian
formulations where one pack (containing polyethylene glycol of
118gm) should be reconstituted in 2 litres of water; ** For
maintenance or home-based disimpaction the preparation may vary
from 6.5g/scoop to 17g /sachet, and needs to be confirmed before
prescription. |
Maintenance therapy
There are different classes of laxatives used for
constipation (osmotic and stimulants).
Osmotic laxatives: These are the mainstay
of maintenance therapy in children [5]. These laxatives
draw water into the stool thereby making the stools softer and easy to
pass. The two main osmotic laxatives are polyethylene glycol (PEG) and
lactulose/lactitol (Table III). Based on the literature,
and the experience of the group, the recommendations are: (i) PEG
is the first line of therapy and is more effective as compared to
lactulose/lactitol. However in children <1 year of age, the only drug
recommended is lactulose/lactitol. (ii) In case of non-response
or intolerance due to non-palatability to PEG, the second line of
treatment is lactulose/lactitol which is safe for all ages. (iii)
Two osmotic agents like PEG and lactulose/lactitol should not be given
simultaneously. Combinations therapy with two classes of laxatives is
not recommended for children [5].
TABLE III Osmotic Laxatives for Maintenance Therapy
|
Osmotic laxative |
Dose |
Side effects |
Comment |
|
Polyethylene Glycol [16] |
0.5-1g/kg /day >12 mo age |
Bloating, |
Safe for both short and long |
|
|
Abdominal pain/cramps |
term use |
|
|
Vomiting |
|
|
|
Loose stools |
|
|
Disaccharides [19] |
|
|
|
|
Lactulose: non absorbable |
1mo-12mo: 2.5 mL BD; |
Abdominal distension |
Lactulose undergoes |
|
synthetic disaccharide, |
1-5y: 2.5-10 mL BD; |
Discomfort |
fermentation in the colon to |
|
consists of 2 molecules of |
5-18y: 5-20 mL BD |
|
yield short chain fatty acids, |
|
galactose and fructose |
|
|
CO2 and H2 |
|
Lactitol (b-galactosido- |
250 to 400 mg/kg/d |
|
|
|
sorbitol): monohydrate is a |
(15 mL =10 g of lactitol |
|
Lactitol is more palatable with |
|
analogue of lactulose, |
monohydrate |
|
better acceptability |
|
consists of galactose and |
|
|
|
|
sorbitol |
|
|
|
Stimulant Laxatives: Stimulant laxatives
are used only as rescue therapy No randomized controlled trials
are available in children regarding their efficacy. Stimulants are
usually required as rescue therapy (an acute or sudden episode of
constipation while being on regular compliant maintenance therapy).
These stimulants are given for a short duration of 2-3 days to tide over
the acute episode of constipation, and then stopped (Table IV)
[18].
TABLE IV Stimulant Laxatives: Rescue therapy
|
Name |
dose |
Side effects |
Comments |
|
Acts by stimulating colonic |
Oral (effect in 6-8 h), |
Short term usage is free from |
Contraindicated in children |
|
motility, promoting secretion |
single bedtime dose |
side effects. Abdominal cramps, |
with proctitis or anal fissures. |
|
and inhibition of absorption |
3-10 y: 5 mg/d |
diarrhea, hypokalemia, proctitis |
|
|
of water and electrolytes |
>10 y: 5-10 mg/d |
(rare), on prolonged use. |
|
|
in colon |
Should not be used in children |
|
|
|
below 3 years of age |
|
|
|
Rectal (effect within 30-60 min) |
|
|
|
2-10 y: 5 mg/d |
|
|
|
>10 y: 5-10 mg/d |
|
|
|
Sodium Picosulphate |
|
|
|
|
Acts through its active meta- |
Given as single dose |
Abdominal pain, nausea, and |
Contraindicated in setting of |
|
bolite that is produced by the |
1 mo-4 y |
diarrhea ~ 50% |
proctitis and gaseous abdo- |
|
intestinal bacteria and increases |
2.5-10 mg/d |
|
minal distension (underlying |
|
the peristalsis of gut |
4 to 18 y |
|
intestinal obstruction or |
|
2.5-20 mg/d Available as liquid |
|
paralytic ileus) |
|
In view of the side effects of these agents, it is advocated
for short duration as rescue therapy. |
Behavioral therapy and biofeedback; These
are helpful when constipation is associated with behavioral
co-morbidity or pelvic floor dysfunction in older children and
adolescents. This requires referral to centers with expertise.
Follow-up: Regular follow-up is essential.
At each follow-up, record the stool history, associated symptoms,
compliance with diet, medications and toilet-training. It is important
to have a stool diary for proper follow-up. Parents should maintain a
stool diary for objective assessment of response to therapy related to
stool frequency and consistency. First follow-up is advised at 14 days
to assess compliance. Subsequently, 1-2 monthly follow-up till normal
bowel habit is attained or physician is satisfied with response as
defined below as ‘successful outcome’. Further, 3-monthly follow-up for
a minimum period of one year. While on follow-up, the maintenance dose
may be increased or decreased to achieve daily passage of stools,
keeping in view the features of successful outcome.
Successful outcome of treatment should
be defined as (a) stool normalcy while on laxatives for a period
of at least 4 weeks of initiation of therapy, and (b) achievement
of stool normalcy for a minimum period of 6 months before tapering.
Normalcy of stools should defined as daily, not-hard, nor loose watery
stools, with absence of pain, straining, bleeding, posturing or
incontinence.
In Western countries, 50% of children with functional
constipation recover and are taken off medication within 6-12 months
[19, 20]. About 25% continue to experience symptoms up to adult age
[21]. Data from India show that 95% respond over a mean (SD) follow-up
of 15.0 (16.7) months [14]. 18.4% patients have recurrence of symptoms
on follow up; 10.5% of them require rescue disimpaction after a median
duration of 5.5 (1.5-17) months of the first disimpaction [14].
When to stop laxatives: No clear
guidelines exist and only expert opinions are available. Based on
the natural history, child should have been symptom-free while on
maintenance therapy for at least 6 months before attempting to taper the
laxatives. It is then advisable to taper gradually over a period of 3
months. Laxatives should never be stopped abruptly. In the developmental
stage of toilet training, medication should only be stopped once toilet
training and establishment of a regular stooling pattern is achieved.
Dietary and toilet training advice should continue even after stoppage
of laxatives. Triggers and precipitating factors of functional
constipation should have been adequately addressed. Parents should have
the knowledge about the management and also risk of relapse of symptoms
on stoppage of medication.
Refractory constipation: Those patients
not responding to a sustained optimal medical management of functional
constipation should be investigated for hypothyroidism, celiac disease,
Hirschprung disease, Cow milk protein allergy in young children, lead
poisoning and spinal abnormalities. These children also need evaluation
for presence of slow colonic transit, pelvic dyssynergia and
pseudo-obstruction, in centers with expertise.
Conclusion
Functional constipation should be diagnosed in the
absence of red flags. Impacted (incontinent) and non-impacted subgroups
should be identified. Management protocol should be adapted as per the
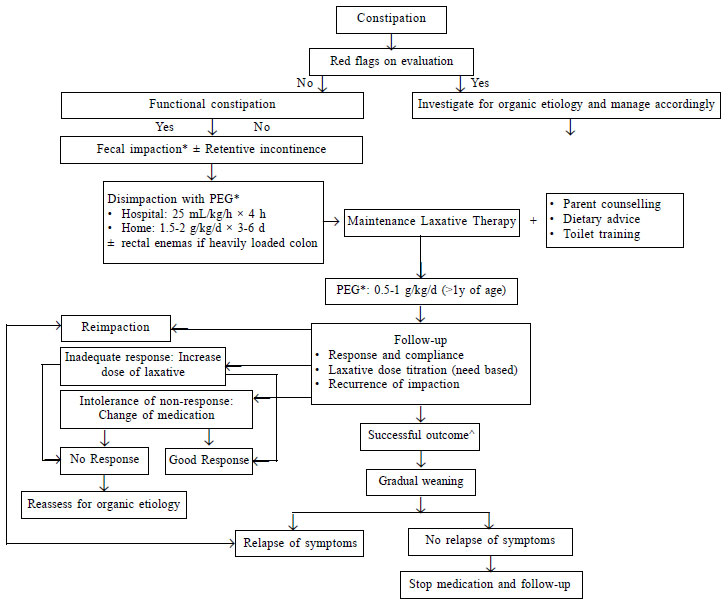
algorithm shown in Fig. 1. Emphasis should be laid on
toilet-training and importantly in counselling particularly related to
long-term usage of medical therapy.
 |
|
*Fecal impaction (seen in 50-70% children
with functional constipation) is diagnosed in the presence of a
hard mass (fecal mass) in the lower abdomen or presence of
large, hard stools on DRE (fecolith); and ^Successful outcome
defined as (a) stool normalcy while on laxatives for a
period of at least after 4 weeks; initiation of therapy, and (b)
achievement of stool normalcy for a minimum period of 6 months
before tapering; PEG: polyethylene glycol (refer table 2);
stimulant laxatives are not a part of the routine management of
algorithm and should only be reserved for rescue therapy.
Fig. 1 Algorithm for the management
of childhood functional constipation.
|
Annexure 1: Participants of
the Indian Society of Pediatric Gastroenterology, Hepatology and
Nutrition Committee on Childhood Functional Constipation, and Pediatric
Gastroenterology Subspecialty Chapter of Indian Academy of Pediatrics
Experts (in alphabetical order):
Lalit Bharadia, Jaipur (co-convenor); Vidyut
Bhatia, New Delhi; Vishnu Biradar, Pune; Vibhor Borkar, Mumbai; Barath
Jagadisan, Puducherry; Sakshi Karkra, Gurgaon; Praveen Kumar, New Delhi;
Neelam Mohan, Gurugram; Srinivas Sankarnarayanan, Chennai; Malathi
Sathiyasekaran, Chennai; Pramod Sharma, Jaipur; Anshu Srivastava,
Lucknow; Babu Ram Thapa, Chandigarh; Surender Kumar Yachha, Lucknow
(Convener).
Critical appraisal (in alphabetical order):
Raj Kumar Gupta, Jaipur; Natwar Parwal, Jaipur; Ashok Kumar Patwari,
New Delhi; VS Sankarnarayanan, Chennai
Writing committee:
Surender Kumar Yachha, Anshu Srivastava,
Moinak Sen Sarma
References
1. Yadav M, Singh PK, Mittal SK. Variation in bowel
habits of healthy Indian children aged up to two years. Indian J Pediatr. 2014;81:446-9.
2. Sujatha B, Velayutham DR, Deivamani N, Bavanandam
S. Normal bowel pattern in children and dietary and other precipitating
factors in functional constipation. J Clin Diag Res. 2015;9:SC12-5.
3. Hyman PE, Milla PJ, Benninga MA, Davidson GP,
Fleisher DF, Taminiau J. Childhood functional gastrointestinal
disorders: neonate/toddler. Gastro-enterology. 2006;130:1519-26.
4. Rasquin A, Di Lorenzo C, Forbes D, Guiraldes E,
Hyams JS, Staiano A, et al. Childhood functional gastrointestinal
disorders: child/adolescent. Gastroenterology. 2006;130: 1527-37.
5. Tabbers MM, DiLorenzo C, Berger MY, Faure C,
Langen-dam MW, Nurko S, et al. Evaluation and Treatment of
Functional Constipation in Infants and Children: Evidence-Based
Recommendations From ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr.
2014;58:258-74.
6. Loening-Baucke V. Urinary incontinence and urinary
tract infection and their resolution with treatment of chronic
constipation of childhood. Pediatrics. 1997;100:228-32.
7. Burgers R, de Jong TP, Visser M, Di Lorenzo C,
Dijkgraaf MG, Benninga MA. Functional defecation disorders in children
with lower urinary tract symptoms. J Urol. 2013;189:1886-91.
8. Borowitz SM, Cox DJ, Tam A, Ritterband LM, Sutphen
JL, Penberthy JK. Precipitants of constipation during early childhood. J
Am Board Fam Pract. 2003;16:213-8.
9. Bardisa-Ezcurra L, Ullman R, Gordon J; Guideline
Development Group. Diagnosis and Management of Idiopathic Childhood
Constipation: Summary of NICE Guidance. BMJ. 2010;340:c2585.
10. Gold DM, Levine J, Weinstein TA, Kessler BH,
Pettei MJ. Frequency of digital rectal examination in children with
chronic constipation. Arch Pediatr Adolesc Med. 1999;153:377-9.
11. Rockney RM1, McQuade WH, Days AL. The plain
abdominal roentgenogram in the management of encopresis. Arch Pediatr
Adolesc Med. 1995;149:623-7.
12. Pashankar D. Childhood constipation: evaluation
and management. Clin Colon Rectal Surg. 2005;18:120-7.
13. Chogle A, Saps M. Yield and cost of performing
screening tests for constipation in children. Can J Gastroenterol. 2013;27:e35-8.
14. Khanna V, Poddar U, Yachha SK. Etiology and
clinical spectrum of constipation in Indian children. Indian Pediatr.
2010;47:1025-30.
15. Bekkali NLH, van den Berg MM, Dijkgraaf MG, van
Wijk MP, Bongers ME, Liem O, et al. Rectal fecal impaction
treatment in childhood constipation: enemas versus high doses oral PEG.
Pediatrics. 2009;124:e1108-15.
16. Chen SL, Cai SR, Deng L, Zhang XH, Luo TD, Peng
JJ, et al. Efficacy and complications of polyethylene glycols for
treatment of constipation in children: A meta-analysis. Medicine
(Baltimore). 2014;93:e65.
17. Guest JF, Candy DC, Clegg JP, Edwards D, Helter
MT, Dale AK, et al. Clinical and economic impact of using
macrogol 3350 plus electrolytes in an outpatient setting compared to
enemas and suppositories and manual evacuation to treat paediatric
faecal impaction based on actual clinical practice in England and Wales.
Curr Med Res Opin. 2007;23:2213-25.
18. Gordon M, Naidoo K, Akobeng AK, Thomas AG.
Osmotic and stimulant laxatives for the management of childhood
constipation. Cochrane Database Syst Rev. 2012:11;7:CD009118.
19. Loening-Baucke V. Prevalence, symptoms and
outcome of constipation in infants and toddlers. J Pediatr.
2005;146:359-63.
20. Pijpers MA, Bongers ME, Benninga MA, Berger MY.
Functional constipation in children: A systematic review on prognosis
and predictive factors. J Pediatr Gastroenterol Nutr. 2010;50:256-68.
21. Bongers ME, van Wijk MP, Reitsma JB, Benninga
MA. Long-term prognosis for childhood constipation: clinical outcomes in
adulthood. Pediatrics. 2010;126: e156-62.
|
|
|
 |
|

