|
|
|
Indian Pediatr 2014;51:
829-830 |
 |
Chronic Hypoxemia in a Child: Thinking Outside
the Box
|
|
Barath Jagadisan, Sriram Krishnamurthy, Renitha
Raghavan and *S Deepak Barathi
From the Departments of Pediatrics and *Radiodiagnosis,
JIPMER, Pondicherry, India.
Correspondence to: Dr Sriram Krishnamurthy, Associate
Professor, Department of Pediatrics,
JIPMER, Pondicherry 605 006, India.
Email: [email protected]
Received: April 21, 2014;
Initial review: June 10, 2014;
Accepted: August 04, 2014.
|
|
Background: Chronic hypoxemia is
generally attributed to primary cardiac or pulmonary entities. Case
characteristics: A 9-year-old boy presenting with cyanosis, clubbing
and hypoxemia, without icterus or hepatosplenomegaly. Cardiovascular and
respiratory system examinations were normal. Outcome: He was
diagnosed as type IB Abernethy malformation, a rare cause of
hepatopulmonary syndrome. Message: Pediatricians should consider
hepatopulmonary syndrome in the differential diagnosis of chronic
hypoxemia, even in the absence of jaundice or hepatosplenomegaly.
Keywords: Abernethy malformation, Central
cyanosis, Clubbing, Hepatopulmonary syndrome.
|
|
Central cyanosis and clubbing is a child is mostly
due to congenital cyanotic heart disease or chronic pulmonary disease.
When cardiac and respiratory system examination is normal, it presents a
diagnostic challenge. We report an unusual cause of chronic hypoxemia in
a child that required extensive work-up before a diagnosis could be
made.
Case Report
A 9-year-old boy, resident of an orphanage, was
brought with history suggestive of upper respiratory infection. There
was no history of chronic cough, prolonged fever, breathlessness,
palpitations, chest pain, edema, jaundice, hematemesisor syncope. There
was no history of respiratory distress, cyanosis or hospitalization in
the past. There was no history of any drug intake or bleeding
manifestations. He was developmentally normal.
On examination, he was afebrile with a respiratory
rate of 18/min and pulse rate of 96/min. He had marked central cyanosis
and pan-digital clubbing. There was no icterus, lymphadenopathy, pallor
or edema. He weighed 19.3 kg (3rd centile for age) with height 123 cm
(between 3rd and 15th centile). Respiratory and cardiovascular system
examination was normal. There was no hepatomegaly or splenomegaly. The
oxygen saturation (SpO 2) was
84% in the upper limbs that improved to 94% with oxygen. The chest X-ray
showed plethoric lung fields; electro-cardiogram and echocardiogram were
normal.
Due to the absence of an intracardiac shunt or
pulmonary hypertension to explain the cyanosis, we investigated him for
an extracardiac shunt by injecting agitated saline intravenously. The
microbubbles appeared on the left side of the heart after the fourth
cardiac cycle, demonstrating an extracardiac shunt. Pulmonary computed
tomography (CT) angiography was performed which did not reveal any
extracardiac pulmonary shunt or pulmonary arteriovenous malformation.
There was also no evidence of chronic lung disease or bronchiectasis on
the CT scan. The partial pressure of oxygen (PaO 2)
was 41.1 mm Hg which improved to 46.5 mm Hg with oxygen. The change in
SpO2 with position was not
significant. The arterial alveolar oxygen gradient (AaDO2)
was elevated (88.2 mm Hg).
The liver function tests and prothrombin time were
normal. The packed cell volume was 45% (Hemoglobin 14 g/dL).
Ultrasonography of abdomen (including Doppler) showed a normal sized
liver with no focal lesions, nodularity or biliary dilatation. Right and
left branches of portal vein were atretic and replaced by an echogenic
strand of tissue. The main portal vein was patent and shown to drain
into the inferior vena cava (IVC). CT portovenography done to delineate
the vessels showed the formation of main portal vein (MPV) by confluence
of the superior mesenteric vein (SMV) and the splenic vein (SV) which
had an end to side communication with the IVC without branching into the
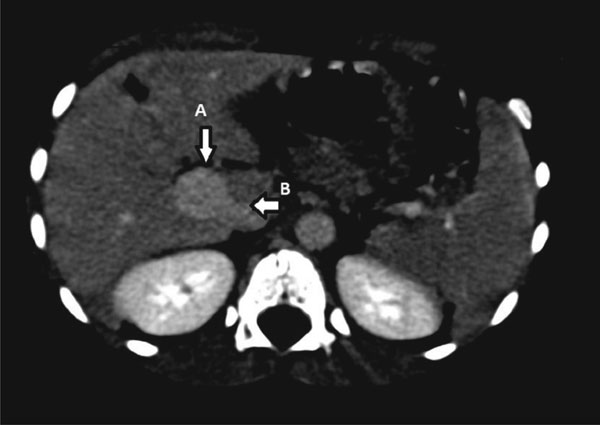
liver. Fig. 1 shows the abnormal communication between the
portal vein and inferior vena cava.
 |
|
Fig. 1 Axial section of contrast enhanced CT study
showing abnormal communication between the portal vein (arrow A)
and inferior vena cava (arrow B).
|
Based on these observations, the child was diagnosed
to have hepatopulmonary syndrome (HPS) due to Abernethy malformation
(type 1B). The caregivers of the child did not consent for liver biopsy,
and opted to get him discharged without further treatment.
Discussion
Abernethy malformation (type IB) with HPS is a rare
cause of hypoxemia which could pose a diagnostic challenge. The most
common causes of chronic central cyanosis and clubbing in children were
ruled out in our patient by appropriate investigations. Pulmonary
arteriovenous malformations (PAVM) and abnormal hemoglobin are uncommon
causes of cyanosis. PAVM in the pediatric age group may be a result of
hereditary hemorrhagic telangiectasia or HPS where it is referred to as
intrapulmonary vascular dilatation [1].
HPS in children is commonly a result of cirrhosis
[2]. Extrahepatic portal venous obstruction (EHPVO), which is a
non-cirrhotic disease, is a very rare cause of HPS [3].The development
of HPS in EHPVO is a classic example of how redirection of blood flow
away from the liver by collateral flow leads to absence of hepatic
handling of unknown circulating factors in portal blood and thereby HPS.
The case under discussion is an extension of the same concept where the
uncommon Abernethy malformation leads to HPS by virtue of shunting blood
away from the liver [4-6].
Abernethy malformation is a rare cause of
hepatopulmonary syndrome [7], characterized by congenital extrahepatic
portosystemic shunts (CEPS) [8]. They have been classified as type 1
when the intrahepatic portal branches are absent and the portal blood
completely empties into the systemic vessels, either directly through
the SMV and SV (type 1A) or after forming the portal vein (type 1B) as
in our case [9]. In type 1, SpO 2
improves with inhaled oxygen as in our case. In type 2 CEPS, the
intrahepatic portal branches are patent and the portosystemic
communication is a side- to- side communication between the portal vein
and the systemic circuit [9]. With the easy availability of ultrasound,
the diagnosis of CEPS is often incidental. CEPS may also manifest with
growth restriction, focal nodular hyperplasia, malignant transformation
of the hepatic nodules, hepatic encephalopathy, HPS or brain abscess.
The management of CEPS is surgical. Liver transplantation (including
auxiliary partial orthotopic liver transplantation) may be the only
option in some cases [10].
To conclude, this case demonstrates the serial
analysis and work-up of an unusual cause of central cyanosis and
clubbing due to type IB Abernethy malformation with HPS. HPS should be
considered in the differential diagnosis of central clubbing and
cyanosis of non-cardiopulmonary origin.
Contributors: All authors were involved in
patient management and contributed to review of literature. BJ, SK:
drafted the manuscript; SDB: interpreted the radiological findings. All
authors approved the final version of the manuscript.
Funding: None; Competing interests: None
stated.
References
1. Ho V. Current concepts in the management of
hepatopulmonary syndrome. Vasc Health Risk Manag. 2008;4:1035-41.
2. Barbé T, Losay J, Grimon G, Devictor D, Sardet A,
Gauthier F, et al. Pulmonary arteriovenous shunting in children
with liver disease. J Pediatr. 1995;126:571-9.
3. Gupta D, Vijaya DR, Gupta R, Dhiman RK, Bhargava
M, Verma J, et al. Prevalence of hepatopulmonary syndrome in
cirrhosis and extrahepatic portal venous obstruction. Am J Gastroenterol.
2001;96:3395-9.
4. Alvarez AE, Ribeiro AF, Hessel G, Baracat J,
Ribeiro JD. Abernethy malformation: one of the etiologies of
hepatopulmonary syndrome. Pediatr Pulmonol. 2002;34:391-4.
5. Tercier S, Delarue A, Rouault F, Roman C, Bréaud
J, Petit P. Congenital portocaval fistula associated with
hepatopulmonary syndrome: ligation vs liver transplantation. J Pediatr
Surg. 2006;41:e1-3.
6. Morikawa N, Honna T, Kuroda T, Kitano Y, Fuchimoto
Y, Kawashima N, et al. Resolution of hepatopulmonary syndrome
after ligation of a portosystemic shunt in a pediatric patient with an
Abernethy malformation. J Pediatr Surg. 2008;43:e35-8.
7. Kinane TB, Westra SJ. A four-year-old boy with
hypoxemia. N Engl J Med. 2004;351:1667-75.
8. Alonso-Gamarra E, Parrón M, Pérez A, Prieto C,
Hierro L, López-Santamaría M. Clinical and radiologic manifestations of
congenital extrahepatic portosystemic shunts: a comprehensive review.
Radiographics. 2011;31:707-22.
9. Morgan G, Superina R. Congenital absence of the
portal vein: two cases and a proposed classification system for
portasystemic vascular anomalies. J Pediatr Surg. 1994;29:1239-41.
10. Emre S, Arnon R, Cohen E, Morotti RA, Vaysman D,
Shneider BL. Resolution of hepatopulmonary syndrome after auxiliary
partial orthotopic liver transplantation in Abernethy malformation. A
case report. Liver Transpl. 2007;13:1662-8.
|
|
|
 |
|

