A
lveolar capillary dysplasia (ACD) is a rare
cause of irreversible persistent pulmonary hypertension. Fewer than
50 cases have been described since the first description by Janney,
et al. [1] in 1981 as a misalignment of pulmonary veins [2,3].
The etiology of disordered alveologenesis is not yet clearly
understood. Clinically, there are signs of respi-ratory failure not
responding to therapy. The definitive diagnosis can be established by
a lung biopsy [4].
Case Report
A full term 2700 g male infant was born by normal
vaginal delivery at the 38 week gestation after uncomplicated
pregnancy, with Apgar score 6/9/9. The physical examination detected
anorectal atresia and surgical treatment was planned. Preoperative
echocardiographic examination did not detect any structural
abnormality. Baby did not have tricuspid regurgitation sufficient to
generate a measurable signal. There was bidirectional (predominantly
left-to-right) shunting at the ductus arteriosus and foramen
ovale. The value of right ventricular pre-ejection period /
right-ventricular ejection time (PEP/RVET) measured by pulsed doppler
at the pulmonary valve was 0.4. The surgery was uneventful but a
short time bronchial hyperactivity appeared during induction of
anesthesia. After surgery, the infant required mechanical ventilation
with FiO2 0.21-0.3 for 18
hours. On the third postoperative day, the baby was intubated because
of dyspnea and impaired oxygenation despite the CPAP treatment. FiO
2
required was 1.0. One day later, there was a progression of severe
respiratory failure not responding to any therapy. The X-ray
examination of the chest did not reveal any pathological changes.
Despite resuscitation, mechanical ventilation, and cardiotonic
support, the infant died at the age of six days. Autopsy revealed a
patent foramen ovale and ductus arteriosus as a result of persistent
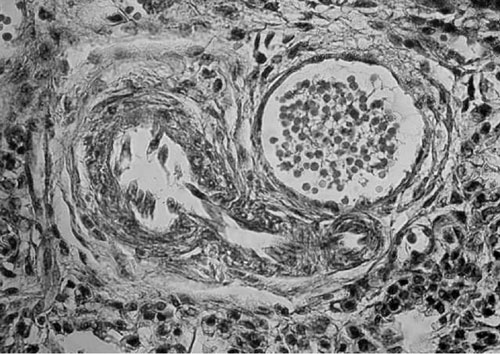
pulmonary hypertension (PPHN) Edwards stage I –II. Histological
examination diagnosed ACD with reduction of capillaries, apposition
of pulmonary veins and thickened alveolar-capillary septum (Fig.
1).
 |
|
Fig. 1 Histological signs of
alveolar capillary dysplasia with hypertrophy of arterial media
and dysplastic vein pass along pulmonary artery sharing common
adventitia. |
Discussion
ACD is a rare lethal condition that has
been recognized in recent years as a cause of idiopathic PPHN. The
prevalence of ACD is not exactly known [1]. Occasional familiar
clustering and documented associations with other non-lethal
congenital anomalies, most frequently of genitourinary and
gastrointestinal tracts, have been reported [1,2,5]. Chang, et al.
and coauthors confirmed the deficiency of immunoreactivity of CD 117
hemangioblast precursor cells in lung tissue, which during
physiological circumstances produce chemo-reactive substances
responsible for vasculogenesis and formation of alveolo-capillary
membrane. There is a lack of expression of VEGF isoforms. Principal
pathomechanism of the disease is a failure of alveologenesis and
formation of blood-gas barrier. Histological analysis reveals
misalignment of pulmonary veins, dysplastic capillaries, hypertrophy
of pulmonary arteries, lymphangiectasis, and thickened alveolar –
capillary septum [7]. In physiological circumstances, pulmonary veins
are localized at the periphery of the lobule within interlobular
septa. In ACD, they pass along pulmonary arteries, sharing common
adventitia in the centre of lung lobule. It is likely that large
abnormal capillaries are immature vessels that are arrested at an
earlier step of vessels development and have not differentiated into
the smaller and more mature size [1, 8]. The dysplastic capillaries
may also fail to connect with the pulmonary arteries upstream, which
would explain why they are thick-walled in ACD [8].
The pathophysiology of ACD is unclear. It is
postulated that reduced number of pulmonary capillaries, hypoxic
vasoconstriction and altered vasoreactivity are causes of pulmonary
hypertension. The resulting increased right-sided pressure may lead
to right to left shunting across patent foramen ovale or ductus
arteriosus.
In 50% of cases, pulmonary hypertension progresses
within first 24 hours, in other 50% the symptoms develop within
several weeks called "the initial honeymoon period". The reason for
this period is unknown [9]. This relatively delayed presentation
could be ascribed to phenotypical variation of the disease, patchy
involvement of lungs or unexpected opening of shunts between
pulmonary arteries and veins [6]. Clinical presentation of ACD is
nonspecific. There are signs of respiratory failure with developing
hypoxemia. X-ray examination is frequently without
pathological changes. Sometimes bilateral nonspecific infiltrative
changes may be present. A variable stage of pulmonary hypertension
with right to left shunting and tricuspidal insufficiency can be
diagnosed by echocardiographic examination [10].
In our patient, the echocardiography was normal in
the preoperative period. Due to a rapid deterioration of clinical
condition of the baby there was no time left to repeat the
echocardiography.
ACD is a universally lethal disease. All the
aggressive therapies including inhaled nitric oxide, mechanical
ventilation and ECMO may only reduce transient hypoxemia but do not
lead to a long term survival. ACD should be suspected in newborns
with respiratory distress that is not responding to the therapy,
especially when other congenital anomalies are present. It is
recommended to consider early lung biopsy to reduce the number of
invasive, expensive and futile procedures that do not improve the
likelihood of survival [8].
Contributors: ZB collected the data and
drafted the paper. KM revised the manuscript for intellectual
content. AJ conducted the echocardiography and interpreted the
results. MZ acted as a guarantor of the study. The final manuscript
was approved by all authors.
Funding: Comenius University grant No.
37/2009 and VEGA grant.
Competing interests: None stated.
References
1. Janney CG, Askin FB, Kuhn G. Congenital
alveolar capillary dysplasia – an unusual cause of respiratory
distress in the newborn. Am J Clin Pathol.
1981;76:722-7.
2. Al-Hathol K, Philps S, Seshia M, Casiro O,
Alvaro RE, Rigatto H. Alveolar capillary dysplasia. Report of a case
of prolonged life without ECMO and review of the literature. Early
Hum Dev. 2000;57:84-5.
3. Thibeault DW, Garola RE, Kilbride HW. Alveolar
capillary dysplasia: An emergeting syndrome. J Pediatr.
1999;134:661-2.
4. Antao B, Samuel L, Kiely E, Spitz L, Malone M.
Congenital alveolar capillary dysplasia and associated
gastrointestinal anomalies. Fetal Pediatr Pathol.
2006;25:137-45.
5. Tibbalas J, Chow CW. Incidence of alveolar
capillary dysplasia in severe idiopatic persistent pulmonary
hypertension of the newborn. J Paediatr Child Health.
2002;38:397-400.
6. Chang KT, Rajadurai VS, Walford NQ, Hwang WS.
Alveolar capillary dysplasia: Absence of CD117 immunoreactivity of
putative hemangioblast precursor cells. Fetal Pediatr Pathol.
2008;27:27-140.
7. Ng PC, Lewindon PJ, Siu LK, To KF,Wong W.
Congenital misalignment of pulmonary veins : un usual syndrome
associated with PPHN. Acta Pediatr. 1995;84:349-53.
8. Galambos C, DeMello DE. Regulation of
alveologenesis : Clinical implications of impaired growth. Pathol.
2008;40:124-40.
9. Shioe A, Lee A, To K, Thumg KH, Lee TW, Yim A.
Alveolar capillary dysplasia with congenital misalignment of
pulmonary veins. Asian Cardiovas Thor Annalas. 2005;13:82-4.
10. Shankar V, Haque A, Johnson J, Pietsch J. Late presentation
of alveolar capillary dysplasia in an infant. Pediatr Crit Care.
2006;7:177-9.

