|
|
|
Indian Pediatr 2011;48: 797-799 |
 |
Prevalence and Annual Risk of Tuberculosis
Infection in Rural Mysore |
|
K Jagadish Kumar, P Prakash, D Srinivasa Murthy And VG Manjunath
From the Department of Pediatrics, JSS Medical College,
JSS University, Mysore and *District Hospital, Chikkaballapur.
Correspondence to: Dr K Jagadish Kumar, Professor of
Pediatrics, JSS Medical College, JSS University, Mysore.
Email: [email protected]
Received: November 22, 2010;
Initial review: December 15, 2010;
Accepted: January 11, 2011.
Published online: 2011 May 30.
PII:S0974755INPE1000453-2
|
|
Abstract
We carried out a tuberculin survey among 5-10 years
old children in rural Mysore (n=1026) to estimate the annual risk
of tuberculosis infection (ARTI). 90.8%of them had BCG scar. The
prevalence of infection was estimated as 13.3% with 95% CI of 11.4-15.5
and ARTI as 1.38% .These figures are comparatively higher than what is
reported from other places in India.
Key words: Annual Risk of Tuberculosis infection, India,
Prevalence.
|
|
T
uberculin survey is the time
tested
epidemiological tool to detect TB
infection in children [1-3]. Annual risk of
tuberculosis infection (ARTI), used widely as the surrogate measure of
incidence, is defined as the probability of acquiring a new TB infection
during the course of 1 year and is computed from estimated prevalence of
infection among younger children [3,4]. We carried out this survey to
ascertain the prevalence of tuberculosis and ARTI in children belonging to
rural Mysore. Little information is available in this regard from
Karnataka, other than from Bangalore [5,6].
Methods
This cross sectional study was undertaken during
May-July 2005 in a rural school near Mysore among children between 5-10
years of age. Ethical clearance was obtained from ethical review committee
of JSS medical college. Written consent was taken after explaining the
study. Children were enrolled according to the attendence register.
Children were examined by a pediatrician. Anthro-pometry and BCG scar
status were entered in the proforma. Those who were on ATT were excluded
from the study.
Tuberculin administration: Children were given PPD-S
0.1 mL of the standard 1 TU of PPD RT23 intradermally on the volar aspect
of the forearm. The tuberculin test was read after 72 hours of injection.
The maximum transverse diameter was measured with pen and platic ruler
method. Tuberculin reaction sizes obtained were arranged in the form of
frequency distribution table and converted to the graph to identify the
mode and antimode of reactions. We used Prism’s graph pad version 3 for
calculating prevalence and its confidence interval.
Results
A total of 1057 children aged between 5-10 years were
enrolled in the study. Out of them only 1026 came back for tuberculin
reading. Of these children 932 (90.8%) had BCG scar. Table I
depicts the age distribution of registered children. The frequency
distribution of reaction sizes among all children is shown in the
Fig. 1.
TABLE I Age Distribution of Registered Children
| Age (y) |
No of children |
% |
| 5 |
42 |
4.1 |
| 6 |
75 |
7.3 |
| 7 |
120 |
11.7 |
| 8 |
163 |
15.9 |
| 9 |
118 |
11.5 |
| 10 |
508 |
49.5 |
| Total |
1026 |
100.0 |
|
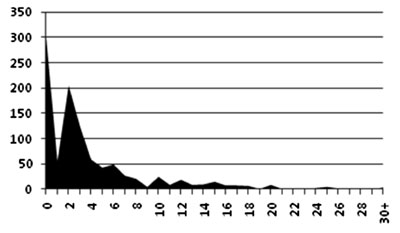
Tuberculin reaction size in mm
|
|
Fig. 1 Frequency distribution of tuberculin
reaction sizes in children. |
The frequency distribution with reaction size on the
x-axis was found to be bimodal with antimode at 9mm. This was taken as
cut-off. The prevalence of tuberculosis was calculated to be 13.3% (95%
CI: 11.4-15.5). Annual risk of tubercular incidence was calculated to be
1.38, presuming the average age of participants as 7.5 years.
Discussion
The prevalence rate of infection was estimated as 13.3%
with 95% CI of 11.4-15.5. ARTI calculated was 1.38% in the present study.
Comparative National level ARTI is 1.5%, and from South, East, West and
North India is, 1.1%, 1.3%, 1.8% and 1.9%, respectively [1,5-7]. A similar
study from Bangalore reported the prevalence to be 8.08% and 8.6% for
unvaccinated and vaccinated children, respectively. The estimated ARTI in
that study was 1.12% and 1.19% in unvaccinated and vaccinated children,
respectively [8]. Another study from Trivandrum reported ARTI of 0.75% in
2000 [3]. Similar study by Chadha, et al. [6] in 2006 has reported
a prevalence of 9.8% and ARTI of 1.5%. Another recent study in 2010 from
tribal population of Madhya Pradesh has reported a prevalence of 6.3% and
ARTI of 1.2% [9]. The variablity of the prevalence between these studies
could be attributed to regional differences in the extent of tuberculosis,
methodology in using tuberculin and because of better performance of
health care systems. Our study children belonged to the lowest
socioeconomic class. This could explain the higher prevalence in this
group.
Studies have shown that tuberculin surveys among 5-9
years help in estimating the ARTI irrespective of BCG coverage. They have
suggested that in areas of high BCG coverage, results of tuberculin
testing among vaccinated and unvaccinated can be combined [8,10,11].
Therefore, we did not attempt to study prevalence rates and ARTI amongst
vaccinated and unvaccinated groups separately.
Acknowledgments: Headmaster, teachers and all the
children of JSS school, Suttur, Mysore and Dr D Narayanappa for his
constant encouragement.
Contributors: KJK: Conceived and designed the study
and revised the manuscript for important intellectual content. He will act
as guarantor of the study; KJK, VG and PP: collected data and drafted the
paper.; PP and VG: also conducted the tests, and interpreted them; DS:
analysed the data and helped in manuscript writing. The final manuscript
was approved by all authors.
Funding: None.
Competing interests: None stated.
|
What this Study Adds?
• This study provides baseline information of
prevalence and ARTI in rural Mysore and highlights the high
prevalence in this population compared to similar population in
south India.
|
References
1. Chadha VK, Agarwal SP, Kumar P, Chauhan LS, Kollapan
C, Jaganath PS, et al. Annual risk of infection in four defined
zones of India: a comparative picture. Int J Tuberc Lung Dis.
2005;9:569-75.
2. Chakraborty AK. Epidemiology of tuberculosis:
Current status in India. Indian J Med Res. 2004;120:248-76.
3. Kumari Indira KS, Sivaraman S, Joshi M, Pillai NS.
Annual risk of tuberculosis infection; An estimate from ten year old
children in Trivandrum district. Indian J Tuberc. 2000;47:211-17.
4. Savanur SJ, Chadha VK, Jagannatha PS. Mixture model
for analysis of tuberculin surveys. Indian J Tuberc. 2002;49:147-52.
5. Chadha VK, Jagannatha PS, Savanur SJ. Annual risk of
tuberculosis infection in Bangalore city. Indian J Tuberc. 2001;48:63-71.
6. Chadha VK, Jithendra R, Kumar P, Kirankumar R, Shashidharan
AN, Suganthi P, et al. Change in the risk of tuberculous infection
over an 8-year period among schoolchildren in Bangalore City. Int J Tuberc
Lung Dis. 2008;12:1116-21.
7. Central TB Division. Managing the Revised National
Tuberculosis Control Programme in Your Area—Training Course 2005.New
Delhi, India: Directorate General of Health Services, Ministry of Health
and Family Welfare; 2005.
8. Chadha VK, Jagannath PS, Suryanarayana HV.
Tuberculin sensitivity in BCG vaccinated children and its implication for
ARI estimation Indian J Tuberc. 2000; 47:139-46.
9. Yadav R, Rao VG, Bhat J, Gopi PG, Wares DF. Annual
risk of tuberculosis infection among the tribal children of Jhabua, Madya
Pradesh. Indian Pediatr. 2010 [E-pub ahead of print].
10. Chadha VK, Jagannatha PK, Kumar P. Can
BCG-vaccinated children be included in tuberculin surveys to estimate the
annual risk of tuberculous infection in India? Int J Tuberc Lung Dis.
2004;8:1437-42.
11. Gopi PG, Subramani R, Kolappan C, Venkatesh Prasad
V, Narayanan PR. Estimation of annual risk of tuberculosis infection among
children irrespective of BCG scar in the south zone of India. Indian J
Tuberc. 2006;53:7-11.
|
|
|
 |
|

