Fusiform dilatation of vessels of circle of Willis to form large
aneurysms, termed "Cerebral Aneurysmal Childhood Arteriopathy", is an
exceedingly rare complication of pediatric HIV(1). We report one such case
in a 12-year-old-child with WHO clinical-stage-4 HIV disease, who was
admitted with complaints of headache and right hemiparesis.
He was diagnosed with vertically acquired HIV infection
at age of 2-years. There was no previous history of neurologic symptoms or
neurocognitive dysfunction. He was on antiretroviral treatment (ART) since
last 4 months and his recent CD4-cell-counts were 217 cells/µL. A magnetic
resonance imaging (MRI) of the brain revealed an aneurysm of the
supraclinoid portion of left internal carotid artery (ICA). A cranial
magnetic resonance angiographic scan was consistent with intracranial
arteritis and revealed a large fusiform aneurysm of the left ICA beyond
the common siphon (Fig. 1). Because of the surgical risk, no
intervention was attempted. He is on ART and continues to be monitored
closely for improvement.
 |
|
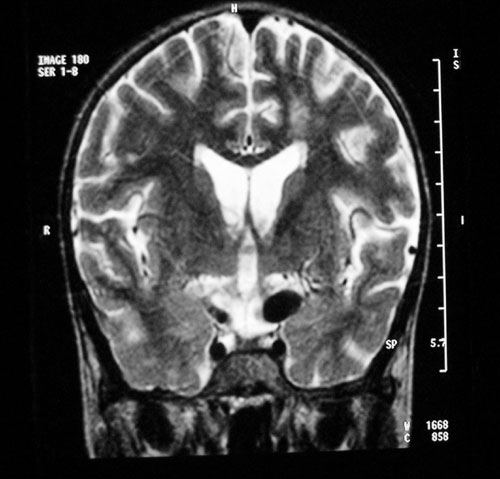
Fig. 1 T2W Coronal Section of Magnetic
Resonance Angiography (MRA) Brain showing a flow void in the left
internal carotid artery (arrow). The left internal carotid artery
appears dilated and ectatic suggestive of fusiform aneurysm of left
internal carotid artery. |
There is an increased incidence of cerebrovascular
disease in HIV infected children who are severely immunosuppressed
(CD4-counts < 200 cells/µL) and who acquire the infection vertically or in
the neonatal period(2). The formation of fusiform aneurysm has been
described previously(3), and it may be a feature specific to AIDS(4).
The proximal segments of middle and anterior cerebral arteries and
the supraclinoid segment of ICA (as in our patient) are the most common
sites for aneurysms(2). Vascular immaturity is
suggested as a possible contributory factor(2).
Most of these patients are asymptomatic during the
early stages of the disease(2). With severe
immunosuppression and usually after infancy, they present with an acute
intracerebral event(5). Hence, screening of high risk children, preferably
by MRI, is advisable for the early detection of cerebrovascular
abnormalities(2). The fusiform nature and location of these aneurysms
makes any form of surgical intervention or embolization impossible(1).
Early detection and intervention with ART could prevent entirely or
diminish the incidence and severity of cerebral vasculopathy(2).
Acknowledgment
Dr Mamta V Manglani, Professor and Head, Department of
Pediatrics for her guidance.
References
1. Mahadevan A, Tagore R, Siddappa NB, Santosh V, Yasha TC,
Ranga U, et al. Giant serpentine aneurysm of vertebrobasilar artery
mimicking dolichoectasia: an unusual complication of pediatric AIDS.
Clinical Neuropathol 2008; 27: 37-52.
2. Patsalides AD, Wood LV, Atac GK, Sandifer E, Butman
JA, Patronas NJ. Cerebrovascular disease in HIV- infected pediatric
patients: Neuroimaging Findings. AJR Am J Roentgenol 2002; 179: 999-1003.
3. Park YD, Belman AL, Kim TS, Kure K, Llena JF, Lantos
G, et al. Stroke in pediatric immuno-deficiency syndrome. Ann
Neurol 1990; 28: 303-311.
4. Shah SS, Zimmerman RA, Rorke LB, Vezina LG.
Cerebrovascular complications of HIV in children. AJNR 1996; 17:
1913-1917.
5. Dubrovsky T, Curless R, Scott G, Chaneles M, Altman
N, Petito CK, et al. Cerebral aneurysmal arteriopathy in childhood
AIDS. Neurology 1998; 51: 560-565.

