|
|
|
Indian Pediatr 2009;46: 903-906 |
 |
Day 1 Blood Glucose and Outcome in Critically
Ill Children |
|
N Suresh, R Ganesh, Janani Sankar and Malathi Sathiyasekaran
From the Departments of Pediatrics and Gastroenterology,
Kanchi Kamakoti CHILDS Trust Hospital, 12-A, Nageswara road, Nungambakkam,
Chennai 600 034, Tamil Nadu, India.
Correspondence to: Dr N Suresh, Senior Registrar in
Pediatrics, Kanchi Kamakoti CHILDS Trust Hospital, 12- A, Nageswara Road,
Nungambakkam, Chennai 600 034, Tamil Nadu, India.
Email:
[email protected]
Manuscript received: September 26, 2008;
Initial Review: October 18, 2008;
Accepted: December 8, 2008.
|
|
Abstract
Primary intestinal lymphangiectasia (PIL) is a rare
disease of intestinal lymphatics presenting with hypoproteinemia,
bilateral lower limb edema, ascites, and protein losing enteropathy . We
report a series of 4 children from Chennai, India presenting with
anasarca, recurrent diarrhea, hypoproteinemia and confirmatory features
of PIL on endoscopy and histopathology.
Key words: Hypoproteinemia, Intestinal lymphangiectasia,
Protein losing enteropathy, Waldmann’s disease.
|
|
I
ntestinal lymphangiectasia (IL) is
an important cause of protein losing enteropathy (PLE) characterized by
diffuse or local ectasia of the enteric lymphatics, often in association
with extraintestinal lymphatic abnormalities. Waldmann and Schwabb in 1961
reported this rare entity with intestinal protein loss leading to
hypoproteinemia and anasarca(1). IL can be either primary (idiopathic) or
secondary. Primary intestinal lymphangiectasia (PIL) usually occurs in
children and adolescents, due to the congenital deformity of the small
bowel lymphatic system, whereas secondary intestinal lymphangiectasia is
more often seen in adults and occurs secondary to an elevated lymphatic
pressure as in lymphoma, systemic lupus erythematosus, inflammatory bowel
disease, malignancies, constrictive pericarditis, and cardiac
surgery(2,3).
Case Report
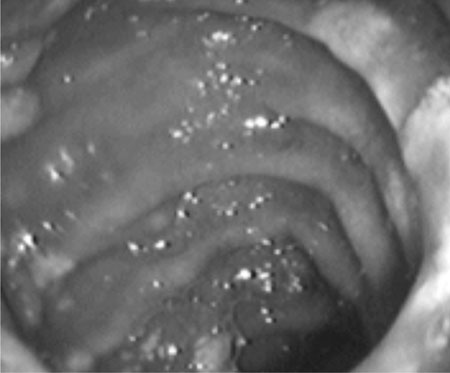
Case 1: A 8 year old girl presented with history of
recurrent small bowel diarrhea and anasarca from the age of 5 years.This
illness was not associated with fever, vomiting, abdominal pain, rash,
arthralgia or urinary symptoms.There was no history of contact with
tuberculosis. The present hospitalization was for swelling of hands and
feet which had increased with worsening of diarrhea. She was first born to
non-consanguineous parents, with a birth weight of 3.5 kgs and was
apparently well till 5 years of age. On examination, she had generalized
anasarca and her vitals and systems examination were normal. She weighed
21.6 kgs as against 26 kg. Biochemical and hematological profile is
summarized in Table I. USG abdomen showed ascites and
bilateral pleural fluid. Barium meal and follow through demonstrated
coarse mucosal folds and flocculation in the small intestine. Her lipid
profile was normal except for low HDL levels. The characteristic "snow
flake appearance" of the duodenum was seen on upper gastrointestinal
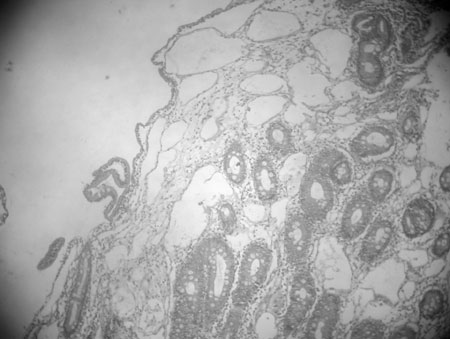
endoscopy (Fig. 1). Dilated lymphatics, the typical
histopathological feature of IL was reported in the duodenal biopsy (Fig
.2). She was given medium chain triglycerides (MCT) based diet
supplemented with albumin transfusions. Diarrhea and anasarca improved
over 2 weeks but she succumbed later at the age of 8 years and 6 months
due to an intercurrent viral illness.
 |
 |
|
Fig. 1 Upper gastrointestinal endoscopy of
duodenum showing the snow flake appearance. |
Fig. 2 Histopathology of small intestine
showing the grossly dilated lymphatics in lamina propria the
hallmark of intestinal lymphangiectasia. |
TABLE I
Clinical and Laboratory Details of 4 Children with Primary Intestinal Lymphangiectasia
| |
Case 1 |
Case 2 |
Case 3 |
Case 4 |
| Age at diagnosis |
8 Yrs |
9Yrs |
36 day of life |
5yrs |
| Gender |
Female |
Female |
Male |
Male |
| Age of onset |
5 yrs |
9 yr |
day 5 |
1 year |
| Hemoglobin (g/dL) |
13.5 |
11.6 |
12.2 |
8 |
| WBC (cells/cmm) |
10,000 |
6500 |
8500 |
4100 |
| Differential count |
P68,L22,E8,M1 |
P54,L44,B2 |
P65,L30,E5 |
P55,L45 |
| Serum bilirubin (mg/dL) |
0.4 |
0.5 |
0.3 |
0.2 |
| SGOT (IU/L) |
40 |
24 |
40 |
40 |
| SGPT (IU/L) |
35 |
23 |
35 |
40 |
| Serum proteins(g/ dL) |
3.6 |
3.6 |
2.8 |
3.8 |
| Serum albumin (g/dL) |
2.3 |
2.3 |
2 |
1.7 |
| Serum globulin (g/dL) |
1.3 |
1.3 |
0.8 |
2.1 |
| Serum IgA (mg/dL) |
90 |
41 |
10 |
165 |
| Serum IgG (mg/dL) |
700 |
561 |
35 |
800 |
| Serum IgM (mg/dL) |
120 |
189 |
14 |
49 |
| Serum IgE (IU/ML) |
160 |
59 |
2 |
70 |
| Cholesterol (mg/dL) |
133 |
75 |
79 |
163 |
| HDL (mg/dL) |
25 |
16 |
45 |
36 |
| LDL(mg/dL) |
81 |
47 |
80 |
80 |
| VLDL(mg/dL) |
27 |
12 |
22 |
23 |
| TGL (mg/dL) |
100 |
60 |
48 |
50 |
| HIV Elisa |
Non reactive |
Non reactive |
Non reactive |
Non reactive |
| T cell workup |
Not done |
Not done |
Normal |
Not done |
| Barium meal |
Malabsorptive |
Malabsorptive |
Malabsorptive |
Malabsorptive |
| |
pattern |
pattern |
pattern |
pattern |
| Snow flake appearance in UGIE |
Yes |
Yes |
Yes |
Yes |
| Biopsy proven lymphangiectasia |
Yes |
Yes |
Yes |
Yes |
Case 2: A 9 year old female, presented with
anasarca and recurrent loose stools suggestive of small bowel diarrhea for
20 days. She was first born of non consanguineous parents and remained
apparently well till 9 years of age except for body asymmetry. The right
side of her body including her extremities and face was noted to be more
prominent than the left. She had minimal motor delay and poor scholastic
performance. On examination her face was dysmorphic with depressed nasal
bridge, puffy eyelids and small mouth. She had asymmetrical generalized
edema with lymphedema involving the right side of her body including the
genitalia and both feet. Her blood pressure and systems examination were
normal. A diagnosis of Hennekman Syndrome was made based on the phenotypic
features. Investigations are summarized in Table I. She was
managed with albumin transfusions, low fat with MCT diet and genetic
counseling was offered to the parents.
Case 3: A 36 day old male infant presented
with diarrhea and anasarca since 5 th
day of life. His vitals including blood pressure and other systems
examination were normal. Investigations are shown in Table I.
He was managed with albumin infusions, formula milk containing high MCT
and partial parenteral nutrition. The child showed some response to
treatment. He is on regular follow up but requires repeated
hospitalizations for diarrhea and anasarca.
Case 4: A 5 year old male presented with
history of recurrent small bowel diarrhea associated with anasarca since 1
year of age. He was hospitalized thrice for similar complaints. There was
no rash, arthralgia, joint pains or contact with tuberculosis. He was
alert and had anasarca. Investigations are shown in Table I.
He was given MCT based diet and albumin infusions following which he
responded and is on regular follow up.
Discussion
Primary intestinal lymphangiectasia (PIL) or Waldmann’s
disease is characterized by malformation of lymphatics leading to
obstruction, rupture and leak of lymph fluid into the bowel lumen
resulting in hypoalbuminemia, lymphopenia and hypogammaglobulinemia(3).
The clinical features of PIL are bilateral lower limb edema, ascites, and
chronic diarrhea which was seen in all our 4 cases. The lung, uterus and
conjunctiva may also be involved in IL(4,5). Necrolytic migratory erythema,
osteomalacia, recurrent gastrointestinal bleeding and recurrent hemolytic
uremic syndrome can occur in patients with PIL(3). PIL is generally
diagnosed before 3 years of age but may be diagnosed in older children and
adults as in our series, where 3 children were diagnosed beyond the age of
5 years(6). The etiology of PIL still remains unknown.
The syndromes linked with intestinal lymphangectasia
include Von Recklinghausen, Turner, Noonan, Klippel Trenaunay, Hennekam
and Yellow nail(3). In our case series, one child had features suggestive
of Hennekam syndrome (characteristic facial abnormalities, developmental
delay, severe limb and facial lymphedema)(7). IL has been associated with
celiac disease. Diagnosis of intestinal lymphangiectasia is established by
the characteristic histology of grossly dilated lymphatics seen in the
lamina propria of the small bowel (duodenum/jejunum/ileum). The villi may
be distorted and enlarged but usually without atrophy(6). Endoscopy may be
normal if the involvement is patchy and in such cases videocapsule
endoscopy helps in localization(8). The immunological abnormalities
reported in PIL are reduced immunoglobulin levels (IgG, IgA, IgM), low CD
4+ T cells, lymphocytopenia, skin allergy and graft rejection(3,9). In our
series only 2 children had low immunoglobulin levels.
Life long dietary modification with high protein,
restricted fat substituted with medium chain triglycerides (MCT) and
vitamin supplements remains the cornerstone in the management of PIL.
Exclusion of long chain fatty acids prevents the engorgement and rupture
of malformed lymphatics while MCT get directly absorbed into the portal
venous circulation(3). In case of poor response to this treatment partial
or total parenteral nutrition should be considered. Other treatment
modalities described in literature with variable efficacy include
antiplasmin therapy, octreotide, corticosteroids, small bowel resection,
albumin infusions, peritoneo venous shunt (Levine) and intestinal
transplant(3).
Acknowledgment
Dr Meera Govindarajan, Pathologist, R & D Diagnostic
Laboratory, Chennai for histopathology.
Contributors: NS and RG prepared the
manuscript. JS reviewed the literature. MS reviewed and revised the
manuscript.
Funding: None.
Competing interests: None stated.
References
1. Waldmann TA, Steinfeld JL, Dutcher TF, Davidson JD,
Gordon RS. The role of gastrointestinal system in "Idiopathic
hypoproteinemia". Gastroenterology 1961; 41: 197-207.
2. Fang YH, Zhang BL, Wu JG, Chen CX. A primary
intestinal lymphangiectasia patient diagnosed by capsule endoscopy and
confirmed at surgery : A case report. World J Gastroenterol 2007;13:
2263-2265.
3. Vignes S, Bellanger J. Primary intestinal
lymphangiectasia (Waldmann’s disease).Orphanet Rare Dis 2008; 3: 5.
4. Lee WS, Boey MCC, Goh TAY, Chang KW, Iyngkaran N.
Intestinal lymphangiectasia – A report of three Chinese children in
Malaysia . Singapore Med J 1998; 39: 418-421.
5. Mucuke J, Hoepffner W, Scheerschmidt G, Gornig H,
Beyreiss K. Early onset lymphedema, recessive form – a new form of genetic
lymphedema syndrome. Eur J Pediatr1986; 154: 195-198.
6. Tift WL, Lloyd JK. Intestinal lymphangiectasia long
term results with MCT diet. Arch Dis Child 1975; 50: 269-276.
7. Hennekam RC, Geerdink RA, Hamel BC, Hennekam FA,
Kraus P, Rammeloo JA, et al. Autosomal recessive intestinal
lymphangiectasia and lymphedema with facial anomalies and mental
retardation. Am J Med Genet 1989; 34: 593-600.
8. Chamouard P, Nehme-Schuster H, Simler JM, Finck G,
Baumann R, Pasquali JL. Videocapsule endoscopy is useful for the diagnosis
of intestinal lymphangiectasia. Dig Liver Dis 2006; 38: 699-703.
9. Heresbach D, Raoul JL, Genetet N, Noret P,
Siproudhis L, Ramee MP, et al. Immunological study in primary
intestinal lymphangiectasia. Digestion 1994; 55: 59-64.
|
|
|
 |
|

