|
|
|
Indian Pediatr 2009;46: 891-894 |
 |
Breastfeeding Practices of Urban and Rural
Mothers |
|
A Oommen, M Vatsa, VK Paul and R Aggarwal
From the College of Nursing and Department of Pediatrics,
All India Institute of Medical Sciences, New Delhi, India.
Correspondence to: Dr Manju Vatsa, Principal, College of
Nursing, All India Institute of Medical Sciences, New Delhi, India.
Email: mvatsa2001@yahoo.co.in
Manuscript received: January 2, 2008;
Initial review: February 11, 2008;
Accepted: September 9, 2008.
Published online 2009 April 15. PII:S097475590800008-2
|
|
Abstract
This longitudinal study was conducted to describe the
prevalence of exclusive breastfeeding and factors influencing it in
urban (tertiary care hospital of Delhi) and rural (First Referral Unit
in Haryana) settings. The exclusive breastfeeding rates were 38%, 30%,
24%, 20%, 16% and 1% at discharge, 1.5, 2.5, 3.5, 4.5 and 6 months,
respectively in the urban and; 57%, 16%, 9%, 6%, 5% and 0% at discharge,
1.5, 2.5, 3.5, 4.5 and 6 months, respectively in rural setting. Use of
formula feeding was very high (55%) among the urban mothers during
hospital stay. The factors associated with continuation of exclusive
breastfeeding were mothers’ knowledge regarding breastfeeding and
reinforcement by health professionals, whereas the factors associated
with cessation were perceived insufficiency of milk, and cultural
practices.
Key words: Breastfeeding, India, Infant feeding, Rural, Urban.
|
|
A
s a global public health
recommendation, exclusive breastfeeding (EBF) should be practiced for the
first six months of life, to achieve optimum growth, development and
health(1). In India, breastfeeding is almost universal, but the EBF rate
is quite low. Third National Family Health Survey (NFHS III) from India
reports EBF rates of 46.3% at 5 months(2). Government has launched several
measures for strengthening exclusive breastfeeding at National level
including baby friendly hospital initiative (BFHI). Hospitals are
certified baby friendly after rigorous assessment but are not monitored
later(3). Most studies assessing breastfeeding practices in India are
cross-sectional in nature. The present study employed a longitudinal
design to study the pre-valence of EBF and to identify the factors
associated with continuation/discontinuation of EBF among urban and rural
mothers.
Methods
This descriptive longitudinal study was conducted in a
teriary hospital in New Delhi (urban setting) and a First Referral Unit (FRU)
in Ballabgarh, Haryana (rural setting). Cohort of mothers delivering in
each setting during one month study period, who were willing to
participate, stayed nearby to the study site and who could understand
English or Hindi were enrolled. Mothers having babies with birthweight
<1500 grams, gestational age <34 weeks, admitted in intensive care unit
for >48 hours or having contraindications for breastfeeding were excluded.
A sample of 97 mothers from each setting was calculated to be adequate to
estimate the prevalence at 0.10 level of significance based on reported
EBF rates of 0.55 in NFHS II(4).
Semi structured interview schedules (three) were
developed and validated by five experts. Ethical clearance was
obtained from ethics committee of AIIMS, New Delhi. After obtaining
informed written consent, first two interviews were conducted on the
day of delivery and discharge, respectively. Subsequent interviews were
conducted at 1.5, 2.5, 3.5, 4.5 and 6 months. Data analysis was done using
SPSS 10.0 package.
Results
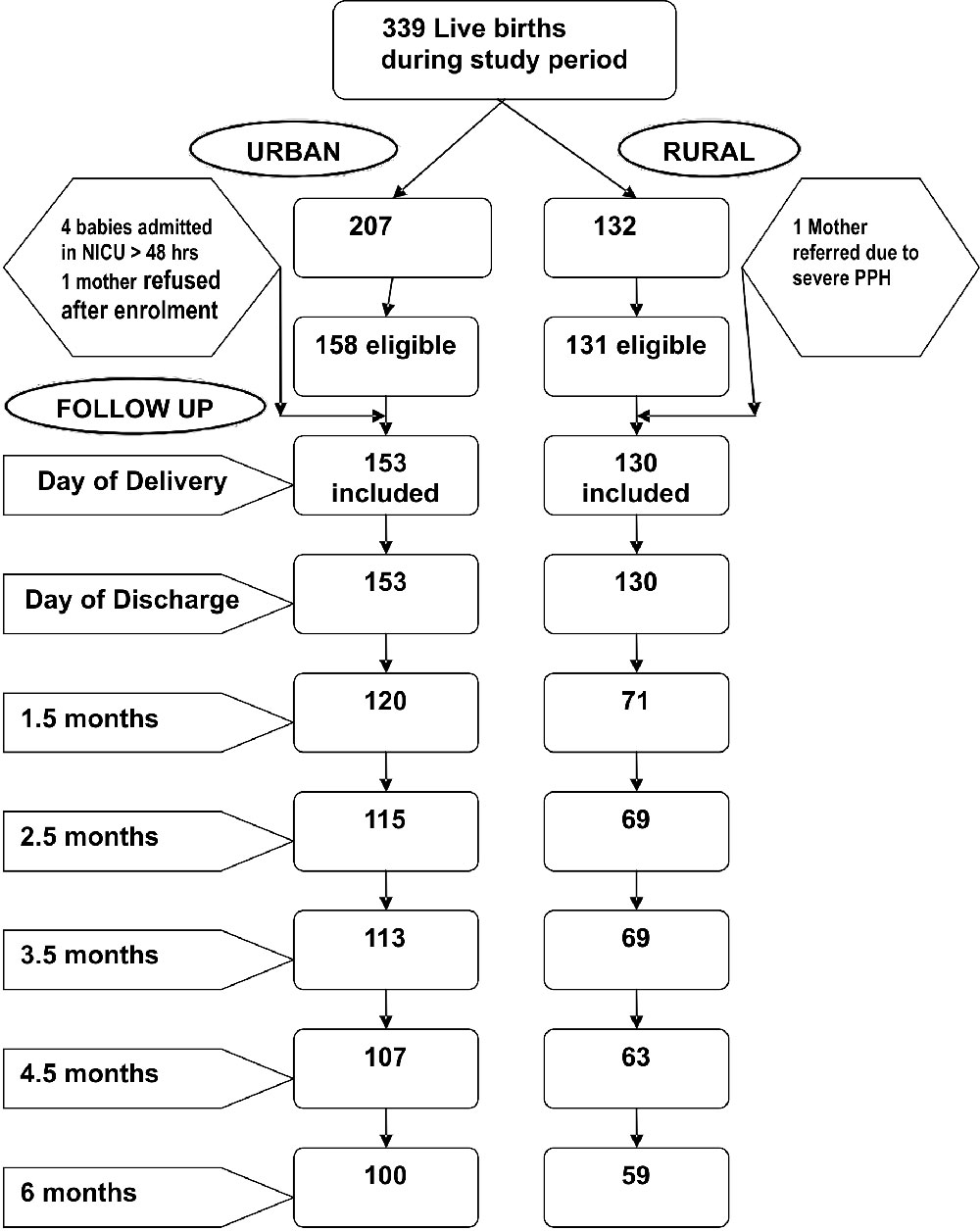
153 urban and 130 rural mothers were included in the
study (Fig. 1). The sample was heterogeneous with
respect to age of the mother, educational and occupational status of
parents, and birth order of baby in both settings. Majority (72% urban;
80% rural) of mothers belonged to joint families and were multiparous
[urban 72%; rural 69%). 40% of mothers in urban setting had cesarian
deliveries whereas 94% of rural births were normal deliveries.
 |
|
Fig. 1 Sample Description.
|
Only 21 % urban and 35% rural mothers initiated
breastfeeding within one hour of birth. EBF at discharge was low (urban
38%; rural 57%). Formula milk was fed by 55% urban mothers during hospital
stay. Mothers in the rural setting fed honey, tea and water (10-16%).
Perception of breastmilk being best for the newborn baby promoted EBF in
74% urban and 36% rural mothers. Doctors’ advice for EBF motivated 21%
urban and 23% rural mothers during hospital stay.
 |
|
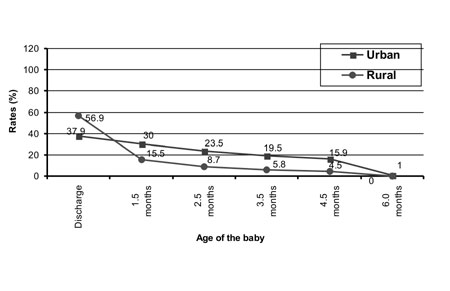
Fig.2 Trend in EBF rates from birth to six
months. |
Feeding pattern after discharge till six months of life
is described in Table I. EBF rates were abysmally low
in both settings (Fig. 2) and there was a consistent fall
reaching almost zero by six months of age. After discharge, awareness
about need for EBF encouraged 51 -100% urban mothers who breastfed babies
exclusively, while doctors’ reinforcement promoted EBF in rural mothers
(46.1-75 %).
TABLE I Pattern of Non-Exclusive Breastfeeding by Mothers
|
Feed in addition |
1.5 months |
2.5 months |
3.5 months |
4.5 months |
6.0 months |
|
to breastmilk |
Urban |
Rural |
Urban |
Rural |
Urban |
Rural |
Urban |
Rural |
Urban |
Rural |
| |
n=32 |
n=60 |
n=47 |
n=63 |
n=54 |
n=65 |
n=71 |
n=60 |
n=99 |
n=59 |
| |
(%) |
(%) |
(%) |
(%) |
(%) |
f(%) |
(%) |
(%) |
(%) |
(%) |
| Water |
11 (34.4) |
42 (70) |
17 (36.2) |
45 (71.4) |
22 (40.7) |
46 (70.8) |
25 (35.2) |
40 (66.7) |
17 (17.2) |
28 (47.5) |
| Animal milk |
11 (34.4) |
7 (11.7) |
17 (36.2) |
10 (15.9) |
22 (40.7) |
9 (13.8) |
41 (57.7) |
12 (20) |
51 (51.5) |
30 (50.8) |
| Formula milk |
11 (34.4) |
0 |
16 (34) |
0 |
16 (29.6) |
1 (1.5) |
10 (14.1) |
2 (3.3) |
1 (1) |
0 |
|
Commercial |
0 |
0 |
0 |
0 |
1 (1.9) |
0 |
4 (5.6) |
2 (3.3) |
43 (43.4) |
6 (10.2) |
| top feeds |
|
|
|
|
|
|
|
|
|
|
|
Home made |
0 |
0 |
0 |
0 |
4 (7.4) |
1 (1.5) |
8 (11.3) |
2 (3.3) |
80 (80.8) |
22 (37.3) |
|
supplements |
|
|
|
|
|
|
|
|
|
|
| Ghutti |
1 (3.1) |
35 (58.3) |
0 |
40 (63.5) |
1 (1.9) |
40 (61.5) |
4 (5.6) |
33 (55) |
2 (2) |
18 (30.5) |
|
Others (gripe |
1 (3.1) |
1(1.7) |
1 (2.1) |
1 (1.6) |
1 (1.9) |
1 (1.5) |
1 (1.4) |
1 (1.7) |
1 (1) |
1 (1.7) |
|
water, tea) |
|
|
|
|
|
|
|
|
|
|
Non-exclusive breastfeeding was practiced by 52% of
urban and 50% rural mothers during hospital stay due to perceived
insufficiency of milk. Cultural practice influenced 45% rural mothers.
Perceived insufficiency of milk (36%-47%) in the first 3.5 months and
baby not satisfied after feeds (37-62%) in children aged between 3.5
months to 6 months were again the most common reasons for non exclusive
breastfeeding in urban mothers. Rural mothers explained that they fed
water (17%-31%) to prevent drying of lips in summers and ghutti
(18%-44%) to promote digestion, which explains cultural influence.
Discussion
The practices related to breastfeeding in the present
study were found to be faulty in the majority of mothers in either urban
or rural setting. Only 21% urban and 35% rural mothers initiated
breastfeeding within 1 hour of birth despite being in hospital. Two
previous studies from North India(5,6) have reported a higher proportion
of mothers initiating early breastfeeding. This may be related to the
recall bias in these studies owing to cross-sectional nature of their
design. EBF rates were also generally low. Lesser EBF rate in the urban
setting was also contributed by a large number of caesarean sections. The
high rates of formula feeding in the urban setting (55%) indicate that
formula was easily available to the mothers. There was failure to initiate
EBF in urban setting whereas there was a failure to continue EBF after
discharge in rural setting (Fig.1). The median age at which
EBF was discontinued was the first day in urban and eleventh day in rural
setting, probably because large number of mothers fed formula on the first
day in urban and started water or ghutti soon after discharge in rural
setting. The EBF rates in our study at various time periods were much
lower than the national figure of 55% given by NFHS II(4).
Reinforcement by health professionals promoted
breastfeeding. Perceived insufficiency of milk was the major reason cited
by mothers for non exclusive breastfeeding after discharge which is
consistent with findings of studies conducted in Delhi(6) and Rajastan(7).
Cultural influences explained are similar to previous studies from North
India(6-8).
A major limitation of our study was large number of
drop outs especially in rural setting because of migration of subjects
from original homes. This migratory population might have some different
characteristics related to breastfeeding practices. In the absence of
sound data about infant feeding practices of such migratory population,
the direction in which the results could have been influenced by the
attrition can not be reliably predicted.
Many of the factors responsible for discontinuation of
EBF as found in our study are easily amenable to intervention.
Strengthening of infant feeding counseling services provided to the
mothers at all levels and frequent evaluation and reinforcement for
breastfeeding in baby friendly hospitals may help to improve the status of
breastfeeding in the country.
Contributors: AM collected data, and analysed and
interpreted it. All authors contributed to concept design, revision of
article and final approval.
Funding: None.
Competing interest: None stated.
|
What This Study Adds?
•
Exclusive breastfeeding rates are low and fall progressively
during first six months, even among the mothers delivered in
baby-friendly hospitals.
|
References
1. National Guidelines on Infant and Young Child
Feeding. 2004. Available at: http://www.wcd.nic.in/national guidelines.pdf.
Accessed November 24, 2007.
2. Ministry of Health and Family Welfare. National
Family Health Survey (NFHS-3) National fact sheet India. Available at:
http://www.nfhsindia.org/pdf/IN.pdf. Accessed March 12, 2008.
3. Phatak A, Gupta A. Recommended duration of exclusive
breastfeeding and age of introduction of complementary foods: A review.
Available at: http://bpni.org/egi/news.asp?id705&title= Advocacy+Document.
Accessed January 18, 2007.
4. Dadhich JP, Paul V, editors. State of India’s
Newborns. New Delhi: National Neonatology Forum; 2004. p. 102-104.
5. Taneja DK, Saha R, Dabas P, Gautam VP, Tripathy Y,
Mehra M. Study of infant feeding practices and underlying factors in a
rural area of Delhi. Indian J Community Med 2003; 28: 107-111.
6. Rasania SK, Singh SK, Pathi S, Bhalla S, Sachdev TR.
Breastfeeding practices in maternal and child health centre in Delhi.
Health Popul Perspect Issues 2003; 26: 110-115.
7. Paliwal S, Khanna A. Infant feeding practices in a
rural community. Indian J Prev Soc Med 2001; 32: 104-112.
8. Kumar D, Agarwal N, Swami HM. Socio-demographic
correlates of breastfeeding in urban slums of Chandigarh. Indian J Med Sci
2006; 60: 461-466.
|
|
|
 |
|

