|
clinicopathological conference |
|
|
Indian Pediatr 2009;46: 867-873 |
 |
A Patient with Rashes and Limb Weakness |
|
S Sawhney*, M Agarwal*, S Roy **, S Buxi , S Sud ***, and S Singh
#
From the *Pediatric Rheumatology Unit, Centre for Child
Health, **Department of Histopathology, ***Department of Radiodiagnosis,
North MRI Scan and Research Centre, Sir Ganga Ram Hospital, New Delhi,
India, and #Department of Immunology, APCCC, PGI, Chandigarh, India.
Correspondence to: Dr Sujata Sawhney, Pediatric
Rheumatologist, B 602, Som Vihar, New Delhi 110022, India.
Email:
drsujatasawhney@gmail.com
|
|
Patient Summary
An 8-yr-old girl presented in July 2007 with a history
of skin rashes during the last six months, pain and weakness of the left
leg three months ago, one episode of loss of consciousness in the last
three months and severe limb pains and worsening of the rashes over the
last month (Fig.1). The rash was erythematous, blanched on
pressure, was not itchy and was predominantly seen on the hands and feet.
There was no history of associated fever, weight loss, joint pains, oral
ulcers, hair loss, respiratory or gastrointestinal complaints. There was
no aggravating or relieving factor. No specific diagnosis was reached and
the child was treated with anti-histaminics. Until March 2007, the child
had a spontaneous increase or decrease in the rashes with no associated
complaints. At this time while playing she tripped, following which she
could not bear weight on the left leg and was numb below the knee.
Investigations included a hemoglobin level of 13 g/dL, leukocyte count of
10300/cu mm, platelets 248000/cu mm and an ESR of 30 mm at 1 hr. The CRP
was negative, and transaminases and creatinine levels were normal. The
creatine kinase was elevated to 3982 I.U/L (normal <140). The urine showed
a 2+ proteinuria and 10 erythrocytes per high power field, urine culture
grew E. coli 10000/mL. The rheumatoid factor, antineutrophilic
cytoplasmic antibody (ANCA) and the antinuclear antibody (ANA) were
negative. An MRI of the spine showed patchy signal alteration in the left
gluteus, adductor group, rectus femoris and vastus lateralis muscles,
compatible with that associated with history of trauma. The kidneys were
swollen with altered signal intensity (Fig. 2).Nerve
conduction studies showed motor changes in the common peroneal, posterior
tibial and sural nerve suggestive of a sciatic nerve injury. The child was
treated with oral prednisolone for two weeks followed by tapering over
next four weeks, during which she showed satisfactory improvement and
resumed normal activities.
 |
 |
|
Fig. 1 Erythematous rash on
palms. |
Fig. 2 T2 weighted axial image showing
a large area of hyperintensity in the rectus femoris muscle on the
right side suggestive of inflammation. |
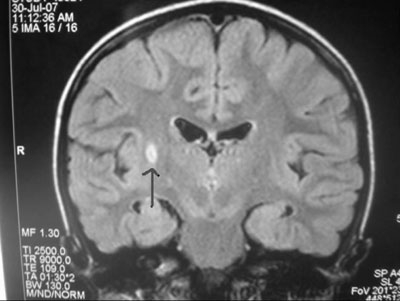
In May 2007, while playing she collapsed, accompanied
by momentary loss of consciousness. A MRI of the brain showed multiple
tiny foci of altered signal in the brain parenchyma in the right
cerebellar hemisphere, pons, thalamus and left basal ganglia, suggestive
of a "demyelinating process or vasculitis" (Fig.3a
and 3b).
 |
 |
|
Fig. 3a TIRM coronal image of
the brain showing a focal hyperintense lesion on the right
periventricular region suggestive of a lacunar infarct. |
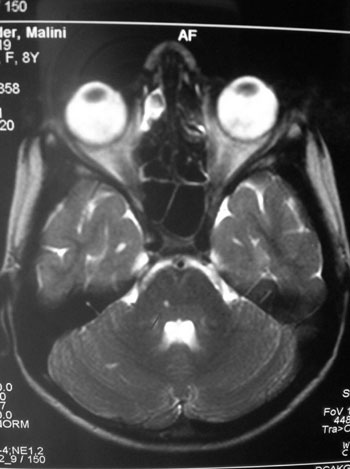
Fig. 3b T2W axial brain MRI
showing focal hyper intensity in the right side of the pons
suggestive of a lacunar infarct. |
Over the next two months the child had an episodic
increase in the rashes and limb pains. On examination at this hospital in
July 2007, she had a blanching erythematous rash on the palms. The
peripheral pulses and four limb blood pressures were normal.
Investigations showed a hemoglobin level of 11.9g/dL, leukocyte count
9500/mm 3, platelet count 233000/mm3
and an ESR of 20 mm at 1 hr. CRP was negative and urinalysis, liver
function tests, creatinine and CPK were normal. The chest X-ray and
thyroid function test were normal. The ANA, antiphospholipid antibodies,
double stranded DNA and ANCA were negative, and complement levels were
normal. A screen for infection with hepatitis B and C, and HIV was
negative. Ultrasonography of the abdomen showed a scar on the superior
pole of the right kidney. Nerve conduction velocity showed a delayed
latency and decreased amplitude and con-duction velocity in left sural
nerve and only decreased amplitude in the left median nerve. The nerve
conduction study was abnormal with left median motor axonal involvement
and left sural sensory involvement with chronic neurogenic changes.
A diagnostic procedure was performed.
Discussion
Dr. Surjit Singh: Clinical Discussant
Physical examination of the 8 yr old girl showed normal
vital signs and four limb blood pressures. She had an erythematous palmar
rash but the systemic examination was unremarkable. The reticulated rash
was not classical of any particular disease but may be a manifestation of
systemic vasculitis, anti-phospholipid antibody syndrome or autonomic dysfunction.
If persistent, such a rash should not be ignored. During evaluation, she
had severe pain in the left leg and was noted to have abnormal nerve
conduction study with left median motor axonal involvement and left sural
sensory involvement with chronic neurogenic changes.
The patient appeared to have an episodic illness which
was steroid responsive. In addition she also had a rash for many months,
significant limb pain and muscle disease with pain and tenderness.
Laboratory evaluation revealed a significantly elevated CPK level and MRI
of the thigh muscles showed altered signal intensity in the anterior and
lateral compartments of the thigh, which was definitely abnormal, although
interpreted as posttraumatic. She also had both a central nervous system
involvement in the form of loss of consciousness and abnormal MRI
findings, and a peripheral neuropathy, confirmed by the nerve conduction
study. In addition she had renal involvement with albuminuria and
microscopic hematuria and a renal scar suggestive of infarction. There was
no definite evidence of urinary tract infection.
Of note was a normal platelet count. The platelet count
is of great interest in rheumatology because in most rheumatologic
disorders with inflammation, thrombocytosis is commonly seen. A normal
count suggests that there was no active inflammation at that time. ESR was
borderline elevated and a detailed immunological panel was negative.
The following conditions should be considered in a
patient with multisystem involvement: (1) infective endocarditis (2)
systemic lupus erythematous (SLE) and (3) vasculitic syndromes.
Infective endocarditis. There is no setting for the
patient to develop infective endocarditis but if this child had normal
valve endocarditis, I cannot exclude it based on the data available.
SLE: From the physical findings, there is nothing
to suggest SLE. Moreover, on two different occasions, both the antinuclear
antibodies and the anti-double-stranded antibodies were negative. If ANA
has been done by immunofluoresence and remained negative over a period of
six months, I can with a fair amount of confidence rule out SLE.
Thus, I would like to rule out both these conditions,
based on the data that has been provided.
Systemic vasculitis syndromes: These conditions can
explain the multisystem involvement in this patient.
The common vasculitis disorders seen in children are
classified into large vessel, medium vessel, and small vessel based on the
vessel size(1,2). We shall discuss them one by one.
This is not the presentation of Takayasu disease since
four limb pulses and blood pressure were normal. Temporal arteritis does
not occur in children. Kawasaki disease: This diagnosis was excluded based
on the clinical history and findings. Similarly there was no evidence of
Henoch Schnolein Purpura, Wegener’s granulomatosus, hypersensitivity
angitis, urticarial vasculitis, and cryoglobulinemia related vasculitis.
Microscopic polyangitis and polyarteritis nodosa (PAN)
are similar conditions that are included in the category of medium vessel
vasculitis. PAN, first described by Kussmaul and Maier, was initially
called periarteritis nodosa and described as a chronic, relapsing, febrile
disease with protean manifestations resulting from inflammation of the
small and medium-sized muscular arteries often leading to aneurysm
formation. The hallmarks of the condition include.
(i) Non-specific signs and symptoms:
Constitutional symptoms of fever and myalgias are frequent. PAN is one
of the most difficult clinical diagnoses to make in children, and has a
variable clinical course as can be expected from a disorder with diffuse
vasculitis.
(ii) The clinical presentation depends on the
system involved. The organ system involvement is episodic and
unpredictable, just as in this patient. The childhood form of the
disease is different from that described in adults. Ozen et al have
described major and minor criteria for diagnosing childhood PAN. These
criteria are guidelines for diagnosis of the disease based on experience
at that center on 31 patients over 28 years. The major criteria pertain
to renal and musculoskeletal involvement. Minor criteria, focus on
cutaneous findings, peripheral neuropathy, hypertension, lung disease,
increased acute phase reactants, gastrointestinal involvement,
neurological and cardiac disease, constitutional symptoms, and presence
of hepatitis B surface antigen(3).
A patient is said to have PAN if there are three
criteria, including at least one major criterion. It is emphasized that
these criteria have not been validated. The index case had the following
features: renal disease, significant musculoskeletal involvement,
cutaneous findings, peripheral neuropathy and neurological disease.
However, she did not have constitutional symptoms, or hypertension which
is seen in many patients with PAN. But a normal blood pressure in this
patient can be explained as the variant of microscopic polyangiitis which
does not have hypertension. The present patient definitely fulfills Ozen’s
criteria for PAN.
An important concern regarding the diagnosis of PAN in
this patient includes the absence of fever. In our series on PAN, all the
patients had fever. Most patients also show significant hypertension. More
than 90% of our patients were hypertensive and most had elevated acute
phase reactants(4).In fact, it is the hypertension which often points to
the disease in addition to elevated acute phase reactants. It is therefore
difficult to explain these findings in the context of a diagnosis of PAN.
There is a subset of patients with polyarteritis that have mononeuritis
multiplex. These children may have little or no systemic features. So, in
our patient since there was a very prominent component of mononeuritis
multiplex, even if this child did not have fever and hypertension, it
could still be PAN.
Thus the chief clinical, laboratory and imaging
findings are consistent with the diagnosis of PAN. This is a disorder that
is known to be both episodic and steroid responsive as was the case in
this patient. The skin rash though not typical of PAN is significant. Limb
pain can be a very prominent finding in children because of neuropathy and
muscle ischemia. Muscle disease can be explained as well. Increased CPK
level, though not a very prominent feature can occur in PAN. The patient
had classical mononeuritis multiplex. The neurological disease,
loss of consciousness and MRI findings were all compatible with the
diagnosis of PAN. The renal involvement, albuminuria, microscopic
hematuria, are all present in patients with the microscopic polyangiitis,
a variant of PAN.
There are two aspects of the case which are not well
explained. These include the history of urinary infection and the renal
scar. In the literature, there are case reports of abnormal intravenous
pyelograms in patients with PAN. Here, the passage of the urine through
the ureter is affected because the vascular supply to the ureter is
compromised. Thus, infection could be a result of ureteral dysfunction and
scars have been described in patients with PAN and ureteric dysfunction.
However, if this patient had an otherwise unrelated urinary tract
infection, then repeated episodes of urinary tract infection can result in
scars as a result of reflux nephropathy(5,6). Thus, virtually all
the problems described can be related to the main diagnosis of PAN.
Based on the history and the physical findings, the
only differential diagnosis here is PAN. The diagnostic investigation
which was done in the child was probably an angiography to confirm the
diagnosis. The angiography would have shown micro aneurysms and may be
arterial narrowing beyond that. Another procedure that would have been
helpful was a muscle biopsy from the sites which were shown to be abnormal
on MRI. The muscle biopsy would have shown evidence of vasculitis. Thus,
muscle biopsy could also have been done but a more definitive
investigation would have been some form of the angiography, either an MR
angiography or a conventional angiography.
Similar clinical features may be seen in patients with
infection associated vasculitis. We have managed one such patient who was
admitted with the diagnosis of microscopic polyangiitis, had all the
typical features of microscopic polyangiitis including glomerular
nephritis and was found to have antibodies against parvovirus B19. This
child recovered on her own and remains well(7). Thus, parvovirus B19 may
have a very similar presentation and it can mimic all the features of
systemic vasculitis. We have also seen a patient with varicella
glomerulonephritis, an uncommon complication(8), while as a group,
infection- associated vasculitis(9) can be considered as a
differential diagnosis, the most likely diagnosis in this case is PAN.
Dr Arvind Taneja (Pediatrician) The urine infection
discussed may be a red herring because one urine culture showing
insignificant growth does not confirm the diagnosis of urinary infection.
Contamination due to improper collection is a possibility.
Dr Singh I agree, it would be important only if the
child had been on antibiotics.
Dr Sawhney This young child came to me after she
had a cerebral MRI which suggested vasculitis. On review of the history,
clinical examination and detailed investigations, two things were clear.
Firstly, she was episodically unwell and well enough between times to
attend school. Thus, this was not the clinical gestalt of a patient with
severe systemic vasculitis or frank connective tissue disease. It appeared
more like an embolic phenomenon. Secondly her inflammatory parameters were
not raised. This raised the question that the child had a "vasculitic
mimic". The diagnostic investigation that clinched the diagnosis was an
echocardiogram.
Dr Buxi (Radiologist) I will briefly discuss the
imaging. The MRI done showed multiple areas of cortical altered signal
intensity in the kidney. The gluteus maximus and the right rectus
femoris muscles have features suggestive of inflammation (Fig. 2).
In the brain, T2 weighted axial image revealed multiple small
hyperintense areas in the vicinity of the left caudate, left frontal
periventricular region and the left lenticular region. Small hyperintense
lesion was seen in the right basal ganglion as well. These findings are
suggestive of multiple infarcts (Figs. 3a and 3b).
The possibility of an embolic phenomenon affecting the skin, muscles,
kidney and brain should be considered.
Dr Mohanty (Cardiologist) On clinical examination
the cardiovascular system was normal. On echocardiogram the left atrium
was slightly enlarged and there was a solitary mass measuring 3 cm x 3 cm
attached to lateral wall of the left atrium. It was just prolapsing into
the left ventricular cavity during systole. There were no areas of
necrosis or haemorrhage and a clinical diagnosis of left atrial myxoma was
made (Fig. 4).
Dr Sujata Sawhney The cardiology team opined that
the myxoma was prolapsing into the left ventricle during systole. The
patient was at risk of obstructive cardiac failure and hence underwent
cardiac surgery within twelve hours of diagnosis.
Dr G Shivnani (Cardiac Surgeon) The patient was put
on a cardiopulmonary bypass and a large pedunclated mass 3 cm x 3 cm was
found attached to the lateral wall of the left atrium, just inferior to
right superior pulmonary vein. The mass was excised and the child had an
uneventful recovery.
Dr Subimal Roy (Pathology) The specimen consisted
of multiple polypoidal and mucoid grey pink pieces of tissue, measuring 4
× 3 × 2 cm. In one fragment a pedicle was identified which was 0.5 cm
long. Microscopic examination showed polypoid tissue covered with
flattened endothelial cells. The stroma showed marked myxoid change with
focal hemorrhages, many small capillaries and a diffuse inflammatory
infiltrate of lymphocytes, plasma cells and occasional polymorphs (Fig.
5).The findings were compatible with the diagnosis of atrial
myxoma.
Literature review
More than 50% of primary tumors in the heart are
cardiac myxomas. A review of 1029 patients showed that 83.0% of myxomas
were located in the left atrium and 12.7% in the right atrium(10).
About 15% patients may be asymptomatic for a long period of time. When
they are symptomatic, majority of patients with myxomas may experience
symptoms due to central or peripheral embolism or intracardiac
obstruction. Claudication is also well reported(11). If the tumor is in
the right heart chambers it may cause pulmonary emboli, a Budd-Chiari
syndrome and remittent or lasting fever. Weight loss, chronic anemia,
arthralgia, polycythemia and hyper-gammaglobinemia may occur in some
patients. These manifestations often disappear after resection of the
tumor(10).
Generally most of the cases of atrial myxoma are
sporadic (90%). A small numbers of cases are familial as in Carney
syndrome. The condition is characterised by a complex of spotty skin
pigmentation, myxomas, endocrine overactivity, and schwannomas. It is a
multiple endocrine neoplasia (MEN) and lentiginosis syndrome that is
inherited in an autosomal dominant manner and is genetically
heterogeneous(12). Although myxomas are most common in left atrium, they
can occur in the right side or even be multiple. The index patient is a
case of nonfamilial cardiac myxoma which is generally solitary.
Final diagnosis: Left atrial myxoma
Dr Sawhney There are 107 cases of atrial myxomas
reported till 2004, both in adults and children. The female-male ratio is
3:1. The mean age is 43 years and of note, more than 80% of the patients
were detected after a stroke and one-fourth of them are autopsy
reports(13). The first antemortem report of left atrial myxoma was in a
3-yr-old child who was diagnosed to have the myxoma when he presented with
recurrent hemiplegia. The same paper reviewed nine children, of these 8
had a stroke prior to diagnosis, 6 had erythematous rashes on the
extremities, 4 had normal cardiac examination and two had a
recurrence(14).
Dr Singh How are the skin rashes, lack of cardiac
findings and the neurological features explained?
Dr Sawhney On literature review of nine children,
vast majority had rashes. The reason for the transient cutaneous eruptions
involving the extremities was most likely attributable to fragmentation of
the atrial tumor with peripheral embolization. Several patients may have
no clinical symptoms or signs referable to the cardiovascular system(14).
Dr Manvir Bhatia (Neurophysiologist) The NCV done
at this centre showed that the left sural nerve was definitely delayed in
latency, had a decreased amplitude and conduction velocity. This was the
same leg where she had developed numbness. I think that possibly was a
vascular phenomenon which involved the sural nerve. Involvement of a
single sensory nerve does not fit the criteria for mononeuritis multiplex.
Study of the left median nerve revealed decreased amplitude only, with no
change in latency and conduction velocity. This is not suggestive of a
neuropathy involving the median nerve.
Dr Singh The response to steroids: how is this
explained?
Dr Sawhney I think this was incidental. The child
had episodic phenomenon of embolization and was well between the episodes.
The patient continues to be on regular follow up.
Multiple follow up echocardiograms are normal and she remains well. Since
a small percentage of patients may have a recurrence, patients need
careful follow up. The present case suggests that atrial myxoma should be
considered in the differential diagnosis when children present with
unexplained neurologic symptoms or with signs of embolization, because
surgical removal of the tumor is curative(14).
Funding: None.
Competing interests: None stated.
References
1. Ozen S, Ruperto N, Dillon MJ, Bagga A, Barron
K, Davin JC, et al. EULAR/Press endorsed consensus criteria for the
classification of childhood vasculitides. Ann Rheum Dis 2006; 65: 936-941.
2. Ozen S. The spectrum of vasculitis in children. Best
Pract Res Clin Rheumatol 2002; 16: 411-425.
3. Ozen S, Besbas N, Saatci U, Bakkaloglu A. Diagnostic
criteria for polyarteritis nodosa in childhood. J Pediatr 1992; 120:
206-209.
4. Kumar L, Sarkar B, Singh S, Bajwa RP, Joshi K, Malik
N. Polyarteritis nodosa—a few unusual findings. Indian Pediatr 1996; 33:
459-464.
5. Kaskarelis IS, Zarifi M, Dantis P, Vrachliotis G.
Bilateral ureteral involvement in polyarteritis nodosa. Scand J Urol
Nephrol 1995; 29: 323-326.
6. Melin JP, Lemaire P, Birembaut P, Aubert L, Cohen J,
Lardennois B, et al. Polyarteritis nodosa with bilateral ureteric
involvement. Nephron 1982; 32: 87-89.
7. Dass R, Ramesh P, Ratho RK, Saxena AK, Singh S.
Parvovirus B19-induced multisystem disease simulating systemic vasculitis
in a young child. Rheumatol Int 2005; 25: 125-129.
8. Dass R, Singh S, Kumar V, Vaiphei K, Agrawal S,
Saeed T, et al. Varicella glomerulonephritis mimicking microscopic
polyangiitis. Rheumatol Int 2004; 24: 362-364.
9. Pagnoux C, Cohen P, Guillevin L. Pagnoux C, Cohen P,
Guillevin L. Vasculitides secondary to infections. Clin Exp Rheumatol
2006; 24: S71-81.
10. Kuon E, Kreplin M, Weiss W, Dahm JB. The challenge
presented by right atrial myxoma. Herz 2004; 29: 702-709.
11. Gavrielatos G, Letsas KP, Pappas LK, Dedeilias P,
Sioras E, Kardaras F. Large left atrial myxoma presented as fever of
unknown origin: a challenging diagnosis and a review of the literature.
Cardiovasc Pathol 2007; 16: 365-367.
12. Malchoff CD. Editorial: Carney complex—clarity and
complexity. J Clin Endocrinol Metab 2000; 85: 4359-4366.
13. Ekinci EI, Donnan GA. Neurological manifestations
of cardiac myxoma: a review of the literature and report of cases. Intern
Med J 2004; 243-249.
14. Al-Mateen M, Hood M, Trippel D, Insalaco SJ, Otto
RK, Vitikainen KJ. Cerebral embolism from atrial myxoma in pediatric
patients. Pediatrics 2003; 112: 162-167.
|
|
|
 |
|

