Neonatal lupus erythematosus (NLE) is a rare form of
lupus erythematosus first described in 1954(1). It is characterized by
the presence of cutaneous lesions or congenital heart block or both, in
an infant whose mother has connective tissue disease or auto antibodies
to extractable nuclear antigens Anti-Ro (SSA), Anti-La (SSB) or
ribonucleoproteins (RNP)(2).
Case Report
A 45-days-old male delivered to a 22-year-old,
primigravida by caesarean section at 35 weeks of gestation due to fetal
bradycardia. There was no history of fever, rash, lymphadenopathy or
drug intake during pregnancy. The natal and postnatal periods were
uneventful. At presentation the infant weighed 3.8 kg, with length of
51.5 cm and head circumference 34.2 cm. The heart rate was 76/min,
regular and had no pulse deficit. All peripheral pulses were palpable.
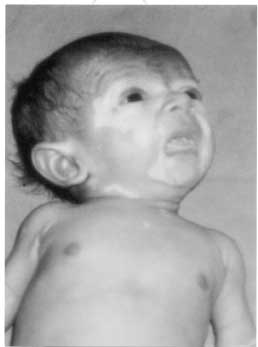
There were areas of depigmentation (with no erythema or scaling) over
the nose, cheeks, around the eyes, scapular region and lower back. There
was no significant lymph-adenopathy, bleeding spots, rash or
hepato-splenomegaly. Laboratory investigations showed Hg of 12g% (PCV
was 40%). Total Leukocyte Count was 6800/mm3, differential leukocyte
count was P60, L40, E0, M0 and platelet count of 22,000/mm3. Liver
function tests were within normal limits. Anti-nuclear antibody (ANA) by
immunoflorescence was strongly positive (1:640), Anti Ro and Anti La
were negative. Electrocardiogram of the baby revealed type 3 congenital
heart block The echocardiography showed a structurally normal heart.
Skin biopsy revealed scattered lymphocytic infiltration in the dermis
with few lymphocytes seen clustered around dermal appendages features
compatible with NLE. Immunoflorescence studies could not be done. ANA
was positive at 1:640 with speckled pattern in motherís serum. Anti-Ro
was present but there were no detectable Anti-La or Smith (Sm)
antibodies.
Discussion
Neonatal lupus erythematosus (NLE) is characterized
by the presence of cutaneous lesions, congenital heart block or both in
about 10% cases(3). The reasons why some babies develop skin disease,
while others develop heart disease are not clearly known. The incidence
of NLE is not known. Although genetically determined autoantibody
production occurs in the mother, tissue injury may depend on other
factors which are not very clear at present(3). More than 90% infants
will have cutaneous lesions, of which 70% are present at birth and the
remainder usually develops within 2 months. These lesions are usually
transient and last for a few weeks to months(2). Cutaneous lesions
characteristically are erythematosus papules, annular discoid or
polycyclic plaques with or without fine scaling. NLE lesions are
frequently found on the scalp and face, however, unusual presentation
with congenital skin atrophy, erosions and alopecia have also been
rarely described. On occasion lesions are concentrated in the
periorbital or malar region(3,4). The skin biopsy in lupus erythematosus
may reveal epidermal atrophy, liquefaction, degeneration of basal
keratinocytes, colloid bodies and a perivascular and periappendageal
lymphohistocytic infiltrate in the dermis(5).
 |
|
Fig. 1. Photograph showing depigmented
macular patches on the face. |
Amongst the cardiac abnormalities about 50% are
conduction defects. In mid to late fetal development anti-Ro antibodies
can bind to cardiac conducting cells, alter membrane repolarization and
selectively damage AV node(6). Heart block can be detected as early as
16 week of gestation by USG or fetal electrocardiography(3). Other
cardiac problems include subendocardial fibro-elastosis, fibrinous
pericarditis, PDA(6). Other systemic manifestations include hemo-lytic
anemia, thrombocytopenia, liver, lung and CNS involvement(3,6).
Maternal auto antibodies directed against tissue
antigens of skin, heart, liver, bowel, lung and blood cells are present
in infants with NLE. The IgG class are most frequent (95%) and are
directed against the Ro ribonucleo-proteins antigen(6).
Antenatal therapy is generally not required. Serial
plasmapheresis and systemic steroids have been tried with variable
success(3). Systemic steroids may occasionally be required for
associated thrombocytopenia or hemolytic anemia. Treatment of heart
disease is not always necessary. For children with heart failure due to
slow heart rate, pacemaker implantation is the treatment of choice. If
heart failure persists even after pacemaker implantation and children
who have serious internal systemic manifestations, may be treated with
systemic steroid(2,3). As many as 8.3% cases of NLE may progress to
systemic lupus erythematosus (SLE) in later childhood(6).
Acknowledgement
We thank Dr. Sharmila Mishra, Depart-ment of
Pathology, ICMR, Delhi for reviewing the skin biopsy.
Contributors: NA, PP worked up the case, reviewed
the literature and drafted the article. RM planned the management; PP
will act as the guarantor.
Funding: None
