Hepatic abscess with onset in neonatal period is a
serious disorder, which has been reported rarely. The diagnosis of
neonatal hepatic abscess is difficult and requires high index of
suspicion(1). To the best of our knowledge portal vein thrombophlebitis
and portal cavernoma formation in a neonate is a hither to unreported
complication of neonatal hepatic abscess. We present a neonate with
hepatic abscess who developed portal vein thrombosis and portal
cavernoma during medical therapy.
Case Report
A 28-day-old female neonate was admitted to the
referral neonatal unit of our hospital with complaints of high-grade
fever for 7 days and progressively increasing abdominal distension,
lethargy and decreased feeding for 2 days. Baby was delivered by lower
segment cesarean section to a 27-year-old mother in a nursing home.
Antenatal and perinatal periods were uneventful. Clinical examination at
admission showed fever (39ēC), irritability, pallor, tachypnea, and
tachycardia. Abdomen was distended and tense. Liver was firm and
palpable 8 cm below costal margin in right mid clavicular line with a
span of 10 cm. Spleen was palpable 2 cm below the costal margin, along
splenic axis.
On investigations, sepsis screen was positive with
20% bandemia and 18 mm microESR at one hour. Liver function tests were
within normal limits. Ultrasonography showed hepatomegaly with a
heteroechoic mass, 5 cm × 4 cm × 3 cm, with focal hyper echoic areas, in
the right lobe of liver. The lesion was mostly cystic in appearance.
Other abdominal organs were normal.
Possibilities of infantile hemangioen-dothelioma,
hepatoblastoma and liver abscess were entertained. Contrast enhanced
computed tomography of upper abdomen revealed hepatomegaly with multiple
well defined, multi septated hypodense lesion of varying sizes in both
lobes of liver, the largest measuring 4.2 cm × 3.4 cm in the right lobe
(Fig 1). After administration of intravenous contrast, presence
of enhancement was noted in the walls and internal septations of the
lesions. Diagnosis of liver abscess was made and ultrasound guided
tapping of the abscess was done, which revealed thick pus.2 ml pus was
withdrawn which grew Staphylococcus aureus sensitive to
vancomycin and cefotaxime. Blood culture also revealed the same
organism. The infant was treated with vancomycin and cefotaxime for 6
weeks. Fever gradually reduced over 3 weeks and the infant became
afebrile by 25th day of treatment. Repeated ultrasound examination, at
weekly interval revealed gradual reduction in abscess size. On day 40 of
treatment ultrasound examination revealed no definite abscess remaining
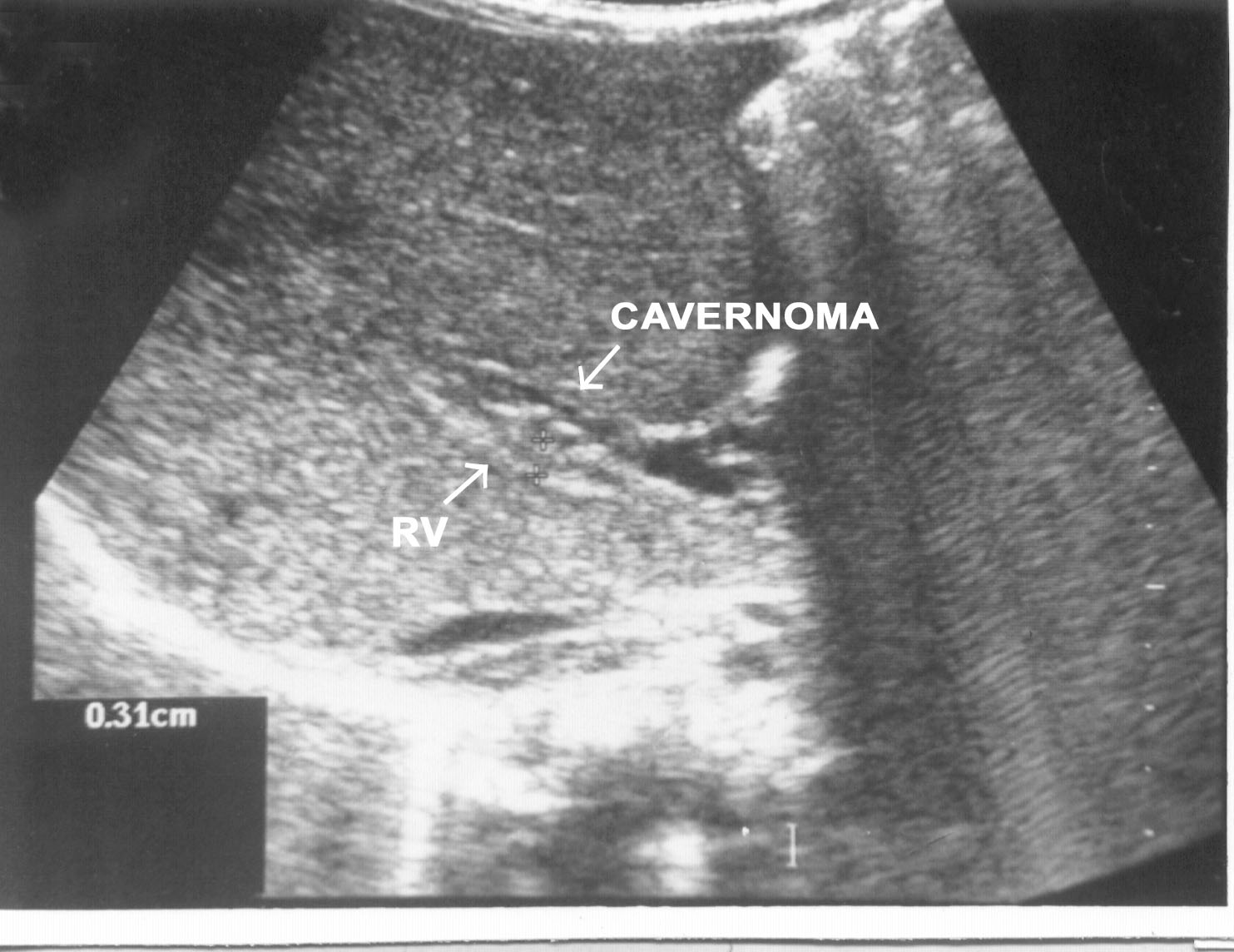
with few small, scattered calcific foci in hepatic parenchyma. Portal
vein, which was normal in previous ultrasounds, was thrombosed and
portal cavernoma was seen around it (Fig 2). Spleen and splenic
vein were normal at that time. The child was discharged after completion
of antibiotic therapy and regular follow up was emphasized.
 |
|
Fig. 1. CT Scan of liver showing multiple,
multisepatate, hypodense abscesses with contrast enhanced walls
and septae. |
 |
|
Fig. 2. Sonogram of upper abdomen showing a
thrombosed echogenic portal vein (PV) with multiple thin tortuous
vascular channels lying anterior to it suggestive of portal
cavernoma. |
Discussion
Hepatic abscess in neonatal period is a rare but a
serious disorder. It is usually noted as an incidental finding in
infants dying of sepsis(2). Most of the hepatic abscesses in neonates
are multiple. The diagnosis of neonatal hepatic abscess is extremely
difficult, especially when associated with serious problems(3).
Previously reported patients have manifested with acute fulminant course
and generalized sepsis(1). Possible risk factors include umbili-cal
venous cannulation, sepsis, abdominal surgery and necrotizing entero-colitis.
Bacteremia either concurrent or preceding the diagnosis of hepatic
abscess is noted in half of the cases. Bacteria isolated from neonatal
hepatic abscesses include Staphylococcus spp., Streptococcus spp.,
gram-negative bacilli and Hemophillus parainfluenzae(4). Amebic
liver abscess is extremely uncommon in neonates. There have been stray
case reports of amebic liver abscess in literature(5). Amebic liver
abscess presents with high grade fever and tender hepatomegaly, and
diagnosis is established by elevated indirect hemag-glutination titers
and ultrasonography of liver. In our case Staphylococcus aureus
was isolated from both blood and liver abscess.
Fever, abdominal distension, hepato-megaly, abnormal
gas pattern in right upper quadrant, elevation and limitation of the
motion of the right diaphragm and right sided pleural effusion are some
of the described manifestations(6). Our patient had fever, abdominal
distension and hepatomegaly. Diagnosis of hepatic abscess would seem to
rest mainly on high index of suspicion in any septic appearing infant.
Liver function studies, as in our case, are not helpful in making the
diagnosis(3). CT scan and ultrasound of the liver are the most sensitive
diagnostic tests in the detection of hepatic abscess(6). On ultra-sound
abscesses appear as poorly defined, hypoechoic lesions with
inhomogeneous heteroechoic areas. Although ultrasound is noninvasive and
easily available procedure but is less sensitive in detecting small
multiple abscesses(7). Findings on ultrasound are not diagnostic for
hepatic abscess as similar findings are seen in cases of hepatoblastoma,
infantile hemangioendothelioma and mesen-chymal hemartoma, if solitary
and in cases of secondaries of neuroblastoma, if multiple lesions are
seen. Same difficulty was observed in diagnosing liver abscess in our
case on ultrasound. When ultrasound is not helpful then CT scan may help
in confirming the diagnosis(7). The characteristic CT appear-ance is
that of a well-circumscribed low attenuation mass with a
contrast-enhancing rim. Multiloculation is a useful sign when present,
as in our case.
Treatment of hepatic abscess would include diagnostic
or therapeutic drainage of abscess by needle aspiration and intravenous
antibiotic therapy for 4-6 weeks. We did diagnostic aspiration of pus
from the largest abscess cavity and treated the child conser-vatively on
intravenous antibiotics for 6 weeks.
Portal vein thrombosis and portal cavernoma formation
in a neonate is, hitherto unreported complication of neonatal hepatic
abscess in English literature. Only a single report of two cases of
hepatic abscesses developing portal vein thrombosis during treatment is
available in French literature(8). A neonate developing portal vein
thrombosis following an exchange transfusion has also been reported(9).
Various causes of pediatric portal vein thrombosis have been listed in
literature but in neonates umbilical vein catheterization and sepsis are
the commonest causes implicated. However, in a prospective study to
detect thrombosis of the portal venous system after umbilical vein
catheterization and sepsis in 47 children no such complication was
observed(10).
Obstruction of portal vein leads to development of
collateral channels around it, which tend to maintain the hepatopetal
flow but progressively lead to development of portal hypertension by 3-5
years of age. These collateral channels are seen as cavernous
transformation of portal vein on Doppler ultrasound. Most of the cases
of portal vein thrombosis are insidious and asymptomatic in onset with
diagnosis possible only at later stages when features of portal
hypertension are evident clinically. Since onset is insidious with late
recognition hence no role of thrombolytic or antithrombotic therapy in
treatment of portal vein thrombosis. Only a single case report of
successful therapy of neonatal portal vein thrombosis within 16 hours of
onset by giving regional streptokinase infusion is described through an
umbilical vein catheter, which was left in situ following an exchange
transfusion(9). This modality of treatment may not be feasible in older
children or neonates with no access to the umbilical or portal vein, as
in our case.
Though portal vein thrombosis is an extremely rare
complication of hepatic abscess in neonates, these case reports indicate
the need for repeated ultrasound supervision of neonatal hepatic abscess
for portal vein patency and regular follow up.
Contributors: SA was responsible for day to day
care of the patient and preparation of the draft. NBM was responsible
for interpretation of data, finalization of the draft and will act as
guarantor for the paper. AG was responsible for interpretation of
radiological findings and contributed to drafting of the paper.
Funding: None.
Competing interest: None stated.
