|
|
|
Indian Pediatr 2021;58:1052-1055 |
 |
Diagnosis
and Assessment of Severity of Pediatric Pneumonia
Using the Respiratory Index of Severity (RISC)
Scoring System
|
|
Kalyani Pillai, 1
Edwin Ros Sartho,1
TP Lakshmi,2
V K Parvathy1
From Departments of 1Pediatrics and
2Radiodiagnosis, Amala Institute of Medical
Sciences, Thrissur, Kerala.
Correspondence to: Dr Kalyani Pillai, Professor
of Pediatrics, Amala Institute of Medical Sciences,
Amala Nagar, Thrissur 680 555, Kerala.
Email:
[email protected]
Received: August 29, 2019;
Initial review; February 01, 2020;
Accepted: August 09, 2020.
|
Objectives: To evaluate the correlation
between the Respiratory Index of Severity (RISC)
scoring system and the World Health Organization
(WHO) interpretation of chest radiographs, and
to evaluate the RISC scoring system in the
diagnosis and assessment of severity of
pneumonia in children against chest X-ray.
Methods: 241 children presenting to a
tertiary care center with a clinical diagnosis
of pneumonia that necessitated a chest
radiograph to be taken, were enrolled. The RISC
scoring was done for all participants by a
single pediatrician and chest X-ray
graded by a single radiologist as per the WHO
interpretation of chest radiographs. Results:
There was a statistically significant positive
correlation (P=0.02) between the two
scores. RISC score of >1 had a sensitivity of
80.3%, and score
³3
had a specificity of 88.3%, positive predictive
value of 61.3% and negative predictive value of
76.8% for diagnosis and to predict severity of
pneumonia. Conclusion: In a
resource-limited setting, RISC scoring can be
used to diagnose and predict the severity of
childhood pneumonia.
Keywords: Community-acquired
pneumonia, Severity, X-ray chest.
|
|
T
he
Respiratory Index of Severity (RISC) scoring
was formulated in South Africa to provide a
standardized means of quantifying severity of
respiratory illness among children during
epidemiologic studies [1]. This score has a negative
score for wheezing, which potentially excludes
children with wheezing, a probable drawback of the
Integrated Management of Childhood Illness (IMCI)
developed by the World Health Organization (WHO).
The gold standard for diagnosis
of pneumonia is the chest X-ray (CXR). In an
attempt to improve the consistency of CXR
interpretation between epidemio-logical studies, the
WHO standardized the interpretation of CXRs for the
diagnosis of pneumonia in children [2,3]. The CXR
interpretation exercise was done and validated under
WHO [4]. If the RISC scoring system correlates well
with CXR, this scoring system could be of use in
resource-poor settings where CXR is not routinely
available. The aim of the study was to evaluate the
correlation between the RISC scoring system and the
WHO interpretation of chest radiographs. It also
aims to evaluate the RISC scoring system in the
diagnosis and assessment of severity of pneumonia in
children by validating it against the CXR.
METHODS
This descriptive study was
undertaken at a semi-urban tertiary care hospital in
India from 1 February, 2018 to 31 July, 2018. The
study was approved by the institutional ethics
committee and informed consent from parents was
taken prior to enrollment. Consecutive patients aged
1 month to 12 years, who visited the pediatric OPD
and/or got admitted in the pediatric ward with a
clinical diagnosis of pneumonia by the treating
doctor, and which necessitated a chest radiograph to
be taken, were enrolled for the study. Exclusion
criteria were subjects with documented congenital
heart disease, chronic respiratory illness,
congenital lung problems, immunosuppressive
conditions or known to have neuromuscular disorders
with respiratory system involvement.
For calculation of sample size,
prevalence of lower acute respiratory infection was
taken as 28% [5]. At significance level of 5%, with
20% relative precision, and power of the study 80%,
sample size was calculated as 240. To allow for
potential recruitment failure rate, 285 children
were assessed for eligibility for enrollment in the
study.
A detailed history was taken and
respiratory system examination done for all
subjects, and RISC scoring for HIV non-infected
children [1] was done by the principal investigator.
Variables in the the RISC score represent known risk
factors for severe outcomes of pneumonia in
children, with a maximum score of 8 points.
CXR scoring was done by a single
radiologist, as per the WHO interpretation of chest
radiographs [2,4] .
Statistical analysis:
Analysis was done using Spearman rho (ñ) correlation
to assess the correlation between RISC score and WHO
CXR score. We divided the children into two groups
by using the WHO CXR score of 3 (lobar pneumonia on
X-ray) as a cut off. Group A with CXR score
<3 were clinically suspected by physician but CXR
was not suggestive of pneumonia, and group B with
CXR score ³3,
clinically suspected by physician and also CXR
suggestive of pneumonia. By plotting the receiver
operating characteristic (ROC) curve, we calculated
specificity and sensitivity to determine the
appropriate RISC score to diagnose and predict the
severity of pneumonia. Analysis was done by
Statistical Software Package for Social Sciences
Version 23 (SPSS 23)
RESULTS
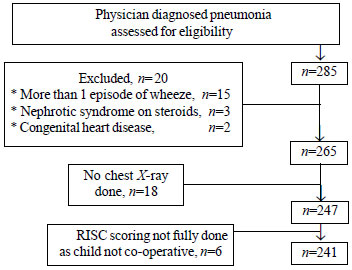
A total of 285 children with
physician-diagnosed pneumonia were assessed for
eligibility to be enrolled in the study (Fig. 1).
Out of these, 20 were excluded based on exclusion
criteria and 18 were excluded as a CXR was not
taken/available. A total of 241 children were
finally included in the study.
 |
|
Fig. 1 Study flow
chart.
|
Baseline clinical characteristics
are presented in Table I. Of the study
subjects 34 (14.1%) had a RISC score
³3
and 61 (25.3%) had a CXR score
³3.
Table I Clinical Profile, Respiratory Index of Severity (RISC) score, and Chest X-ray Score of
Children With Physician-Diagnosed Pneumonia (N=241)
| Characteristics |
No (%) |
| Male |
142 (58.9 |
| Age |
|
| 1mo-1 y |
96 (39.8) |
| 1y-5y |
112 (46.5) |
| 5-12 y |
33 (13.7) |
| Symptoms |
|
| Fever |
205 (85) |
| URI symptoms |
223 (92) |
| Breathlessness |
40 (16.5) |
| Feed refusal |
219 (90.8) |
| Immunization as per NIS |
239 (99.2) |
| Disease severity based
on treatment |
|
| Outpatient treatment |
90 (37.3) |
| Admission as
inpatient |
140 (58.1) |
| Pediatric intensive
care unit admission |
11 (4.6) |
| CXR score |
|
| 1 |
141(58.5) |
| 2 |
39 (16.1) |
| 3 |
42 (17.1) |
| 4 |
16 (6.5) |
| 5 |
3 (1.2) |
| RISC score |
|
| 1 |
59 (24.6) |
| 2 |
148 (61.2) |
| 3 |
6 (2.5) |
| 4 |
26 (10.9) |
|
≥5 |
2 (0.8) |
| URI-Upper
respiratory tract infection. |
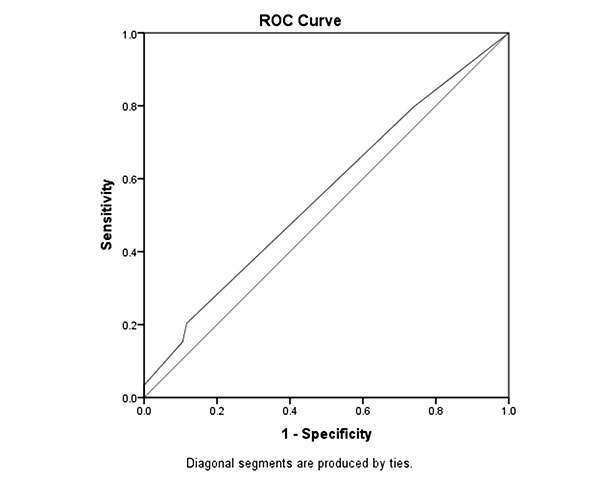
There was a statistically
significant positive correlation between RISC score
and WHO CXR score (r=0.144, P=0.025). The ROC
curve was plotted (Fig. 2). Taking WHO CXR
score of ³3
(lobar pneumonia score 3) as severe pneumonia, a
RISC score of >1 had a sensitivity of 80.3% and
specificity of 26.1%, suggesting it is a moderate
screening test for pneumonia. A RISC score of
³3
had a sensitivity of 21.3% and specificity of 88.3%
for diagnosis and to predict severity of pneumonia (Table
II).
Table II Test Characteristics of the Respiratory Index of Severity (RISC) Score (N=241)
| Characteristicsa |
RISC threshold
|
RISC threshold
|
|
score >1 |
score ³3 |
| Sensitivity (%) |
80.3 |
21.3 |
| Specificity (%) |
26.11 |
88.3 |
| PPV (%) |
25.9 |
61.7 |
| NPV (%) |
79.6 |
76.8 |
| Accuracy (%) |
39.8 |
71.3 |
| aUsing CXR
WHO score 3 as diagnosis of lobar
pneumonia. |
 |
|
Fig. 2 ROC curve for
Respiratory Index of Severity (RISC)
scoring system in pediatric pneumonia.
|
DISCUSSION
There are hardly any scoring
systems which are validated for community-acquired
pneumonia (CAP) in Indian children that would have
high utility in resource-limited settings. We
demonstrated a statistically signi-ficant
correlation between RISC scoring system [1] and the
WHO interpretation of chest radiographs [2].
Limitations of the study were
that RISC score is not useful to differentiate
between types of pneumonia based on etiology. RISC
score is not useful to monitor resolution of
symptoms. A negative score for wheeze (-2) may
encourage false negatives. When developing detection
tests, a balance must be chosen between risks of
false negatives and false positives.
The major scoring systems
designed to predict mortality risk and serve as
guides for admission in community-acquired pneumonia
(CAP) are for adults [6], and such scores for
children are scarce [7,8]. Only the modified
predisposition, insult, response and organ
dysfunction (PIRO) score has so far been applied to
children with CAP [6]. We used the RISC score for
our study as it has six predictors for assessing the
severity of pneumonia (hypoxia, chest indrawing,
feed refusal, wheeze, malnutrition, age) and is easy
to administer. Other risk models [9,10] are
relatively cumbersome to administer.
The WHO introduced the Integrated
Management of Childhood Illness (IMCI) to
standardize and improve treatment and thus prevent
major causes of death in children <5 years [10]. The
first drawback of IMCI diagnostic criteria is of
over-diagnosing pneumonia by including children with
wheezing. In our study too, 36.5% of patients had a
wheeze on presentation. However, the RISC scoring
system overcomes this by giving a negative score for
wheezing. The second drawback of IMCI is a missed
diagnosis, as it has a low sensitivity [11,12].
Hooli, et al. [13] did an
external validation of RISC by calculated
classification performance measures at thresholds of
3 and 4. Using a RISC score of 3 had a sensitivity
of 59% and specificity of 78%. With a score
threshold of 4, the sensitivity was 32.6% and
specificity was 93.1%. A median RISC score of 1
corresponded with a risk of mortality of 0% (95%CI:
0%-0.6%) in the study by Reed, et al. [1]. In our
study, using a RISC score of >1 had a higher
sensitivity and was a moderate screening test to
predict pneumonia.
Validation of Bacterial pneumonia
score (BPS) score was done with multiplex PCR
examinations of blood specimens by Imilda, et al.
[14]. BPS had 69% sensitivity and 60% specificity,
42% positive predictive value, and 81% negative
predictive value. In our study, which was validated
with X-ray chest, a RISC score of
³3
had a higher specificity and positive predictive
value and almost similar negative predictive value
for diagnosis and to predict severity of pneumonia.
To conclude, we propose that RISC
score may be used for diagnosing pneumonia in
resource-constrained areas to supplement IMCI
protocols. Assessment of a combination of the two in
community-based studies may provide additional
information on this aspect.
Ethics clearance: Amala
Institute of Medical Sciences; No. AIMSIEC/05/2018
dated January 22, 2018.
Contributors: KP: concept and
design of the study; ERS: analyzed and collected
data; drafted the manuscript; TPL: analyzing data;
VKP: supervised cognitive and behavioral
assessments. All authors approved the final version
of manuscript, and are accountable for all aspects
related to the study.
Funding: None; Competing
interest: None stated.
| |
|
What this Study Adds?
•
In a resource-limited setting, where
chest X-ray is unavailable, RISC
scoring can be used for diagnosing and
predicting the severity of
community-acquired pneumonia.
|
REFERENCES
1. Reed C, Madhi SA, Klugman
KP, et al. Development of the respiratory index
of severity in children (RISC) score among young
children with respiratory infections in South
Africa. PLoS One. 2012;7:e27793.
2. Cherian T, Mulholland EK,
Carlin JB, et al. Standardized interpretation of
paediatric chest radiographs for the diagnosis
of pneumonia in epidemiological studies. Bull
WHO. 2005;83:353-9.
3. O’ Grady KA, Torzillo PJ,
Ruben AR, et al. Identification of radiological
alveolar pneumonia in children with high rates
of hospitalized respiratory infections:
comparison of WHO - defined and pediatric
pulmonologist diagnosis in the clinical context.
Pediatr Pulmonol. 2012;47:386-92.
4. Taylor E, Haven K, Reed P;
SHIVERS Investigation Team. A chest radiograph
scoring system in patients with severe acute
respiratory infection: A validation study. BMC
Med Imaging. 2015;15:61.
5. Prietsch Silvio OM,
Fischer Gilberto B, César Juraci A, et al. Acute
lower respiratory illness in under-five children
in Rio Grande, Rio Grande do Sul State, Brazil:
Prevalence and risk factors. Cad Saúde Pública.
2008; 24:1429-438.
6. Uwaezuoke SN, Ayuk AC.
Prognostic scores and bio-markers for pediatric
community - acquired pneumonia: How far have we
come? Pediatric Health Med Ther. 2017; 8:9-18.
7. Arbo A, Lovera D, Martínez
– Cuellar C. Mortality predictive scores for
community – acquired pneumonia in children. Curr
Infect Dis Rep. 2019;21:10.
8. Moreno L, Krishnan JA,
Duran P, Ferrero F. Development and validation
of a clinical prediction rule to distinguish
bacterial from viral pneumonia in children.
Pediatr Pulmonol. 2006;41:331-7. Erratum in:
Pediatr Pulmonol. 2006;41:494.
9. Williams DJ, Zhu Y,
Grijalva CG, et al. Predicting severe pneumonia
outcomes in children. Pediatrics. 2016;138:
e20161019.
10. Emukule GO, McMorrow M,
Ulloa C, et al. Predicting mortality among
hospitalized children with respiratory illness
in Western Kenya, 2009-2012. PLoS ONE. 2014;
9:e92968.
11. Deodari AK, Chellani H,
Carlin JB, et al. Clinico-epidemiological
profile and predictors of severe illness in
young infants (<60 days) reporting to a hospital
in North India. Indian Pediatr. 2007;44:739-48.
12. Uwemedimo OT, Lewis TP,
Essien EA, et al. Distribution and determinants
of pneumonia diagnosis using Integrated
Management of Childhood Illness guidelines: A
nationally representative study in Malawi. BMJ
Glob Health. 2018;3:e000506.
13. Hooli S, Colbourn T,
Lufesi N, et al. Predicting hospitalised
paediatric pneumonia mortality risk: An external
validation of risc and mrisc, and local tool
development (RISCMalawi) from Malawi. PLoS One.
2016;11:e0168126.
14. Imilda I, Yani FF, Hariyanto D, Basir D.
Bacterial pneumonia score to identify bacterial
pneumonia, Paediatr Indones. 2015;55:79-82.
|
|
|
 |
|

