|
|
|
Indian Pediatr 2020;57:
1074-1075 |
 |
Deficiency of Adenosine Deaminase 2 (DADA2) –
A New Autoinflammatory Disease with Multisystem Features
|
|
Raju Khubchandani1* and Ivona Aksentijevich2
1Department of Pediatric Rheumatology, SRCC
Children’s Hospital, Mumbai, India; and 2Inflammatory Disease
Section,
National Human Genome Research Institute, National Institutes of Health,
Bethesda, Maryland, USA.
Email:
[email protected]
Published online: August 14, 2020;
PII: S097475591600231
|
|
A
male child born to a non-consanguineous couple
had been extensively investigated for recurrent, prolonged febrile
episodes from 2005 to 2011. The fever episodes were accompanied by
multisystem manifestations consisting of myalgia, arthralgia, rashes,
recurrent and episodic severe abdominal pain (one episode leading to an
appendicectomy), episcleritis, generalized adenopathy and hepatomegaly
[1]. Mutation testing for then known auto-inflammatory diseases
including Tumor necrosis factor receptor associated periodic syndrome
(TRAPS) was negative. TRAPS was considered as the best fit clinical
diagnosis considering that literature had identified subsets of patients
with a clinical profile matching TRAPS without mutations in the
TNFRSF1A gene. The family was advised to start Tumor necrosis factor
(TNF) blocker, etanercept at the dose of 0.4 mg/kg subcutaneously twice
weekly, after tuber-culosis screening. The patient’s symptoms including
fever, arthralgia, myalgia, and abdominal pain abated rapidly with
normalization of his anthropometry over the next 2 years. His complete
blood counts, Erythrocyte Sedimentation Rate (ESR) and C Reactive
Protein (CRP), also normalized and stayed stable over the next seven
years.The cost of etanercept lead to a gradual, progressive
self-titration of dose to 0.4 mg/kg every 20-22 days, at which point
symptoms would recur.
In January 2019, at age 20 years, he was diagnosed
with asymptomatic hypertension (180/120 mmHg) during a pre-employment
check. Urinalysis was normal and serum creatinine was 0.91 mg/dL with
e-GFR of 114 mL/hr. His 2D-echocardio-gram showed mild concentric left
ventricular hypertrophy with grade 2 diastolic dysfunction suggesting
long-standing hyper-tension. The ejection fraction was 60%. His kidneys
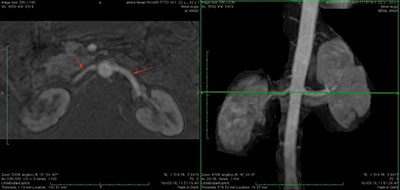
were of normal size. A magnetic resonance angiogram (MRA) showed diffuse
narrowing of the right renal artery and scarring of the right kidney (Fig.
1). Positron emission tomography computerized tomography (PET-CT)
did not show any vascular inflammation. Whole exome sequencing (WES) in
the patient and his asymptomatic parents identified compound
heterozygous mutations (p. Gly47Arg (c.139G>C; p.G47R) and a splice
mutation c.753+2T>A). His father and mother were carriers of the
respective mutations. The patient was started on antihypertensive
therapy and etanercept was increased to 0.8 mg/kg once weekly starting
April 2019. He is doing well since and is presently additionally
receiving metoprolol 50 mg once daily.
 |
|
Fig. 1 MR angiogram showing diffuse
narrowing of the right renal artery and scarring of the right
kidney.
|
DADA2 was described independently by two groups in
2014, and considerable time after our patients first presentation and
report [2,3]. Now over 200 patients have been reported globally. Its
prevalence is higher in endogamous populations (Middle Eastern
countries) or in founder populations (Finnish, Dutch). Our patient hails
from the endogamous Agarwal community and we have since diagnosed two
other children of the same community with DADA2 homozygous for the
p.Gly47Arg (c.139G>C; p.G47R) mutation.
Typically features begin in early childhood or
adolescence. Vasculopathy/vasculitis (polyarteritis nodosa, lacunar
infarcts) and hematological manifestations remain the cardinal features
[4]. Hypertension has been described in 21%, renal artery stenosis in 4%
of patients, and cases with large vessel involve-ment have been
reported. Notable in our patient is an episode of acute abdomen for
which he underwent appendicectomy. Uncommonly DADA2 can present as a
polyarteritis nodosa (PAN)-like disease in adults. Screening such
patients for ADA2 activity can radically modify management.
Laboratory findings are non-specific and include
elevated acute phase reactants during flares and raised transaminases.
Positive lupus anticoagulant autoantibodies have been noted in some.
Sharma, et al. [5] have reported DADA2 in a 35 year old woman
also from the Aggarwal community, who presented as a APLA-like syndrome
with recurrent abortions [5]. The G47R pathogenic variant has been
described in DADA2 patients from Middle East and South Asia and with an
allele frequency higher than in other populations (Caucasian, Latino,
African). Functional protein assay on fresh serum or plasma samples,
which detects low or absent ADA2 enzymatic activity or measuring ADA2
catalytic activity on dried plasma filter paper spots can provide a
rapid confirmatory protein diagnosis.
Despite the increasing availability and reducing
costs of genetic testing, challenges of cost, interpretation, and long
turn-around times exist. Our patient’s samples awaited analysis at
National Institutes of Health (NIH) (a global referral center for
autoinflammatory diseases) for WES and were fast-tracked after recent
developments. It was serendipitous that the child was started on
etanercept in 2011. Retrospectively, spacing the doses for cost
considerations was not prudent since the child has developed a
vasculopathy with renal scarring. Anti-TNF agents prevent and eliminate
vasculitis symptoms in DADA2 patients with a remarkable reduction in
ischemic stroke risk [6]. They decrease inflammatory burden of the
disease, increase growth and development, and improve some hematological
manifestations such as anemia and thrombocytopenia. Thalidomide has been
reported useful in a large study. Aspirin and anticoagulants are
contraindicated since hemorrhage may complicate the stroke.
Hematopoietic stem cell transplantation can be curative in patients who
present with bone marrow failure or are non-responsive to anti-TNF
therapy [4].
In conclusion, pediatricians in India must be aware
of this recently discovered entity and its myriad presentations,
including PAN, early-onset strokes, arterial obliterations,
immunodeficiency, and aplastic anemia. With high rates of consanguinity
and endogamy in several parts of India, we believe more patients of
hereditary auto-inflammatory diseases would be diagnosed with increasing
physician awareness and availability of genetic testing.
REFERENCES
1. Dhanrajani A, Khubchandani RP. Modified regimen of
etanercept for tumor necrosis factor receptor associated periodic
syndrome (TRAPS) like illness. Indian Pediatr. 2014;51:55-7.
2. Zhou Q, Yang D, Ombrello A, Zavialov A, Toro C,
Zavialov A, et al. Early-onset stroke and vasculopathy associated
with mutations in ADA2. N Engl J Med. 2014; 370:911-20.
3. Navon Elkan P, Pierce S, Segel R, Walsh T, Barash
J, Padeh S, et al. Mutant adenosine deaminase 2 in a
polyarteritis nodosa vasculopathy. N Engl J Med. 2014;370:921-31.
4. Meyts I, Aksentijevich I. Deficiency of Adenosine
Deaminase 2 (DADA2): Updates on the phenotype, genetics, pathogenesis,
and treatment. J Clin Immunol. 2018;38:569-78.
5. Sharma A, Naidu G, Chattopadhyay A, Acharya N, Jha
S, Jain S. Novel CECR1 gene mutations causing deficiency of adenosine
deaminase 2, mimicking antiphospholipid syndrome. Rheumatology.
2019;58:181-2.
6. Ombrello A, Qin J, Hoffmann P, Kumar P, Stone D,
Jones A, et al. Treatment strategies for deficiency of adenosine
deaminase 2. N Engl J Med. 2019; 380:1582-4.
|
|
|
 |
|

