|
|
|
Indian Pediatr 2019;56: 923-928 |
 |
Validity of Maternal Report of Birthweight in
a Cohort Study and Its Implication on Low Birthweight Rate Using
Simulations
|
|
Akshay Swaminathan 1,
Tinku Thomas2,
Daniel J Corsi3,
Pratibha Dwarkanath4,
SV Subramanian5 and Anura V
Kurpad6
From Department of 1Statistics, Harvard
College, Cambridge, Massachusetts, USA; Department of 2Biostatistics,
St. Johnís Medical College, Bangalore, Karnataka; 3OMNI
Research Group, Clinical Epidemiology Program, Ottawa Hospital Research
Institute, Ottawa, Canada; Division of 4Nutrition, St. Johnís
Research Institute, Bangalore, Karnataka; Department of 5Social
and Behavioral Sciences, Harvard School of Public Health, Boston,
Massachusetts, USA and 6Department of Physiology, St. Johnís
Medical College, Bangalore, Karnataka, India.
Correspondence to: Dr Tinku Thomas, Department of
Biostatistics, St Johnís Medical College, St. Johnís National Academy of
Health Sciences, Bangalore - 560 034, Karnataka, India.
Email: [email protected]
Received: March 15, 2019;
Initial review: April 22, 2019;
Accepted: September 19, 2019.
|
|
Objective: Maternal recall
of birthweight is a convenient and cost-effective way to obtain
birthweight measurements when official records are unavailable. It is
important to assess the validity of maternal recall of birthweight
before using these measurements to draw conclusions about a population.
Methods: This is secondary analysis of data from a
previous cohort study. We analyzed actual and reported
birthweights of 200 mother-and-child pairs from Southern India. We
validated maternal report of birthweight by generating correlation
coefficients, summary statistics, and Bland-Altman plots. We ran
simulations to evaluate how misclassification as low or normal
birthweight changed with the mean birthweight of the cohort. Results:
Reported birthweight was strongly correlated with actual birthweight
(r=0.80, P<0.001); 55%, 78.5%, and 93% of subjects reported
values within 50 g, 250 g, and 500 g, respectively of actual birthweight.
None of sociodemographic covariates was significantly associated with
the accuracy of maternal recall of birthweight. 7.5% of children were
misclassified as either low or normal birthweight by reported
birthweight. Simulations revealed that increasing the reported and
actual birthweights by 500g reduces the misclassification rate from 7.5%
to 1.5%. Conclusion: Maternal recall is a sufficiently
accurate measure of actual birthweight. However, the distribution of
actual birthweight in the population must be taken into consideration
when classifying babies as low or normal birthweight, especially in
populations where mean birthweight is close to 2500g.
Keywords: Child health, Estimation,
Self-reported data.
|
|
M
any of the most pressing current global health
issues, including diabetes, cancer, obesity and cardiovascular disease,
have been linked to birthweight and body weight in early life [1-5].
Maternal report of birthweight is a convenient and cost-effective method
of obtaining birthweight measurements if accurate birth records are not
available, such as in certain developing countries. Assessing the
accuracy of this type of measurement is necessary to validate the
results of analyses that rely on maternal report of birthweight. Rate of
low birth weight in India is 18% [6]. The error in reporting of
birthweight by mothers may result in misclassification into low
birthweight category. There is currently no evaluation of the potential
misclassification of low birthweight due to measurement error arising as
a consequence of maternal report.
While previous studies have analyzed the accuracy and
correlates of maternal report of birthweight [7-13], most have focused
on cohorts from developed countries. We evaluated the accuracy of
maternal reports at varying time points ranging from 6 months to 7 years
after birth, and studied the association with various sociodemographic
characteristics.
Methods
Subjects were part of a prospective observational
cohort study in Southern India on 2001 pregnant women, and this report
is a secondary analysis of data from that study [14]. For this analysis,
we reviewed 200 mother-child pairs, for which we had 199 maternal
reports of birthweight and 200 measured birthweight. Pregnant women in
the age range of 17-40 years on their first visit for a registered
antenatal checkup were recruited in the pregnancy cohort from the
Department of Obstetrics of St. Johnís Medical College Hospital,
Bangalore, India. Infants were weighed to the nearest 10g on an
electronic weighing scale (Salter Housewares 914 Electronic Baby and
Toddler Scale, NY, USA) immediately after birth. Data on maternal
education, possession, household income, sex and birth order of the
sampled child and parity of the mother were collected in the pregnancy
cohort.
As part of a study on inter-generational transmission
of nutrition, the last 1000 women in chronological order of pregnancy
cohort recruitment (women who delivered live babies from 2008 to 2013)
of the original 2,001 were identified as initial subjects for follow-up
analysis. Of these 1000 women, 560 were deemed valid for data collection
(others either did not have a valid phone number or address or were not
residents of Bangalore). Of these, using a questionnaire, one follow-up
data was finally collected from 200 consenting, contactable mothers
between December 2013 and December 2014, within 7 years after delivery.
The telephone numbers of the mother, spouse or other relatives which
were available in the pregnancy cohort were tried, to establish contact
and obtain residential address of the mother and the child. A maximum of
three home visits were made by a trained field worker to collect data,
once the telephonic contact was made with the mother. Birthweight
reported in kilograms by some mothers were converted to grams for
comparison with the birth records. Maternal and child age at the time of
revisit was collected. The institutional ethical review board of St.
Johnís Medical College Hospital approved the study protocols of both the
pregnancy cohort and the child follow-up study on inter-generational
transmission of nutrition.
Statistical analysis: All statistical analysis
was conducted on R version 3.3.2. Pearson correlation coefficients and
interclass correlation coefficients (ICC) for absolute agreement were
calculated to quantify correlation between actual and reported
birthweight. Paired t-tests were used to compare actual and reported
birthweight overall and in different subgroups (<3 years old, 3-5 years
old, >5 years old, low birthweight (LBW), and normal birthweight. LBW
was defined as <2500 g and normal birthweight was defined as
≥2500 g in measured
weight. Independent sample t-test was used to compare the difference
between reported and actual birthweight in LBW and normal birthweight
infants. Bland-Altman plots with limits of agreement [Mean difference (2
SD)] were used to assess the difference between actual and reported
birthweight. Sensitivity, specificity, positive predictive values (PPV),
and negative predictive values (NPV) were calculated for reported
classification of infants as LBW or normal birthweight, as well as
proportion of misclassified children. Cumulative percent accuracy
calculations were used to determine accuracy of reported birthweight
within increasing margins of error. Linear regression and subsequent
multiple linear regression was used to determine the association between
23 sociodemographic variables and the accuracy of reported birthweight.
Linear regression was also used to compare the effect of using reported
vs actual birthweight as both independent (for child growth) and
dependent variables (on maternal characteristics) in regression
analysis. The regression coefficients between the reported and actual
birthweight were compared using 95% confidence intervals (CI). In
addition, we generated a simulated dataset of 2000 actual and reported
birthweights to illustrate how the distribution of actual birthweight
affects misclassi-fication. The simulated actual birthweights were drawn
from a normal distribution with mean 2878 g and standard deviation 400 g
and then scaled to the mean. The simulated reported birthweights were
set as the simulated actual birthweights plus a normally distributed
error term with mean 10 g and standard deviation 300 g. Parameters for
the simulated dataset were estimated based on the summary statistics of
our study cohort.
Results
The median age of children at revisit was 41 months (Table
I). The average measured birthweight of the original cohort was 2870
g (450 g) and that of the revisit sub-sample of 200 children was 2878 g
(406 g) (Table II). The average reported birthweight was
2889 g, which strongly correlated with actual birthweight (r=0.80 and
ICC=0.79). Correlation remained high (r>0.8) across all age groups. ICC
was high for normal birthweight babies (0.71) than for LBW babies
(0.29).
TABLE I Socio-Demographic Characteristics of the Revisit Cohort (N=200)
|
Characteristics |
Value |
|
Childís age at follow-up (mo)# |
41 (22, 57.25) |
|
Age of mother at follow-up (y)# |
27 (24, 30) |
|
Years of education of mother# |
12 (10, 15) |
|
Total number of possessions# |
17 (16, 19) |
|
Yearly household income (INR)# |
15000 (10000, 27250) |
|
Yearly household income during
|
14000 (10000, 23500) |
|
pregnancy (INR)# |
|
Male sex |
104 (52) |
|
Motherís education level$
|
|
Up to secondary |
63 (32) |
|
Diploma or higher secondary |
57 (29) |
|
Degree |
42 (21) |
|
Professional degree |
22 (11) |
|
Post graduate or above |
15 (8) |
|
First in birth order$ |
140 (70) |
|
Parity of mother$ |
|
|
1 |
97 (49) |
|
2 |
98 (49) |
|
3 |
4 (2) |
|
Possessions$ |
|
Flush Toilet
|
56 (28) |
|
Running cold water |
149 (75) |
|
Running hot water |
83 (42) |
|
Car |
51 (26) |
|
Two-wheeler |
161 (81) |
|
Television |
197 (99) |
|
Refrigerator |
131 (66) |
|
Washing machine |
83 (42) |
|
Fixed telephone |
19 (10) |
|
Radio |
28 (14) |
|
#Median (IQR); $n (%); INR: Indian
Rupee (65 INR = 1 US dollar).
|
TABLE II Reported, Actual and Difference (ReportedĖActual) in Birthweight
|
Reported/Actual, n |
Reported BW |
Actual BW |
Difference BW |
|
Overall |
199/200 |
2889 (2820, 2959) |
2878 (2822, 2935) |
13 (-29, 54) |
|
Low BW |
38/38 |
2337 (2222, 2451) |
2314 (2254, 2373) |
23 (-86, 132) |
|
Normal BW |
161/162 |
3020 (2952, 3087) |
3010 (2961, 3060) |
10 (-35, 55) |
|
Current age |
|
|
|
|
|
<3 years |
87 |
2883 (2774, 2991) |
2889 (2799, 2978) |
-6 (-62, 49) |
|
3-5 years |
72 |
2891 (2768, 3013) |
2886 (2789, 2982) |
10 (-78, 98) |
|
>5 years |
41 |
2900 (2759, 3042) |
2842 (2729, 2956) |
59 (-9, 126) |
|
Values are Mean (95% CI); BW: Birthweight. |
 |
|
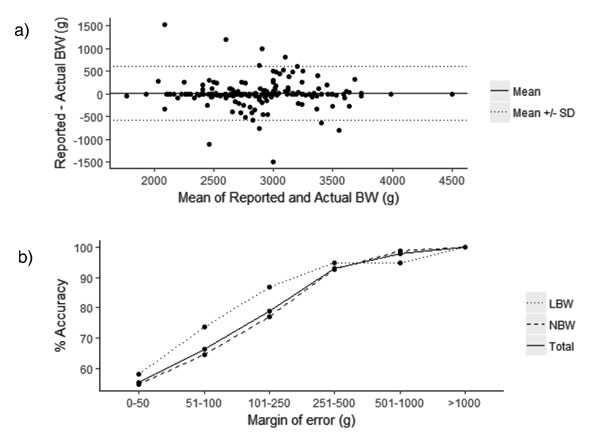
Fig. 1 (a) Bland-Altman plot of
actual and reported birthweights (BW). Points on graph represent
difference in BW (Y-axis) against mean of reported and measured
BW. Solid line: Mean difference. Dotted line: Mean difference Ī2
SD. (b) Cumulative percent accuracy plot of maternal reports.
Points on the graph represent the cumulative percent accuracy of
reported BW within various margins of error. The dotted line
represents actual LBW babies, the dashed line actual NBW babies,
and the solid line all babies.
|
Bland-Altman plots revealed the difference between
each pair of reported and actual birthweight versus the mean of each
pair (Fig. 1a). The mean difference between reported and
measured birthweight was 13 g (95% CI: -29 to 54). The difference was
randomly distributed about zero (Mean=152 g, paired t-test P=0.83),
suggesting that mothers of LBW children are not more likely to over or
under-report their birthweight compared to mothers of normal birthweight
children. The upper and lower limits of agreement of the Bland-Altman
plot were 23 and 83 g, respectively.
We calculated the accuracy of reported birthweight
within increasing margins of error for more insight into the bias.
Overall, 110 (55%) subjects reported birthweight within 50 g of actual,
157 (78.5%) subjects reported birthweight within 250 g of actual, and
185 (93%) subjects reported BW within 500 g of actual (Fig. 1b).
Treating reported BW as a test that can either be positive (reported Low
Birthweight) or negative (reported Normal Birthweight), sensitivity,
specificity, PPV, and NPV were calculated to be 77%, 96%, 83%, and 94%,
respectively against the actual. 7.5% (15/199) of children were
misclassified according to reported birthweight.
In simple linear regression, only one out of 23
sociodemographic variables, whether or not the family possessed a
television, was a significant determinant of the accuracy of reported
birthweight. Multiple linear regression showed no significant
associations between any of the sociodemographic variables and the
accuracy.
We conducted linear regressions using reported
birthweight and actual birthweight as either the independent or
dependent variable to assess how using reported birthweight instead of
actual birthweight affects the estimate for the regression coefficient (Web
Fig. 1). In each pair of regressions, the 95% CI for the
regression estimate using reported birthweight largely overlapped with
the 95% CI of the coefficient estimate for the regression using actual
birthweight, indicating that there is no sufficient evidence of a
difference in estimates by either using reported or actual birthweights.
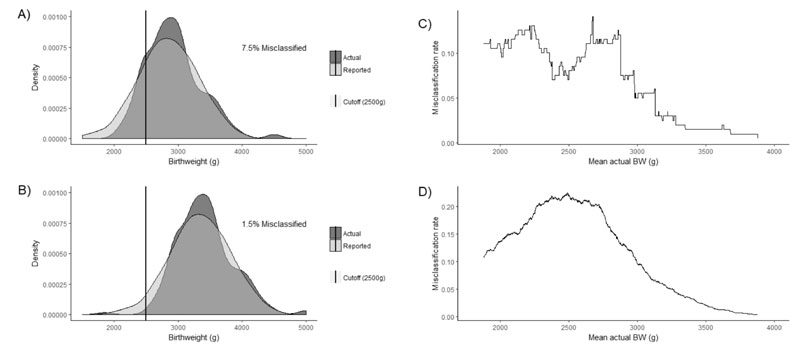
To illustrate how the distribution of actual
birthweight in a population affects the misclassification rate, we
analyzed the distribution of our cohort and a simulated dataset of 2000
actual and reported birthweight. Fig. 2a shows the
distribution of BW in our study cohort, and Fig. 2b shows
the distribution of birthweight in our study cohort after a positive
shift of 500 g. The 7.5% misclassification rate drops to 1.5% after the
500 g shift. Fig. 2c and 2d show how
misclassification rate changes with varying mean actual birthweight. In
both the study cohort (Fig. 2c) and simulated population (Fig.
2d), the highest misclassification rate occurs when the mean actual
birthweight is between approximately 2250 g and 2750 g.
Misclassification rate drops quickly as the mean actual birthweight
passes 2750 g.
 |
|
Fig. 2 (a) Distribution of
study cohort with mean actual birthweight (BW) 2878 g resulting
in 7.5% misclassification; (b) Distribution of shifted study
cohort with mean actual BW 3378 g resulting in 1.5%
misclassification; (c) Misclassification rate vs. mean actual BW
in study cohort; (d) Misclassification rate vs. mean actual BW
in simulated cohort.
|
Discussionnn/p>
Our results indicate that maternal report of
birthweight is a sufficiently accurate measure of the actual birthweight.
However, it must be emphasized that relying on maternal report is not
appropriate in all contexts, regardless of the accuracy of this metric.
Although it may be sufficiently accurate in surveys where actual
birthweight data is unavailable, population assessments, prevalence
estimates and trials with birthweight as an outcome should use recorded
birthweight data in order to maintain the highest standards of accuracy.
Studies from other countries have reported slightly
higher overall correlations, [7,9,10,12,13]. Similarly, strong
correlations across the three age groups indicate that age of child does
not influence the difference between reported and actual birthweight.
The correlation and ICC were lower for the LBW group; however, there was
no association between sociodemographic variables and accuracy of
reported birthweight. This suggests that maternal report of birthweight
is a stable measurement that is not influenced by attributes of the
child, by attributes of the mother, or by attributes of the household.
That is, recall bias was found to be random. Comparison of percent
accuracy measurements of reported birthweight between our cohort and
other studies show lower, yet still comparable rates of accuracy [7,10].
In order to explore the differential effects of using
reported and actual birthweight as outcome and predictor variables, we
conducted two linear regressions where birthweight was considered as a
dependent variable with maternal education and maternal height as
predictors and 2 additional regressions where birthweight was a
predictor for child height and height to age Z score (HAZ) at
follow up. We found no significant differences in the regression
coefficient estimates when reported birthweight was used instead of
actual birthweight in linear regression, indicating that reported
birthweight is a sufficiently accurate proxy for actual birthweight in
linear regression analyses. There were similar associations of
birthweight with maternal education and child growth in subsets of
actual and reported birthweights in NFHS-3 data.
Sensitivity analysis revealed that 7.5% of children
would be misclassified as LBW or normal birthweight. This is notably
higher than the 1.1% [7] and 1.6% [8] misclassification rates in
previous cohorts studies. It is important to note that the proportion of
misclassified children is not necessarily an indicator of the accuracy
of maternal report; rather, it depends greatly on the distribution of
birthweight in the population as well as the cutoff of 2500 g used for
LBW and normal birthweight.
Maternal report in our cohort from Southern India is
more likely to result in misclassification than previous cohorts [7,8],
since our cohort had more birthweights near the cutoff weight for LBW.
Since association studies between birthweight and
disease may require dividing subjects into groups based on birthweight
cutoffs, populations where the distribution centers around the cutoff
value may experience higher rates of misclassification. This suggests
that in countries such as India, where average birthweight is closer to
the cutoff for LBW, studies that use maternal report may be
misclassifying a larger proportion of children. Moreover, small changes
in birthweight distribution may lead to significant fluctuations in
misclassification rate.
The limitations of our study are our relatively small
sample cohort size, as well as low variability in certain
sociodemographic variables. Moreover, this was a follow-up study on
women who had earlier participated in a cohort and there is a
possibility of more accurate reported birthweight, in this sample than
in a general population.
In conclusion, while actual accurate measurements of
birthweight are required in many studies, we corroborate findings from
previous studies that maternal report of birthweight is a sufficiently
accurate proxy for actual birthweight. We have also elucidated that the
maternal report is not influenced by sociodemographic character-istics
of the child, mother, or household. An important area of investigation
for future studies would be on the effect of distribution of birthweight
in a population, on misclassification of children as low birthweight.
This is an especially relevant question in developing countries like
India, where research studies and national maternal and child health
indicators may depend on maternal report of birthweight due to
unavailability of accurate birth records.
Acknowledgments: AS acknowledges the helpful
comments provided by his colleagues at St. Johnís Research Institute.
Contributors: AS: led statistical analysis and
drafted the manuscript; TT: conceived the original study idea, edited
the manuscript, and contributed to study design; DJC: revised manuscript
and contributed to follow up study design; PD: revised the manuscript
and contributed to follow up study design; SVS: contributed to follow up
study design and revised manuscript; AVK: contributed to study design
and reviewed the manuscript. All authors read and approved the final
manuscript.
Funding: No direct financial support or funding
was obtained to conduct this study. Funding for the follow-up cohort was
study was provided by the Harvard Centre for Population and
Developmental Studies, Boston, USA. AS was supported by the Harvard
Global Health Institute. The funders had no role in study design, data
collection and analysis, decision to publish, or preparation of the
manuscript.
Competing interests: None stated.
|
What This Study Adds?
ē Maternal report was found to be an adequate
proxy for actual birthweight
ē Rate of misclassification as either low birthweight or
normal birthweight was 7.5%, higher than in reports from
high-income countries.
|
Referencess
1. Barker DJ, Winter PD, Osmond C, Margetts B,
Simmonds SJ. Weight in infancy and death from ischaemic heart disease.
Lancet. 1989;2:577-80.
2. Curhan GC, Chertow GM, Willett WC, Spiegelman D,
Colditz GA, Manson JE, et al. Birth weight and adult hypertension
and obesity in women. Circulation. 1996;94:1310-5.
3. Forsen T, Eriksson J, Tuomilehto J, Reunanen A,
Osmond C, Barker D. The fetal and childhood growth of persons who
develop type 2 diabetes. Ann Intern Med. 2000;133:176-82.
4. McCormack VA, dos Santos Silva I, Koupil I, Leon
DA, Lithell HO. Birth characteristics and adult cancer incidence:
Swedish cohort of over 11,000 men and women. Int J Cancer.
2005;115:611-7.
5. Rich-Edwards JW, Colditz GA, Stampfer MJ, Willett
WC, Gillman MW, Hennekens CH, et al. Birthweight and the risk for
type 2 diabetes mellitus in adult women. Ann Intern Med.
1999;130:278-84.
6. International Institute for Population Sciences
(IIPS) and ICF. National Family Health Survey (NFHS-4), 2015-16: India.
Mumbai: IIPS; 2017.
7. Adegboye AR, Heitmann B. Accuracy and correlates
of maternal recall of birthweight and gestational age. British J Obs
Gynec. 2008;115:886-93.
8. Gayle HD, Yip R, Frank MJ, Nieburg P, Binkin NJ.
Validation of maternally reported birth weights among 46,637 Tennessee
WIC program participants. Public Health Rep. 1988;103:143-7.
9. Olson JE, Shu XO, Ross JA, Pendergrass T, Robison
LL. Medical record validation of maternally reported birth
characteristics and pregnancy-related events: a report from the
Childrenís Cancer Group. Am J Epidemiol. 1997;145:58-67.
10. OíSullivan JJ, Pearce MS, Parker L. Parental
recall of birth weight: how accurate is it? Arch Dis Child.
2000;82:202-3.
11. Sanderson M, Williams MA, White E, Daling JR,
Holt VL, Malone KE, et al. Validity and reliability of subject
and mother reporting of perinatal factors. Am J Epidemiol.
1998;147:136-40.
12. Tomeo CA, Rich-Edwards JW, Michels KB, Berkey CS,
Hunter DJ, Frazier AL, et al. Reproducibility and validity of
maternal recall of pregnancy-related events. Epidemiology.
1999;10:774-7.
13. Walton KA, Murray LJ, Gallagher AM, Cran GW,
Savage MJ, Boreham C. Parental recall of birthweight: a good proxy for
recorded birthweight? Eur J Epidemiol. 2000;16:793-6.
14. Dwarkanath P, Barzilay JR, Thomas T, Thomas A,
Bhat S, Kurpad AV. High folate and low vitamin B-12 intakes during
pregnancy are associated with small-for-gestational age infants in South
Indian women: A prospective observational cohort study. Am J Clin Nutr.
2013;98: 1450-8.
|
|
|
 |
|

