|
|
|
Indian Pediatr 2018;55: 9 95-996 |
 |
Isolated Congenital
Tracheobiliary Fistula
|
|
Shweta Pathak, Shishir Jethi and Rajendra Saoji
From Department of Pediatrics, Shree Jagdish Children Hospital,
Jabalpur, Madhya Pradesh, India.
Correspondence to: Dr Shweta Pathak, 567, Anand colony Baldev Bag,
Jabalpur, Madhya Pradesh, India.
Email: [email protected]
Received: Àugust 19, 2017;
Initial review: January 01, 2018;
Accepted: June 04, 2018.
|
Background: Congenital tracheobiliary fistula is
a rare developmental anomaly with a persistent communication between the
biliary system and the trachea. Characteristics: A 7-day-old baby
with severe respiratory distress and aspiration pneumonia. Outcome:
Tracheobilliary fistula identified on bronchoscopy. Open surgical
excision of fistula was followed by improvement. Message: This
condition should be considered in the differential diagnosis of
intractable aspiration pneumonia.
Keywords: Aspiration pneumonia, Bronchoscopy, Neonate,
Respiratory distress.
|
|
C
ongenital tracheobiliary or bronchobiliary
fistula is a rare anomalous communication between the carina or the main
bronchus and the biliary system [1]. To date, only few cases have been
reported in the literature.
Case Report
A 7-day-old full term male baby, born to a
primi-gravida, by normal vaginal delivery and with immediate cry, had an
episode of vomiting immediately after a breastfeed given at an about 4-5
hours of birth. This was followed by increasing respiratory distress
which was managed initially at a local hospital, and then referred to
our center on day 2 of life. At admission, the baby was in severe
respiratory distress with heart rate of 160-170/min, respiratory rate of
80/min with retractions and saturation of 60-70% on room air; arterial
blood gas showed mixed acidosis and the baby was mechanically
ventilated. Chest X-ray showed left upper lobe opacity, and
intravenous antibiotics were started in view of neutrophilic
leucocytosis and positive C-reactive protein. The baby improved
gradually and weaned off from invasive to noninvasive mode of
ventilation; however, the baby continued to have intractable coughing,
persistent respiratory distress, chronic respiratory acidosis,
persistent opacity on the right side and high FiO 2
requirement. Computed tomography chest done showed consolidation in the
right upper lobe and apico-posterior segment of left upper and lower
lobes, and gastrograffin study showed no upper GI congenital anomaly.
The baby was then referred for further management to a pediatric surgeon
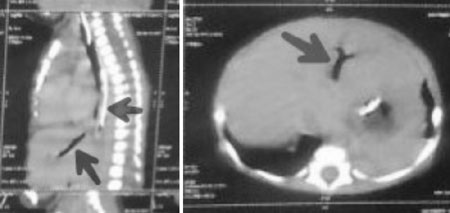
who performed bronchoscopy, which showed a third opening (Fig.
1) at the level of the carina. The opening was cannulated with an
X-ray positive catheter, and a fistula crossing the diaphragm and
communicating with the left hepatic duct was found. The diagnosis of
hepatobilliary fistula was made on bronchoscopy. A right posterolateral
thoracotomy was done, fistula was identified, and ligated at both the
ends and divided. Tracheobilliary fistula was about 6 cm long arising
from the carina between right and left osteum of main bronchi passed
through esophageal hiatus and inserted at the left side of bile duct.
The histopathology showed a tubular structure lined by squamous
epithelium at places by columnar epithelium, muscular wall shows few
mucous glands and cartilages with few mononuclear cells infiltrates.
Small muscular ventricular septal defect with Persistent Pulmonary
Hypertension was identified on color Doppler evaluation. The baby
improved after surgery and discharged home after 10 days of
hospitalization. The baby is now gaining weight, taking direct
breastfeeding well at 6 months of age.
 |
|
(a)
(b) |
|
Fig. 1 CECT chest reveals evidence of an
airfilled fistulous tract (arrows) between the carina and left
intrahepaticbilliary tract.
|
Discussion
Previous reports suggest that majority of
tracheobiliary fistula originate either from the right main bronchus
(42%) or carina (42%). In our patient, it was arising from the carina
between right and left osteum of main bronchi, passed through esophageal
hiatus, and inserted at the left side of bile duct. In our case, the
specimen obtained only from the proximal portion of the fistula, and
histological examination corresponded with previous reports.
The underlying pathogenesis of congenital fistula is
still not clear. However, two possible embryological mechanisms have
been suggested: (a) fusion of an anomalous bronchial bud with an
anomalous bile duct; (b) duplication of the upper
gastrointestinal tract [1].
The fistula was diagnosed at an early age (median
age, 32 d; range, 12 h to 6 y) in most cases (87%) [1-3]; only four
cases were diagnosed in adults [4-7]. Recurrent episodes of aspiration,
two episodes of extubation failure due to aspiration, and bilious
secretion present in the endotracheal tube gave us a clinical clue. The
most common presenting symptom in previously reported cases was
respiratory, including cough, dyspnea, cyanosis, bilious sputum, and
pulmonary infection. However, these symptoms are nonspecific, and other
pathologic conditions (including tracheoesophageal fistula,
gastroesophageal reflux, gastrointestinal obstruction, and aspiration
pneumonia) should be included in the differential diagnosis [8].
Bronchoscopy has been the most commonly used (52%)
method for diagnosis, followed by hepatobiliary scintigraphy (Tc99m HIDA
scan) and bronchography. Recently, two cases using multidetector CT with
multiplanar and 3D reformations to delineate the fistula have been
reported by Gunlemez, et al. [9]
The possibility of congenital anomalies of
respiratory tract should always be considered when evaluating a neonate
with persistent pneumonia and/or recurrent aspirations.
Contributors: All authors contributed equally in
patient care and manuscript preparation.
Funding: None; Competing Interest: None
stated.
References
1. Neuhauser EBD, Elkin M, Landing B. Congenital
direct communication between biliary system and respiratory tract. Am J
Dis Child. 1952;83:654-9.
2. Enjoji M, Watanabe H, Nakamura Y. Congenital
biliotracheal fistula with trifucation of the bronchi - A case
report. Ann Pedatr. 1963;200:321.
3. Stigol LC, Traversaro J, Trigo ER. Carinal
trifurcation with congenital tracheobiliary
fistula. Pediatrics. 1966;37: 89-91.
4. Weitzman JJ, Cohen SR, Woods LO, Chadwick DL.
Congenital bronchobiliary fistula. J Pediatr. 1968;73: 329-34.
5. Wagget J, Stool S, Bishop HC, Kurtz MB.
Congenital broncho-biliary fistula. J Pediatr Surg. 1970;5:566-9.
6. Sane SM, Sieber WK, Girdany BR. Congenital
bronchobiliary fistula. Surgery. 1971; 69:599-608.
7. Cuadros J, Aransay A, Nistral M, Monereo J.
Fistula traqueobiliar congenita. Ann Esp Pediatr. 1974;7:256-62.
8. Kalayoğlu M, Olcay I. Congenital bronchobiliary
fistula associated with esophageal atresia and tracheo-esophageal
fistula. J Pediatr Surg. 1976;11:463-4.
9. Chan YT, Ng WD, Mak WP, Kwong ML, Chow CB.
Congenital bronchobiliary fistula associated with biliary atresia. Br J
Surg. 1984;71:240-1.
|
|
|
 |
|

