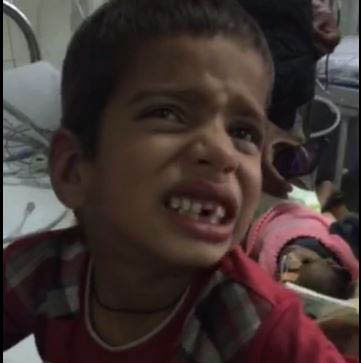
A 5-year-old, developmentally normal boy, presented
with sudden onset involuntary, persistent, deviation of neck towards
left, along with protrusion of tongue and hoarse cry for last 5 hours
(Fig. 1 and Webvideo 1). It was associated with
neck pain and inability to close the mouth. There was history of fever
for 1 day and he received four doses of oral paracetamol (15 mg/kg/dose)
over a period of 24 hours. Examination showed spasmodic torticollis to
left, persistent open jaw, and protruded tongue. Rest of the
neurological examination was essentially normal. Acute onset
drug-induced dystonic crisis was considered and child was treated with
single intravenous dose of chlorpheniramine (0.2 mg/kg); prompt response
was seen with subsidence of dystonic reaction within next 20 minutes. He
was observed for next 24 hours, and there was no recurrence of dystonic
crisis.
 |
|
Fig.1 Spasmodic torticollis to left.
|
Acute dystonic crisis can occur with antidepressants,
dopamine receptor blocking agents, antiemetics and anti-psychotics.
Drug-induced dystonic reaction commonly present as acute onset focal
dystonia characterized by torticolis, tongue protrusion and laryngeal
spasm. Paracetamol is a selective inhibitor of cyclooxygenase and in
usual doses it does not crosses the blood brain barrier. Higher doses
may activate central serotonergic pathways resulting in central
cholinergic and dopaminergic imbalance. Acute onset cervical dystonia is
very unusual with therapeutic dosage of paracetamol. Treatment include
immediate withdrawal of offending agent and anticholinergic agents like
chlorpheniramine, benzodiazepines or dopaminergic agonists. Acute
dystonic reaction is often misdiagnosed as seizure, encephalitis or
tetany. Eliciting a through history is important to avoid unnecessary
investigations and treatment for this potentially reversible condition.
|

