|
|
|
Indian Pediatr 2017;54: 966 -968 |
 |
Synovial Arteriovenous Malformation
Masquerading as Arthritis
|
|
Pooja Prakash Mallya and *Anand Prahalad Rao
From Pediatric Rheumatology Clinic; Vijaya Children’s Clinics, and *Manipal
Hospital and Indira Gandhi Institute of Child Health; Bengaluru,
Karnataka, India.
Correspondence to: Dr Pooja Prakash Mallya, H. no 46, 2nd Cross,
Panduranga Nagar, Bannerghatta Road, Bengaluru – 560076, Karnataka,
India.
Email:
[email protected]
Received: November 02, 2016;
Initial Review: February 08, 2017;
Accepted: August 31, 2017.
|
Background: Synovial arteriovenous malformation
is rare. Case characteristics: We present three children with
recurrent monoarthritis secondary to synovial arteriovenous
malformation. Outcome: Two children underwent excision of
arteriovenous malformation. Another child had diffuse arteriovenous
malformation, which was inoperable. Message: Synovial
arteriovenous malformations should be considered in the differential
diagnosis of monoarthritis, especially of the knee.
Keywords: Arthralgia, Misdiagnosis, Vascular malformation.
|
|
A
rteriovenous (AV) malformations are congenital
vascular lesions composed of a complex tangle of arteries and veins
connected by one or more fistulae. They are commonly seen in the brain
and the spine and rarely in joints. Patients with AV malformations
involving the joints may present with symptoms of joint pain, swelling (hemarthrosis)
and limitation of movement [1]. These lesions can lead to chronic
synovitis and progressive cartilage denudation leading to secondary
osteoarthritis. We present three children who presented with recurrent
knee joint swelling, and were diagnosed to have synovial AV
malformations.
Case Report
Case 1
A 4-year and 6-month old boy presented with recurrent
swelling of the right knee joint since the age of 2 years. The patient
on examination was noticed to have a purplish compressible swelling in
the sole of the right foot at the base of the great toe. There was no
history of similar complaints in the family members. Complete blood
count, coagulation studies (prothrombin time and activated partial
thromboplastin time) and erythrocyte sedimentation rate (ESR) were
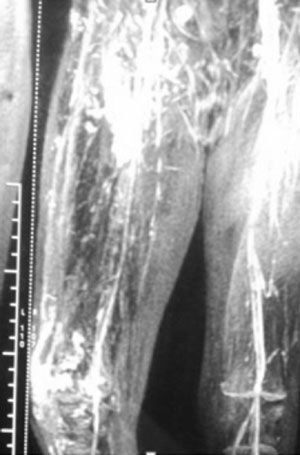
normal. Magnetic resonance imaging (MRI) of the affected limb revealed
the AV malformation involving the whole right lower limb (Fig.
1). The knee swelling was as a result of recurrent hemarthrosis
secondary to synovial AV malformation. As the AV malformation was
involving the whole lower limb (diffuse variety), it was not amenable to
treatment with either surgical excision or sclerotherapy/embolization.
The patient continues to be under observation, and persists to have
recurrent knee joint swelling. He continues to have periods of
immobilization and school absenteeism because of recurrent hemarthrosis.
 |
|
Fig.1 MRI showing hypertrophy of the
right lower limb with underlying AV malformation (dilated
vessels infiltrating the subcutaneous fat,muscles, patella and
knee joint).
|
Case 2
A 5-year-old boy presented with recurrent right knee
joint pain and swelling from infancy, which was brought about by trivial
trauma. On examination, he had swelling and tenderness of the right knee
joint. Complete blood count, coagulation studies and ESR were normal.
X-ray of the right knee joint showed early erosive changes. MRI of
the right knee joint revealed a synovial AV malformation. He underwent
excision of the AV malformation. Histopathological examination was
suggestive of hemangioma. He had complete resolution of the symptoms for
the first 6 months post-surgery. Subsequently he was lost to follow-up.
Case 3
A 3-year and 5-month old boy presented with recurrent
episodes of left knee pain and swelling that had been present for the
last 2 years. He had complaints of early morning stiffness of the left
knee joint. On examination, he had swelling and tenderness of the left
knee joint. He was diagnosed as oligoarticular Juvenile idiopathic
arthritis and was treated with methotrexate and folic acid. He had a
persistent microcytic, hypochromic anemia, which did not improve
significantly with iron supplementation. In view of recurrent
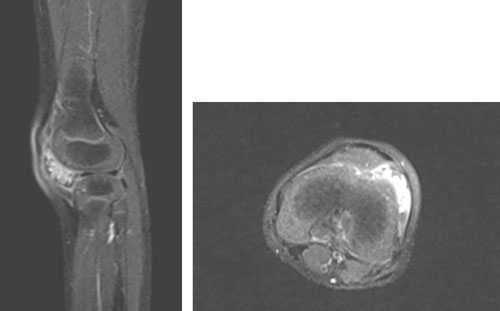
monoarthritis with lack of response to methotrexate and persistent
anemia, he was subjected to MRI, which revealed heterogeneously
hyper-intense lesion on T2-weighted image in the anterolateral aspect of
the left knee joint with post-contrast non-homogenous enhancement with
small branches of popliteal artery supplying the lesion (Fig.
2). The child underwent open synovectomy with en-bloc
excision of the AV malformation. Biopsy was suggestive of hemangioma.
Four months post-surgery, he was doing well.
 |
|
Fig. 2 Sagittal and coronal
T2-weighted MR image showing a heterogenous mass hyper intense
lesion in the anterolateral aspect of the left knee joint with
post contrast non-homogenous enhancement.
|
Discussion
Synovial AV malformations are rare in children [2].
They are usually congenital malformations but are often diagnosed later
in life. They can be localized or diffuse in nature. Intra-articular AV
malformations can arise from any synovial surface. Possibility of
synovial AV malformations should be considered in patients having
recurrent painful hemarthoses with normal coagulation parameters [3].
Synovial AV malformations commonly tend to involve
the knee joint, but have also been reported in the elbow, wrist, tempo-mandibular
joint and ankle [4]. The knee joint was involved in all our patients.
The usual symptoms brought about by these synovial AV malformations
include recurrent joint pain, joint swelling – either because of the AV
malformation or because of the recurrent hemarthrosis caused by minimal
trauma – and limitation of movement. Kassabach Merrit syndrome is a rare
association with this type of AV malformation [5]. Synovial AV
malformations cause premature destructive arthropathy secondary to
repeated hemarthrosis. The differential diagnoses that need to be
considered are pigmented villonodular synovitis, tuberculous
monoarthritis, synovial sarcoma, other arthritis/arthropathies (Juvenile
idiopathic arthritis, hemophilic arthropathy, synovial
osteochondromatosis) – usually distinguished clinically or on MRI [6].
Radiographs usually reveal a soft tissue swelling of
the joint. Rarely phleboliths are seen in the joint. MRI is the
investigation of choice for diagnosis and planning of the management
strategies in this condition. MRI typically shows isointense or
hypointense lesion in T1-weighted images and hyperintense in T2-weighted
images [7]. The diagnosis was unmarked by MRI in all our patients. Whole
body MRI to rule out AV malformations in other organs could not be done
in view of cost-constraints.
Early surgical excision is indicated to prevent joint
damage. Arthroscopic excision is done when the hemangioma is well
circumscribed and pedunculated. Open excision is the treatment modality
of choice for diffuse hemangioma, but carries a higher risk of
recurrence [8]. Angiography defines the size, location of the lesion and
can identify the feeder vessels associated with the AV malformation.
High flow lesions require trans-arterial embolization whereas
percutaneous sclerotherapy is typically used for low-flow lesions [8].
These are usually performed in cases of associated cutaneous hemangioma
or abnormal varicosity because these findings are indicative of a more
general vascular abnormality [9].
We conclude that pediatricians should consider
synovial AV malformations in the differential diagnosis of recurrent
joint swelling affecting a single joint.
Contributors: PPM reviewed the literature and
drafted the manuscript. APR supervised and critically revised the
manuscript.
Funding: None; Competing interest: None
stated.
References
1. Herdman G, Dussa CU, Watura R, Cobby M. Intra-articular
arteriovenous malformation of the knee. Eur J Orthop Surg Traumatol.
2005;15:66-68.
2. Bavikar RR, Deshmukh SD, Khadilkar M. Knee: an
unusual site for arteriovenous malformation. Curr Orthop Pract.
2013;24:353-4.
3. Winzenberg T, Ma D, Taplin P, Parker A, Jones G.
Synovial hemangioma of the knee: a case report. Clin Rheumatol.
2006;25:753-5.
4. Greenspan A, Azouz EM, Matthews J2nd, Decarie JC.
Synovial hemangioma: imaging features in eight histologically proven
cases, review of the literature, and differential diagnosis. Skeletal
Radiol. 1995;24:583-90.
5. Elsayes KM, Menias CO, Dillman JR, Platt JF,
Willatt JM, Heiken JP. Vascular Malformation and Hemangiomatosis
Syndromes: Spectrum of Imaging Manifestations. Am J Roentgenol. 2008;190:1291-9.
6. Anosheh VA, Shahin Z, Josef H, Monika H, Peter R.
Synovial hemangioma of the knee joint in a 12-year-old boy: A case
report. J Med Case Rep. 2010;4:105-8.
7. Vakil-Adli A, Zandieh S, Hochreiter J, Huber M,
Ritschl P. Peripheral vascular malformations: imaging, treatment
approaches, and therapeutic issues. Radiographics. 2005;25:159-71.
8. Akgun I, Kesmezacar H, Ogut T, Dervisoglu S.
Intraarticular hemangioma of the knee. Arthroscopy. 2003;19:1-8.
9. Durieux S, Brugieres P, Voisin MC, Goutallier D,
Larget-Piet B, Chevalier X. Radiologic vignette. Arthritis Rheum.
1995;38:559-64.
|
|
|
 |
|

