|
|
|
Indian Pediatr 2017;54: 963 -965 |
 |
Paint in the Pipe: An Unusual Foreign Body
|
|
Neha Garg, *Natasha
Gupta, Dheeraj Shah and Piyush Gupta
From Departments of Pediatrics and *Radiology,
University College of Medical Sciences (University of Delhi) and GTB
Hospital, Dilshad Garden, Delhi, India.
Correspondence to: Dr Dheeraj Shah, Professor,
Department of Pediatrics, University College of Medical Sciences and GTB
Hospital, Dilshad Garden, Delhi 110 095, India.
Email: [email protected]
Received: February 10, 2017;
Initial Review: March 28, 2017;
Accepted: May 24, 2017.
|
Background: Foreign bodies in the airway can be a
diagnostic and therapeutic challenge. Case characteristics:
30-month-old girl with complaints of noisy and fast breathing following
fall over a pile of sand. Sand was suctioned out by direct bronchoscopy.
The child improved initially but condition worsened in next four days
with marked stridor and wheeze. Observation: Imaging revealed
elongated sharp radiodense opacity in the cervical region, suggestive of
foreign body. At repeat bronchoscopy, paint material was removed
from the airway, leading to recovery Message: Paint
material mixed in the sand can adhere to the walls of the airway, and
cause persistent symptoms of obstruction.
Keywords: Airway foreign body, Bronchoscopy, Stridor.
|
|
T
racheobronchial foreign body aspiration in
children aged between 1 to 3 years is a common medical emergency [1-4].
A long list of commonly aspirated objects amongst children is available
[5]; though, aspiration of sand, gravel, or dirt is rare but potentially
lethal. Majority of cases of sand aspiration reported so far share the
common mechanism of either being buried accidentally under sand, dirt,
or gravel masses at construction sites, as the result of the collapse of
sand tunnels, sand castles and sand piles or during drowning [6]. We
report a child with sand aspiration where symptoms persisted after
removal of sand through bronchoscopy.
Case Report
A 30-month-old girl was brought by her parents to our
hospital with complaints of sudden onset of noisy and difficult
breathing for two days that started soon after accidentally falling over
a sand pile while playing. There was no history of cough, fever,
rhinorrhea, nasal congestion, or history of similar illness in past.
Examination revealed inspiratory stridor and wheeze. Breath sounds were
heard equally on both sides. Systemic examination was normal. Suspecting
sand deposits as possible foreign body in airway, the child was taken up
for emergency bronchoscopy. Sand particles were seen during bronchoscopy,
and were suctioned out from trachea. Post-bronchoscopy, stridor and
wheeze decreased; and the child was discharged after 24 hours. Four days
later, child reported back with complaints of progressively increasing
noisy breathing following initial improvement. There was no associated
history of cough, fever and cold. Examination revealed stridor and
wheeze with equal breath sounds. Patient was treated with steroids and
antibiotics considering the possibility of post-bronchoscopy edema.
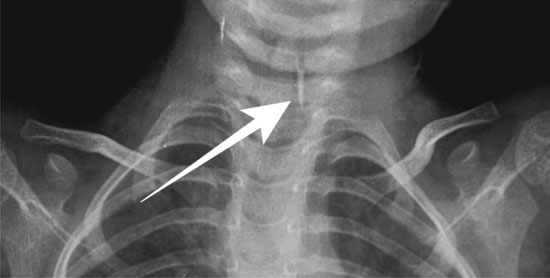
Frontal radiograph of the chest showed a well-defined, elongated pointed
radio-opaque shadow in the airway at the level of C6-7 vertebrae,
suggestive of impacted foreign body in the airway (Fig. 1).
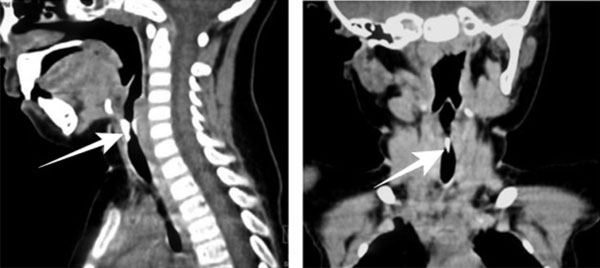
A Contract-enhanced Computed tomography (CECT) of neck and thorax was
planned in view of persistent symptoms and radio-opaque shadow on X-ray,
which revealed an elongated structure isodense to bone, of an unusual
shape with inferior sharp margin and superior rounded margin, appearing
fixed to the anterior and posterior walls of airway straddling across
its lumen, causing significant luminal narrowing, and lodged just below
the expected location of true cords (Fig. 2a and 2b).
 |
|
Fig.1. X-Ray Chest- Frontal view
shows elongated pointed foreign body of metallic density (arrow)
in the airway at C6-C7 level.
|
 |
|
(a) |
(b) |
|
Fig. 2 Conrast enhanced computed
tomogram of the cervical Sagittal (a), and Coronal (b)
multiplanar reconstruction of images reveal high density
elongated structure with sharp inferior tip lodged in airway
(thick arrow) straddling across its lumen, causing luminal
narrowing (arrowheads).
|
Repeat bronchoscopy revealed greenish deposits
of paint just below the glottis and in right main bronchus. Those 1-5 mm
paint scrapings were removed using forceps. The aspirated material could
not be sent for chemical analysis. Post-bronchoscopy, stridor and wheeze
settled. Antibiotics and supportive care were continued for 48 hours.
Child improved and on follow-up after one week, child was stable and
free of symptoms.
Discussion
Airway aspiration of sand presenting as respiratory
distress is rare. Most of the accidental aspirations, notably those of
children being buried under sand masses, improve after successful
bronchoscopy treatment [6]. Majority do not require repeat bronchoscopy.
Sand is ubiquitously present and usually contains
large or small sedimentary particles known as gravel and silt,
respectively. It is usually composed of aluminium silicate, silicon
dioxide and calcium carbonate as major components. The percentage of
calcium carbonate present directly increases the radio opaque property
of the aspirated material [7]. At times it may mixed with other things
like paint scrapings, small paper pieces and plastic material. Sand with
thick bronchial secretions may get adhered to the mucosa, and can form
casts in the airway due to its own nature and the mixed substances. Some
particles can be larger than the diameter of suction catheter, and may
cause continuous plugging. Also, the sand particles can be too heavy to
be lavaged easily and may require tedious, repeated manual extraction
[8].
In this child, we assume that the paint material
present in the sand adhered to the wall of the glottis, and could not be
suctioned out during first bronchoscopy. The persistence of stridor and
wheeze following emergency bronchoscopy was initially attributed to
post-broncho-scopy edema as it is a well-known complication of
bronchoscopy [9]. However, persistence of symptoms and radio-opaque
sharp shadow on X-ray prompted us to evaluate the child for any
retained foreign body, which in this case turned out to be solidified
paint material.
The oil-based paint is composed of base, vehicle,
pigment, thinner and dryer. Except for the vehicle and thinner, other
three components are metallic. Commonly used bases are zinc oxide, iron
oxide and metallic powder (Aluminium, Copper, and Bromium), which make
the film harder. Calcium carbonate, mica, silicas, and talcs are used as
pigment that gives the paint its colour. Organic salts of iron, zinc,
lead, manganese and calcium helps in drying [10]. These radiopaque
metallic components of paint made the findings evident on radiograph and
CT scan in our case. Also being metallic in composition, these paint
scrapings were capable of initiating an inflammatory response, which
probably led to previous worsening of symptoms compared to the size of
foreign material.
Irregular foreign bodies or orientation in sagittal
plane may produce only partial obstruction allowing adequate air
movement around the obstruction. Later worsening of symptoms in this
child can be explained by the fact that air passage realigned the paint
scrapings to anterior and posterior walls causing worsening of
obstruction and stridor. We could not trace any other report of paint
material being aspirated by the children and presenting with obstructive
symptoms.
We suggest the need of follow-up and re-evaluation in
case of persistence of symptoms and radio-imaging before and after
bronchoscopy in cases of sand aspiration. Cases of sand aspiration
should be viewed with caution as there could be other material mixed in
it.
Contributors: Neha Garg, DS, PG: were involved in
management of the patient; Natasha Gupta: was involved in the diagnostic
work-up of the patient; The first draft of manuscript was prepared by
Neha Garg, and was revised after critical outputs from DS, PG and
Natasha Gupta. All authors approved the final version of the manuscript.
Funding: None; Competing Interests: None
stated
References
1. Bittencourt PF, Camargos PA, Scheinmann P, De Blic
J. Foreign body aspiration: clinical, radiological findings and factors
associated with its late removal. Int J Pediatr Otorhinolaryngol.
2006;70:879-84.
2. Cohen S, Avital A, Godfrey S, Gross M, Kerem E,
Springer C. Suspected foreign body inhalation in children: what are the
indications for bronchoscopy? J Pediatr. 2009;155:276-80.
3. Metrangolo S, Monetti C, Meneghini L, Zadra N,
Giusti F. Eight years experience with foreign-body aspiration in
children: what is really important for a timely diagnosis? J Pediatr
Surg. 1999;34:1229-31
4. Tan HK, Brown K, McGill T, Kenna MA, Lund DP,
Healy GB. Airway foreign bodies [FB]: a 10-year review. Int J Pediatr
Otorhinolaryngol. 2000;56:91-9.
5. Yetim TD, Bayarogullary H, Arıca V, Akcora B,
Aryca SG, Tutanc M. Foreign body aspiration in children; Analysis of 42
cases. J Pulmon Resp Med. 2012;2:121
6. Kettner M, Ramsthaler F, Horlebein B, Schmidt PH.
Fatal outcome of a sand aspiration. Int J Legal Med. 2008;122:499-502.
7. Arun Babu T, Ananthakrishnan S. Unusual
presentation of sand aspiration in a 14-mo-old child. Indian J Pediatr.
2013;80:786-8.
8. Choy IO, Idowu O.Sand aspiration: a case report. J
Pediatr Surg. 1996;31:1448-50.
9. Ciftci AO, Bingöl-Koloğlu M, Senocak ME, Tanyel
FC, Büyükpamukçu N. Bronchoscopy for evaluation of foreign body
aspiration in children. J Pediatr Surg. 2003;38:1170-6.
10. Civil Engineering Portal of Lectures & Training
Material. Composition of Paints. Available from:
http://www.aboutcivil.org/Composition%20of%20paints.html. Accessed
December 21, 2016.
|
|
|
 |
|

