|
|
|
Indian Pediatr 2016;53: 1028-1029 |
 |
Pediatric Multiple Sclerosis
|
|
*Ajay Kumar and Vyom Aggarwal
Department of Pediatrics, Tirath Ram Shah Hospital,
Delhi, India.
Email:
[email protected]
|
|
An 11-year-old girl presented to us with history of sudden diminution of
vision in the right eye. There was no associated history of altered
sensorium, fever, headache, vomiting, rashes or head injury. She also
had a history of feeling of decreased sensation in left arm 4 weeks ago,
which recovered completely and spontaneously within 2 weeks. There was
decreased visual acuity in the right eye, with evidence of optic atrophy
on fundoscopy. The Visual Evoked Potential (VEP) test revealed increased
latency and decreased amplitude in the right eye.
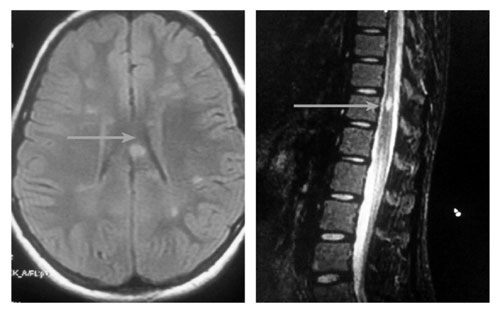
Magnetic resonance imaging (MRI) of the brain showed
multiple lesions involving white matter in bilateral periventricular,
bilateral fronto-parietal subcortical and right temporal subcortical
regions. On contrast enhanced cerebral MRI, few enhancing lesions were
located in the corpus callosum, periventricular and bilateral frontal
regions (Fig. 1). MRI spinal cord showed T2 hyperintense
lesions in cord at C2, C4 and D12 vertebral levels. The cerebrospinal
fluid analysis revealed normal cytology and biochemistry, with no
oligoclonal band. Anti NMO antibodies were negative. According to Polman
(2010 revised Mcdonald criteria) [1], diagnosis of multiple sclerosis
(MS) was made and pulse corticosteroid therapy with methylprednisolone
was started with strict monitoring of vital and laboratory parameters.
The vision improved within 24 hours of initiation of therapy and the
girl was discharged on oral steroids, after 3 days of intravenous
therapy.
 |
|
Fig.1 MRI Brain and MRI Spinal cord
showing lesions consistent with multiple sclerosis.
|
Multiple sclerosis (MS) is a chronic demyelinating
disorder of brain, spinal cord and optic nerves characterized by a
relapsing-remitting course of neurologic events, separated in time and
space, without encephalopathy, thus distinguishing it from acute
disseminated encephalomyelitis [2]. Oligoclonal band in cerebrospinal
fluid is considered to be a useful aid in diagnosis, but may be absent
in up to 60% of confirmed pediatric cases. Its incidence is reported to
be about 5.68/100000 per year, and the pediatric population accounts for
about 2% to 5% of all MS cases [3]. Intravenous methyl prednisone is the
preferred therapy in freshly diagnosed cases. Currently available
first-line disease modifying therapies for adults, including
interferon â and glatiramer acetate, have not been approved by the US
FDA for the treatment of children with MS.
References
1. Polman CH, Reingold SC, Banwell B,
Clanet M, Cohen JA, Filippi M, et al. Diagnostic criteria for
multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol.
2011;69:292-302.
2. Dale RC, Brilot F, Banwell B. Pediatric central
nervous system inflammatory demyelination: acute disseminated
encephalomyelitis, clinically isolated syndromes, neuromyelitis optica
and multiple sclerosis. Curr Opin Neurol. 2009;22:233-40.
3. Ghezzi A, Deplano V, Faroni J, Grasso MG, Liguori M, Marrosu G,
et al. Multiple sclerosis in childhood: Clinical features of 149
cases. Mult Scler. 1997;3:43-6.
|
|
|
 |
|

