Formative assessment has a major influence on
learning [1]. The educational utility of a summative or year-end
examination is limited since it usually involves a single encounter
with assessment of a limited number of competencies, mostly
knowledge-based, with no opportunity for feedback and improvement.
Internal assessment provides a very useful opportunity to not only
test acquisition of knowledge but also provide feedback to make
learning better.
The strengths of internal assessment (IA) are
three-fold. One, there is an opportunity to provide timely
corrective feedback to students. Feedback is recognized as the
single-most effective tool to promote learning [2].Two, IA can be
designed to test a range of competencies, such as, skill in
performing routine clinical procedures (giving injections, suturing
wounds, performing intubation etc.), professionalism, ethics,
communication, and interpersonal skills, which are hardly assessed
in the final examinations [3]. Three, the continuous nature of this
assessment throughout the training period has the potential to steer
the students’ learning in the desired direction over time. The focus
is on the process, as much as on the final product of learning.
The concept of IA is not new. The University
Grants Commission [4] recommends that we need to "… move to a system
which emphasizes continuous internal assessment and reduces
dependence on external examinations to a reasonable extent."
Similarly, the National Accreditation and Assessment Council (NAAC)
encourages the use of internal assessment to guide learning [5].
The draft of the 2012 revised Regulations on
Graduate Medical Education (GME) released by the Medical Council of
India (MCI) stipulates that undergraduate students should have
passed in their IA to be eligible to appear in the final university
examinations [6]. The recommendation is for IA to be based on
day-to-day records. Also, regular assessments conducted throughout
the course shall relate to assignments, preparation for seminars,
clinical case presentations, participation in community health care,
proficiency and skills required for small research projects etc.
Further, electives and skills should be assessed as part of internal
assessment [6].
Problems with Internal Assessment in India
Despite its obvious strengths, internal
assessment has not been used to its full potential in India. Often
trivialized as a replica of the final examination, IA is restricted
only to theory and practical tests, while its potential to test
other competencies is seldom exploited. The major issues with
internal assessment in India are: improper implementation, lack of
faculty training, misuse or abuse, lack of acceptability among all
stakeholders and perceived lack of reliability [7].
Improper implementations: Implementation has
a strong bearing on any assessment and its educational utility. The
earlier 1997 guidelines [8] did not carry any mention of how the IA
was to be implemented. Institutions were left to design their own
plan of IA leading to considerable variation in the methods of
assessment and the competencies assessed. Practical guidelines have
not been provided for implementation of IA in the 2012 revised
regulations on GME [6] either, giving rise to a sense of déjà vu.
Lack of faculty training: Faculty
development is pre-requisite to proper implementation of any
educational method. Lack of training is often the reason for poor
implementation, lack of transparency, and inadequate or no provision
of feedback to students. By not providing timely and appropriate
feedback, the biggest strength of internal assessment is nullified.
When teachers do not give competencies such as communication skills,
professionalism, ethics, interpersonal skills, ability to work in a
team etc. enough weightage in the internal assessment due to the
fear that these cannot be precisely measured, they indirectly convey
to students that these qualities are not important in medicine.
While the faculty do gain experience of teaching and research, there
is no opportunity for them to get a hands-on experience on student
assessment.
Misuse/Abuse: IA is often misused as
an examination without external controls [9-10].The 2012 draft
regulations [6] have proposed some variations from the 1997
regulations [8]. Marks of IA are no longer to be added to the final
scores. Although not expressly stated, fear of abuse of IA to
inflate marks seems to have prompted this change. However, this
opens new opportunities to use IA to assess competencies hitherto
left un-assessed.
Lack of acceptability: The issues that
lower the acceptability of IA from all its stakeholders are:
variability in marking by institutions, too much ‘power’ bestowed to
single individuals (often departmental heads), too much weightage to
single tests and a perceived lack of reliability. Reliability (also
sometimes described as reproducibility) is commonly seen as
‘consistency of marking’. Here, it may be pertinent to clarify that
reliability should be seen as consistency or reproducibility of
student performance rather than consistency of marking by examiners.
Assessing a student in one clinical situation poorly predicts his
performance in another clinical situation. Also, it is uncertain
that a physician will encounter the same conditions in actual
practice under which he was assessed. Therefore, if reliability has
to contribute towards prediction of student’s future performance in
real situations, the true meaning of reliability should be
‘consistency of performance’ rather than ‘consistency of scoring’
[11]. Marker variability in IA is often cited as a reason for lack
of reliability. Research has consistently shown that increasing the
number of assessors and increasing the sample of the content being
assessed improves reliability [12]. Even with rather subjective
assessments, having different assessors for different parts of a
test can neutralize an incompetent/ biased assessor’s influence
[13]. By increasing the number of clinical situations in which a
student is assessed, the reliability of the assessment can be
improved more than by merely making more objective tests.
The utility of any assessment is dependent upon
its validity, reliability, acceptability, feasibility and
educational impact [14]. Although each one of these attributes is
important, there is always some trade-off between them. For example,
an assessment which is apparently low on reliability can still be
useful by virtue for its positive educational impact [13]. Where
combinations of different assessments alleviate draw-backs of
individual methods, use of the programmatic approach to assessment
is advocated, thereby rendering the total more than the sum of its
parts [15].
When properly implemented, IA scores over the
year-end examination in terms of its validity, reliability
(consistency of performance), feasibility and educational impact
[7]. To ensure that students are not denied the benefit of this
extremely useful modality, efforts need to be made to improve its
implementation and acceptability.
In this paper, we propose a model for internal
assessment, which tries to overcome some of the issues that teachers
and students face. We call it the ‘in-training assessment
(ITA) program’ as it reflects the philosophy and intent of
this assessment better. The ITA is designed to not only test
knowledge and skills, but also provide an opportunity to assess
competencies which are not assessable by conventional year-end
examinations. The purpose of ITA is to provide feedback to students
and teachers, and to improve student learning. It is proposed to be
a longitudinal program spread throughout the MBBS training. ITA is
expected to be complementary to the end-of-training assessment (ETA)
carried out by the affiliating Universities to test for attainment
of intended competencies.
The Proposed Quarter Model
The salient features of this model are outlined
in the Box 1.
|
Box 1: The Quarter Model of
In-training Assessment
1. One assessment to be conducted at
least every quarter.
2. No teacher to contribute more than a
quarter (25%) of the marks for any student.
3. No single tool to contribute more than
a quarter (25%) of the marks.
4. No single assessment to contribute
more than a quarter (25%) of the total marks.
|
Format: We propose that students be
periodically assessed during the course of their training by the
faculty of their parent institutes. Passing separately in ITA and
ETA, in both theory and practical/clinical components should be
mandatory. As proposed in the Graduate Medical Education Regulations
2012 [6], while passing in ITA will be an eligibility criterion for
appearing in the University examinations, marks obtained in ITA will
not be added to the marks obtained in ETA. The scores can be
converted to grades using a 7-point scale (using absolute grading
criteria) and shown separately on the mark-sheet issued by
Universities.
Organization and Conduct: To allow
greater spread of marks, each subject may be assessed out of a
maximum of 100 marks (50% for theory and 50% for practical/clinical
component) in the ITA. ITA should make use of a number of assessment
tools. For theory: essay questions, short answer questions (SAQ),
multiple choice questions (MCQ), extended matching questions and
oral examinations should be used. For practical/clinical assessment:
experiments, long cases, short cases, spots, objective structured
practical/clinical examinations (OSPE/OSCE), mini-clinical
evaluation exercise (mini-CEX) and objective structured long
examination record (OSLER) should be used. Viva in
practical/clinical assessment should focus on the experiments
actually performed or cases actually seen rather than being a
general viva. Colleges can add more tools depending on the local
expertise available.
The planning and assessment for ITA should
involve all teachers of each department to ensure that no single
teacher contributes more than 25% of the marks to the total marks
and no single assessment tool contributes more than 25% marks to the
total ITA. For this purpose, teachers would mean all those working
as tutors/ senior residents and upwards.
The proportion of 25% marks should be calculated
from the assessments spread over the entire year. For example, the
departments should be at liberty to have four assessments with one
having only essay type questions, another having only MCQs, the
third having only oral examination and a fourth one with a mix of
all. Or they could have four assessments with a mix of essays, SAQs,
MCQs and oral examinations. The same applies to practical/clinical
examinations. However, for subjects like radiology, TB and chest,
dermatology, casualty and dentistry, each teacher and each tool may
contribute 50% to the assessment in that subject. In effect, it
means that to maintain the 25% limit, at least four teachers and
four different assessment tools should be used for ITA. For subjects
with the 50% limit, at least two teachers and two tools will be
required.
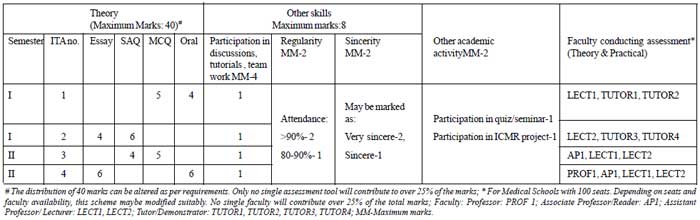
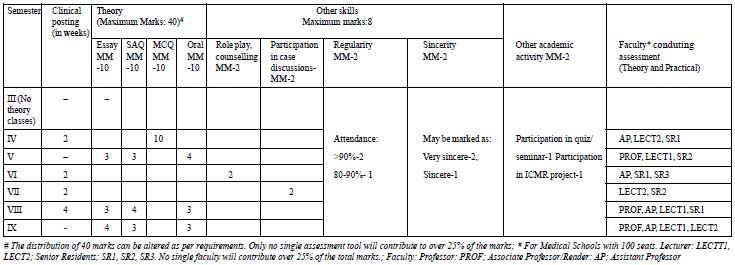
The marks for ITA in each subject is shown in
Table I. To illustrate its working, two examples, one
from a pre-clinical (Physiology) and another from a clinical
(Pediatrics) department are provided (Fig. 1 and 2).
TABLE I Division of Marks
|
Theory (Max. marks 50) |
|
Practical/clinical (Max. marks 50) |
|
|
Knowledge tests: using multiple tools* |
40 |
Practical and clinical skills (including communication |
35 |
|
|
skills, bedside manners): using multiple tools*
|
|
|
Preparation, participation, regularity, sincerity |
8 |
Regularity, sincerity, professionalism, presentation |
8 |
|
Other academic activities: quiz, seminar etc. |
2 |
Log books |
5 |
|
|
ICMR or other projects, community work, etc. |
2 |
The given sample formats have been drafted using
the prescribed number of teaching staff for an institution admitting
a batch of 100 students in a year. Utilization of end-of-posting
assessment for the practical component of ITA in clinical subjects
may contribute towards time efficiency of the ITA program by using
same assessments for formative as well as summative purposes.
 |
|
Fig.1 Physiology : Sample format for ITA.
|
As Fig.2 shows, ITA is
proportionately divided over the phases for subjects that are taught
over different semesters. For subjects that include other allied
subjects (e.g. Medicine includes Dermatology, Psychiatry
etc.), a proportion of ITA is allocated to allied subjects based on
the teaching time allotted. Students would need to secure passing
marks (>50%) in theory and practical separately for allied subjects
also.
 |
|
Fig 2 Pediatrics: Sample format for ITA - Theory
(maximum mark 50); Minimum 4 ITAs over entire course.
|
All results should be declared within two weeks
of the assessment. Students should sign on the result sheet in token
of having seen the results. The results should also be uploaded on
the college website within two weeks of being put up on the notice
board. Students who do not pass in any of the assessments should
have the opportunity to appear for it again – however, any repeat
assessment should not be conducted earlier than two weeks of the
last to allow students to meaningfully make good their deficiencies.
Only one additional assessment may be provided to make good the
deficiency. If a student is unable to score 50% even after an
additional assessment, he should repeat the course/posting and
appear for University examinations 6 months later.
Teachers should provide feedback to students
regarding their performance. A group feedback session should be
organized within a week after declaration of results. However, for
persistently low achieving students, one-to-one feedback sessions
may be organized.
To use the power of assessment meaningfully for
better learning and to ensure stability in assessments, all colleges
should appoint a Chief Coordinator. All the teaching departments
should also appoint a teacher as coordinator to plan and organize
ITA. Departments should coordinate among themselves and with the
Chief Coordinator to ensure that students do not have assessment in
more than one subject during the same week. As far as possible, all
ITAs should be scheduled on Monday mornings so that students get the
weekend to prepare and do not miss classes. For clinical subjects,
the practical component of the ITAs should be scheduled at the end
of clinical postings. The minimum number of ITAs for each subject
should be specified in the beginning of the term. The plan and
tentative dates of assessment should be put up on the notice board
within the first month of starting that phase of training. The ITA
plan of each department should be developed as a standard operating
protocol (SOP) document, approved by the Curriculum/ Assessment
committee of the college and reviewed (and revised if required)
annually. This document should be made available to the students at
the beginning of each phase.
Record keeping: It is important to
maintain a good record of performance in ITA to ensure credibility.
Students should have access to this record and should sign it every
three months. A sample format for record keeping has previously been
published [16].
Faculty development: Unless both the
assessors and students understand the purpose of this exercise, this
powerful tool will continue to be trivialized and acceptance will
remain suboptimal. Success of this model will require training
faculty in use of multiple assessment tools. Currently, faculty
development is carried out through the basic course workshops on
medical education; this needs to be scaled up for capacity building
of medical teachers. It is also imperative that the students be
sensitized to the ITA program for MBBS during the proposed
foundation course (the first two months before Phase I of MBBS).
Discussion
The quarter model addresses several commonly
leveled criticisms against internal assessment. The strength of ITA
is expected to be realistic in its continuous nature and in the fact
that it is based on longitudinal observations in authentic settings.
Provision of feedback not only allows for mid-course correction of
the learner’s trajectory [17] but also reinforces their strong
points.
Medical competence is an integrated whole and not
the sum of separate entities. No single instrument will ever be able
to provide all the information for a comprehensive evaluation of
competence [18]. Single assessments, howsoever well planned, are
flawed [15]. By including assessment in various settings and by use
of multiple tools in this model, the intention is to increase the
sampling and to make more well-informed and defensible judgments of
students’ abilities. Use of multiple examiners is expected to help
reduce the examiner biases involved in the process of assessment,
and also minimize misuse of power.
Understandably, this model may demand more effort
and work from the faculty members. However, we feel that that the
added benefits of this model would be a better distribution of
student assessment tasks within the department and also an
opportunity for the tutors/senior residents to be trained in
assessment methods under supervision. It must be reiterated here
that assessment requires as much preparation, planning, patience and
effort that research or teaching does. Assessment has been taken
rather casually for far too long and at least semi-prescriptive
models of ITA based on educational principles are a need of the day.
Ignoring educational principles while assessing students, merely
because it results in more work, seriously compromises the utility
and sanctity of assessment.
Black and Wiliam [19] state that any strategy to
improve learning through formative assessment should include: clear
goals, design of appropriate learning and assessment tasks,
communication of assessment criteria and provision of good quality
feedback. Students must be able to assess their progress towards
their learning goals [17]. The quarter model largely takes into
account all these elements. Our model gives a broad overview of what
is and what is not being measured. It also balances the content and
counteracts the tendency to measure only those elements which are
easy to measure. By involving students early in the process,
informing them of the criteria by which they will be judged, the
assessment schedules and most importantly, giving them feedback on
their learning, the model is expected to provide them an opportunity
to improve performance. The display of ITA grades alongside the ETA
marks is expected to demonstrate the consistency of student
performance and prevent manipulation of marks.
This model has been conceptualized using accepted
theories of learning and assessment. Multiple tests on multiple
content areas by multiple examiners using multiple tools in multiple
settings in the quarter model will improve the reliability and
validity of internal assessment, and thereby improve its
acceptability among all stakeholders.
1. Rushton A. Formative assessment: a key to deep
learning. Med Teacher. 2005; 27:509-13.
2. Hattie JA. Identifying the salient facets of a
model of student learning: A synthesis of meta-analyses. Int J Educ
Res. 1987;11:187–212.
3. Singh T, Natu MV. Examination reforms at the
grassroots: Teacher as the change agent. Indian Pediatr.
1997;34:1015-9.
4. University Grants Commission. Action Plan for
Academic and Administrative Reforms. New Delhi. Available from:
URL:http://ugc.ac.in/policy/cmlette2302r09.pdf. Accessed 24 June,
2012.
5. National Accreditation and Assessment Council.
Best Practice Series-6. Curricular Aspects. Available from: URL:
http://naac.gov.in/sites/naac.gov.in/files/Best%20
Practises%20in%20Curricular%20Aspects.pdf. Accessed 24 June, 2012.
6. Medical Council of India Regulations on
Graduate Medical Education 2012. Available from: URL:
http://www.mciindia.org/tools/announcement/Revised_ GME_2012.pdf.
Accessed 24 June, 2012.
7. Singh T, Anshu. Internal assessment revisited.
Natl Med J India. 2009;22:82-4.
8. Medical Council of India Regulations on
Graduate Medical Education 1997. Available from: URL:
http://www.mciindia.org/RulesandRegulations/Graduate
MedicalEducationRegulations1997.aspx. Accessed 24 June, 2012.
9. Gitanjali B. Academic dishonesty in Indian
medical colleges. J Postgrad Med. 2004;50:281-4.
10. RGUHS does it again, alters MBBS marks.
Available from: URL:
http://articles.timesofindia.indiatimes.com/2006-04-25/bangalore/27804396_1_internal-assessment-rguhs-medical-colleges.
Accessed 24 June, 2012.
11. Feldt LS, Brennan RL. Reliability. In:
Linn Rl, editor. Educational Measurement. 3rd edn. New York:
Macmillan; 1989.p. 105-46.
12. van der Vleuten CPM, Scherpbier AJJA, Dolmans
DHJM, Schuwirth LWT, Verwijnen GM, Wolfhagen HAP. Clerkship
assessment assessed. Med Teacher. 2000;22:592-600.
13. van der Vleuten CPM, Norman GR, De Graaff E.
Pitfalls in the pursuit of objectivity: Issues of reliability.
Medical Education. 1991;25:110-8.
14. van der Vleuten CPM, Schuwirth LWT. Assessing
professional competence: from methods to programmes. Medical
Education. 2005;39:309-17.
15. van der Vleuten CPM, Schuwirth LWT, Driessem
EW, Dijkstra J, Tigelaar D, Baartman LKJ, et al. A model for
programmatic assessment fit for purpose. Medical Teacher.
2012;34:205-14.
16. Singh T, Gupta P, Singh D. Continuous
internal assessment. In: Principles of Medical Education. 3rd
edn. New Delhi: Jaypee Brothers; 2009. p.107-12.
17. Burdick WP. Foreword. In: Singh T,
Anshu, editors. Principles of Assessment in Medical Education. 1st
edn, New Delhi: Jaypee Brothers; 2012.
18. Dijkstra J, van der Vleuten CPM, Schuwirth
LWT. A new framework for designing programmes of assessment. Adv
Health Sci Educ. 2010;15;379-93.
19. Black P, Wiliam D. Assessment and classroom learning.
Assessment in Education.1998;5:7-75.

