|
|
|
Indian Pediatr 2010;47: 931-935 |
 |
Transient Tone Abnormalities in "High Risk"
Infants and Cognitive Outcome at Five Years |
|
Sudha Chaudhari, Mangalmurti Bhalerao, Anjali Chitale, Bharati Patil,
Anand Pandit and Mahendra Hoge
From the Division of Neonatology, Department of
Pediatrics, KEM Hospital, Pune 411 011, Maharashtra, India.
Correspondence to: Dr Sudha Chaudhari, Consultant,
Division of Neonatology, Department of Pediatrics, KEM Hospital,
Pune 411 011, India.
Email: [email protected]
Received: March 20, 2009;
Initial review: April 24, 2009;
Accepted: August 24, 2009.
Published online 2010 January 15.
PII:S097475590900196-1
|
|
Abstract
Objective: To identify transient tone
abnormalities and determine its prevalence in "high risk" infants and
their cognitive outcome at 5 years.
Design: Prospective cohort observational study.
Setting: High risk infants discharged from a
level II neonatal unit in a 12 month period, and followed upto 5 years.
Methods: High risk infants and normal controls
were assessed for abnormalities of tone using the method described by
Amiel-Tison at 3, 6, 9, 12 months. An IQ by Stanford–Binet method and a
preschool inventory by Ayres, Bobath was done at 5 years. Those infants
who had normal tone at 6 and 12 months were called normal high risk (HR)
group and those who had abnormalities at 6 months, which disappeared at
12 months, were called the transient tone abnormalities (TTA) group.
Results: Out of 190 high risk infants, 113 were
normal HR and 67 (35.2%) were labeled as TTA. Ten infants with cerebral
palsy had abnormal tone throughout the first year. Controls had normal
tone throughout the follow-up period. Although there was no difference
in the IQ of the TTA group (98.5 + 12.4) and the normal HR (99.1+13.1)
group, it was significantly less (P=0.04) than that of controls
(106.1 + 9.1). Preschool inventory in TTA children showed poor
language development (P=0.014).
Conclusion: Many of the tone abnormalities
detected at 6 months resolve by 12 months, hence a hasty diagnosis of
cerebral palsy should not be made. High risk infants with transient tone
abnormalities have a normal cognitive outcome at 5 years, except for
poor language skills.
Key words: High risk Neonate, Outcome, Prognosis, Tone
abnormalities.
|
|
E
arly identification of infants at
risk for neurologic and developmental handicap is the main aim of neonatal
follow up programs. Most of the studies from the developed countries
report on follow up of infants weighing less than 1500g. Our ‘high risk’
infant population consists of preterm low birthweight babies, as well as
full term babies with risk factors like birth asphyxia and
hyperbilirubinemia. Besides, a large percentage of our low birthweight
babies are small for gestational age (SGA) and this intrauterine
malnutrition may add a different dimension to their neurodevelopment.
A syndrome of transiently abnormal neurologic signs in
preterm infants was described by Drillen(1) in 1972. She identified
neuromotor abnormalities in 40% of infants with birthweight less than
2000g and normalization of these findings in majority of infants by one
year of age. She followed them upto school age and reported a normal IQ.
Amiel-Tison defined transient tone abnormalities as abnormalities of tone
which are present in early infancy, which disappear by the end of the
first year(2). However, she questioned the presumption that these
abnormalities are innocuous and found that these children later had school
difficulties(3). The aim of our follow-up study was to identify transient
tone abnormalities and to determine its prevalence in ‘high risk’ infants
in the first year and their subsequent cognitive outcome at 5 years.
Methods
Infants discharged from a Level II care Neonatal Unit
of KEM Hospital, Pune during a 12 month period starting from 1 st
October, 1990, were enrolled in this prospective follow up study. The
criteria for selection as high risk were (i) birthweight less than
2000 g; (ii) gestation less than 37 weeks; (iii) seizures; (iv)
apnea; (v) hypoxic ischemic encephalopathy – Sarnat stage II or
III; (vi) intraventricular hemorrhage >grade I; (vii) hyper-bilirubinemia
needing treatment; and (viii) respiratory distress with a Silverman
Anderson score(4) of >3. Infants with congenital anomalies were
excluded. Full term infants with a normal antenatal, natal and postnatal
course, born during the same period, were enrolled as controls. Ethical
clearance was obtained from the hospital committee and parental consent
was taken.
These infants were assessed for tone abnormalities at
3, 6, 9 and12 months using the method described by Amiel-Tison(5).
Corrected age was used in preterms. Evaluation of muscle tone is the
fundamental part of this method. The evaluation of muscle tone is based on
the study of spontaneous posture, passive tone and active tone. Passive
tone is measured by popliteal, adductor and dorsiflexor angles in the
lower extremity and scarf sign in the upper extremity. The range for
normal angles in Indian infants has been previously described by us(6).
Active tone comprises of spontaneous movements and movements provoked by
maneuvers such as pull to sit and pull to stand.
Based on this examination, the infants were categorized
in three groups – (i) hypertonia, (ii) hypotonia, and (iii)
minor tone abnormalities like mild hypertonia or hypotonia in one
extremity, mild adductor or abductor spasm at the hip joint, and mild
hypertonia of the neck extensors. The assessment was jointly done by the
neonatologist and occupational therapist. All infants found to have tone
abnormalities were given occupational therapy.
If there were no tone abnormalities at 6 and 12 months,
the group was called normal high risk (HR) group. If tone abnormalities
were present at 6 months, but disappeared at 12 months, they were called
transient tone abnormalities (TTA) group. Those infants who persisted to
have tone abnormalities at 6 and 12 months, were diagnosed as cerebral
palsy, and referred to our rehabilitation centre and excluded from further
follow up.
The study children were recalled at 5 years of age and
an IQ was done by a trained psychologist using Kulkshetra’s adaptation of
Stanford Binet Intelligence scale(7). An IQ >85 was considered as
normal. A preschool inventory described by Ayres, Bobath(8) was also used,
which consists of assessment of 7 areas of development – gross motor, fine
motor, perception, intersensory integration, preschool skills, activities
of daily living, and language development.
Statistical analysis was done using ANOVA for comparing
means. The difference in groups was analyzed using chi-square test. P
value less than 0.05 was considered as significant. Analysis was done
using Statistical Package for Social Science (SPSS) for Windows (version
10.0).
Results
Two hundred and eight consecutive neonates discharged
from the neonatal unit were enrolled in this study. Sixteen families lived
in far off cities and could not come for regular follow up. Two babies
died after going home. The birthweight and gestational age of this cohort
of 190 neonates is shown in Table I. The cohort had 115
(60.5%) males. Out of the 49 controls, 37 were males. Out of the 119
preterms, 57(47.9%) were small for gestational age (SGA). Out of the 71
full term infants, 38 (53.5%) were SGA.
TABLE I
Birthweight and Gestational Age of the Cohort (n=190)
|
Birthweight (g) |
n (%) |
Gestational |
n (%) |
| |
|
Age (wk) |
|
| <1500 |
33 (17.3) |
< 30 |
7 (3.7) |
| 1500-1999 |
94 (49.5) |
31-32 |
21 (11.0) |
| 2000-2499 |
26 (13.7) |
33-34 |
51 (26.8) |
| |
|
35-36 |
40 (21.0) |
| >2500 |
37 (19.5) |
>37 |
71 (37.4) |
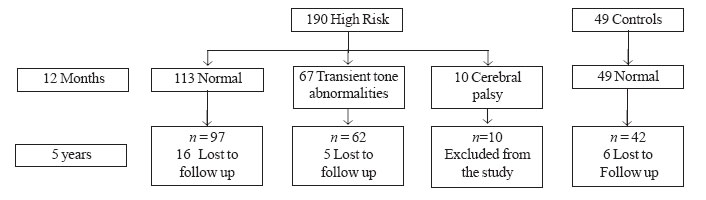
One hundred and thirteen infants had normal tone at 6
and 12 months and formed the normal HR group. The flow chart of the cohort
is shown in Fig. I. Seventy seven (40.5%) infants had tone
abnormalities at 6 months. Sixteen (20.7%) had hypertonia, 23 (29.8%) had
hypotonia and 38 (49.3%) had minor tone abnormalities. Sixty seven (87%)
infants started normalizing at 9 months, and had no tone abnormalities at
12 months. This group was called the transient tone abnormalities or TTA
group. Out of 16 infants with hypertonia, 12 normalized at 12 months. Out
of the 23 infants with hypotonia, 17 normalized, and all 38 infants with
minor tone abnormalities became normal at 12 months. Ten infants had
abnormal tone (4 hypertonia, 6 hypotonia) at 6 and 12 months and were
diagnosed as cerebral palsy and referred to our rehabilitation center and
excluded from the study. Thus, the prevalence of TTA was 35.2% in the
whole high risk cohort.
 |
|
Fig. 1
Flowchart of study participants. |
There was no difference in the proportion of TTA
between fullterms and preterms (30.8% and 35.9%, respectively), VLBW
infants and those with birthweight
³1500g
(41% and 30%, respectively), and SGA and AGA infants (37.8% and 36.4%,
respectively).
All these infants were recalled at 5 years and an IQ
was done. The mean IQ of the TTA group (98.5±12.4) was significantly lower
than that of controls (106±9.8) (P=0.04), but it was well within
normal limits. There was no difference in the mean IQ of the TTA and
normal high risk group.
The preschool inventory showed that there was no
difference in the six skills in the TTA and normal HR group. In the six
items of language development, the TTA group fared poorly. Out of 42
controls, only 4 failed, whereas out of 62 children from the TTA group, 45
failed in language development. This difference was significant (P=0.001).
Discussion
Many of the tone abnormalities detected in the first
six months in high risk infants start normalizing by 9 months and
disappear by 12 months. Our study showed a prevalence of 35.2% for
transient tone abnormalities in a high risk cohort consisting of preterm
and full term infants. Half of the infants with TTA had minor tone
abnormalities and all these normalized at one year. There was no
difference in the prevalence rate amongst preterm and full term infants,
and SGA and AGA infants. When the infants with TTA were recalled at 5
years, their IQ was within normal limits and there was no difference
between the mean IQ of the TTA group and the normal high risk group.
Transient tone abnormalities have been reported in
several follow up studies of preterm infants(9-11). Amiel Tison(3)
reported these abnormalities in a small study of full term infants. Bradt,
et al.(11) have stated that more transient tone abnormalities occur
in preterms compared to full terms. But the cohort in all these
studies(9-11) had many more VLBW infants compared to ours. We found no
significant difference in the incidence of TTA between our small number of
VLBW infants and those weighing >1500 g. Another major difference
between our cohort and those reported in the Western literature was the
higher number of SGA infants. However, there was no difference in the
incidence of TTA between the SGA and AGA group.
In a large follow up study of high risk infants, Matile,
et al.(11) reported that hypertonia found at 6 months disappeared
in 81.2% cases. The tone abnormalities in our high risk cohort disappeared
in 87% of cases. Pedersen, et al.(12) felt that the specificity of
motor evaluation at 7 months regarding cerebral palsy is unsatisfactory
since dystonia at this age is most often transient.
Sommerfelt, et al.(14) reported normal cognitive
development in low birthweight children with transient tone abnormalities
at 5 years. Our children with TTA also had normal cognitive development at
5 years. deVries, et al.(15) assessed preterms and full terms on
two motor items from the Bayley Scales at 39 weeks corrected age and at
2.5 years. They found correlation between poor hand function at 39 weeks
and 2.5 years. They postulated that preterm children had problems in
adequately coordinating their muscle power compared to those born at term.
We found no problems in gross motor, fine motor and coordination in our
TTA group at 5 years. The only abnormal finding on the preschool inventory
was poor language development in the TTA group. Gosselin, et al.(16)
also found language problems in their group with minor neurological signs.
D’Eugenio, et al.(17) followed a group of preterm infants with
gestation of 28-32 weeks and found the incidence of transient
abnormalities to be 82%. They followed them upto 4 years and concluded
that these neurologic abnormalities did not predict cognitive delay.
In conclusion, our study of a cohort consisting of
preterm and full term infants with a high number of SGA infants shows that
many of the tone abnormalities detected at 6 months are transient and
resolve by twelve months. Hence, a hasty diagnosis of cerebral palsy
should not be made till the latter part of the first year. These
abnormalities of tone are not predictive of poor outcome. Our children
with transient tone abnormalities did not show any cognitive impairment at
5 years, except for poor language skills.
Contributors: SC conceived the project,
supervised data collection, wrote the manuscript and will be guarantor for
the paper. MB collected the data. AC did IQ tests. BP did preschool
inventory. AP supervised data collection. MH made home visits, ensured
appointments. The final manuscript was approved by all authors.
Funding: None.
Competing interests: None stated.
|
What This Study Adds?
• The prevalence of transient tone abnormalities in high risk
infants was 35.2%. Many of the tone abnormalities in high risk
infants at 6 months resolve by 12 months.
|
References
1. Drillen CM. Abnormal neurologic signs in the first
year of life in low birthweight infants: Possible prognostic significance.
Dev Med Child Neurol 1972; 14: 575-584.
2. Amiel-Tison C, Stewart A. The Newborn Infant. One
Brain for Life. Paris: Les Editions INSERM; 1994. p. 227.
3. Amiel-Tison C, Dube R, Garel M, Jequier JC. Outcome
at age five years of full term infants with transient neurologic
abnormalities in the first year of life. In: Stern L, Bard H, Frics-Hansen
B, editors. Intensive Care in the Newborn. New York: Masson; 1983. p.
247-258.
4. Silverman WE, Anderson DH. Controlled clinical trial
of effects of water mist on obstructive respiratory signs, death rate and
necropsy findings among premature infants. Pediatrics 1956; 171: 1-2.
5. Amiel-Tison C, Grenier A. Neurological assessment
during first year of life. New York: Oxford University Press; 1986. p.
180-191.
6. Chaudhari S, Deo B. Neurodevelopmental assessment in
the first year with emphasis on evolution of tone. Indian Pediatr 2006;
43: 527-534.
7. Stanford–Binet. Intelligence Scale. Third Revision –
form LM. Kulshreshta, Allahabad: Manas Seva Sansthan Prakashan; 1960.
8. Smith HD. Preschool Inventory. In: Hopkins
HL, Smith HD (eds). Willard and Spackman’s Occupational Therapy.
Philadelphia: JB Lippincott Co; 1983. p. 672-681.
9. Roth SC, Baudin J, Townsend J, McCormick DC.
Neurological impairment at one year predicts neurological and cognitive
outcome at 8 years in very preterm infants. Pediatr Res 1991; 30: 636-637.
10. Stewart AI, Costello A, Hamilton PA, Baudin J.
Relation between neurodevelopmental status at one and four years in very
preterm infants. Dev Med Child Neurol 1989; 33: 756-765.
11. Brandt I, Sticker EJ, Hocky M, Lentze MJ. Transient
abnormal neurologic signs (TANS) in a longitudinal study of very low
birthweight preterm infants. Early Hum Dev 2000; 59: 107-109.
12. Matile PA, Calame A, Plancherel B. Prognostic value
of the neurodevelopmental status in the first year of life in children
with increased perinatal risk. Helv Pediatr Acta 1994; 39: 449-462.
13. Pedersen SJ, Sommerfelt, Markestad T. Early motor
development of premature infants with birthweight less than 2000g. Acta
Pediatr 2000; 89: 1456-1461.
14. Sommerfelt K, Pedersen S, Ellersten B, Markestad T.
Transient dystonia in non-handicapped low birthweight infants and later
neurodevelopment. Acta Pediatr 1996; 85: 1445-1449.
15. de Vries AM, Groot L. Transient dystonias
revisited: a comparative study of preterm and term children at 2 1/2
years of age. Dev Med Child Neurol 2002; 44:
415-421.
16. Gosselin J, Amiel-Tison C, Infante-Rivard C, Fouron
C, Fouron JC. Minor neurological signs and developmental performance in
high risk children at preschool age. Dev Med Child Neurol 2002; 44:
323-328.
17. D’Eugenio DB, Slagle TA, Mettelman BB, Gross SJ.
Developmental outcome of preterm infants with transient neuromotor
abnormalities. Am J Dis Child 1993; 147: 570-574.
|
|
|
 |
|

