|
|
|
Indian Pediatr 2021;58:
485-486 |
 |
Multicystic
Hepatic Lesion: An Unusual Presentation of
Extra-Pulmonary Tuberculosis in a Child
|
|
Pawan Kumar,1 Sudha Sharma2* and
Avik Banerjee3
From Departments of 1Pediatrics
and 2Pathology, Dr YSPGMC, Nahan, HP; and
3Department of Radiodiagnosis, MRI & CT center,
Healthmap Diagnostics Pvt Ltd, Civil Hospital Sector
6, Panchkula, Haryana.
Email:
dr.sudhasharma28@gmail.com
|
|
Tuberculosis of the liver is a
rare form of extra pulmonary tuber-culosis, and is
seen more commonly in immunocompromised patients or
in association with disseminated tuberculosis. Liver
involvement without involvement of lung or other
organs is rare. Nodular form of liver tuberculosis
presenting as abscess is uncommon, and is commonly
mistaken for pyogenic/amebic liver abscess or
malignancy. Definitive diagnosis requires detection
of tubercular bacillus in pus or liver biopsy [1].
A 12-year-old girl presented with
non-localized upper abdominal pain for 3 months,
with history of fever off-and-on and weight loss of
4 kg in two months. There was no history of previous
hospitalization or contact with tuberculosis.
Immuni-zation was complete as per national
immunization schedule; however, BCG scar was absent.
On examination, child was stunted and wasted (weight
for age at –2.04 z-score, height for age at
–2.54 z-score as per IAP charts). General
physical examination revealed severe pallor, angular
cheilitis, mucositis and knuckle hyperpigmentation,
with no lymphadenopathy. On systemic examination,
there was hepatomegaly with other systems being
unremarkable. Chest radiograph was normal.
Ultrasonography abdomen revealed a large
heterogenous solid cystic mass lesion involving the
segment VIII and IV of liver, extending till the
subcapsular regions. A possibility of hydatid
cysts, multiple pyogenic abscesses and fungal
abscesses was kept. On laboratory evaluation,
hemogram was performed: Hemoglobin 4.4 gm/dL, total
leucocyte count 17200/mm3 (lymphocytes 18%,
neutrophils 78%) and peripheral smear revealed
dimorphic blood picture with microcytic hypochromic
and macrocytic normochromic red cells. ESR was
raised (60 mm/h); liver and renal function tests
were normal. Serum iron levels (40 mcg/dL) and serum
B12 levels (160 pg/mL) were both low. Mantoux test
and gastric aspirate for cartridge based nucleic
acid amplification test (CBNAAT) were negative.
Stool microscopy did not reveal cyst or ova and HIV
test and immunodeficiency work up was negative.
Computed tomo-graphy (CT) scan of abdomen revealed a
large ill-defined heterogeneously hypodense mass
lesion involving the left and right lobes (segment
VIII and IV) of liver, faintly hyperdense internal
septations could be seen (Fig. 1). A
possibility of hydatid cysts and malignancy was
kept. Hydatid serology was negative. CT-guided tru-cut
needle biopsy was planned, for which the child was
referred to a higher centre. Liver biopsy showed
multiple epithelioid cell granulomas, positive for
acid-fast bacilli on Ziehl Neelson (ZN) stain. A
diagnosis of tuberculosis was made and child was
started on directly observed treatment, short-course
(DOTS) therapy for tuberculosis. On follow up after
2 months, child started gaining weight and repeat
ultrasonography showed decreasing size of liver
abscesses.
 |
|
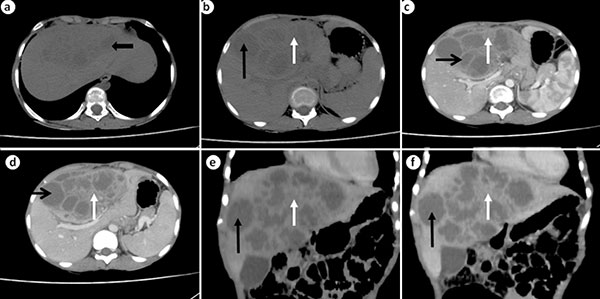
Fig. 1 (a)
Axial plain CT images reveal a large
ill-defined heterogeneously hypodense mass
lesion involving left and right lobes
(segment VIII and IV) of liver; (b)
Cystic appearing areas (black arrow) as well
as solid slightly hyperdense areas (white
arrow) seen within the lesion. Contrast
enhanced CT scan shows axial images: late
arterial phase (c) and porto venous
phase (d), composed of solid and
cystic areas. Cystic areas (black arrow)
show no significant enhancement whereas
solid areas show mild progressive
enhancement (white arrow); Contrast enhanced
CT scan shows coronal images of the lesion.
(e) late arterial phase, (f)
porto venous phase. Lesion is composed of
solid and cystic areas. The cystic areas
(black arrow) show no significant
enhancement whereas solid areas show mild
progressive enhancement (white arrow).
|
Primary hepatic tuberculosis
without pulmonary or miliary tuberculosis is an
uncommon diagnosis. The diagnosis is frequently
missed due to lack of suspicion and can mimic other
etiologies like bacterial, amebic or fungal liver
abscess [2]. In a study from South Africa, in 296
patients with hepatic tuberculosis, tubercular
abscess accounted for only 0.54% cases [3]. In an
Indian study of 242 immunocompetent tuberculosis
patients, 38 had liver involvement, of which 10 had
tubercular liver abscess [4]. Patients usually
present with fever, abdominal pain, anorexia,
hepatomegaly and loss of weight with jaundice being
an uncommon presentation. Right lobe of liver has
been found to be more commonly involved (82.5%) [1].
Radiological findings are
variable and insufficient for diagnosis. Majority of
the cases have shown heterogenous, anechoic or
hypoechoic lesions with irregular margins; however,
some reports have described a hyperechoic mass [5].
Amebic or pyogenic liver abscess or hepatocellular
carcinoma are the differential diagnosis. Definitive
diagnosis can be made by detection of tubercular
bacilli in pus or liver biopsy stained by ZN stain
[1]. Although culture is the gold standard, but it
requires long incubation period. Polymerase chain
reaction has a sensitivity of 92.4% and specificity
of 98%, and should be performed for rapid diagnosis
[6].
We report this case to highlight
a rare manifestation of a common disease. A high
index of suspicion may help in timely diagnosis and
avoid unnecessary investigations or surgical
intervention.
REFERENCES
1. Baveja C, Gumma V, Chaudhary
M, et al. Primary tubercular liver abscess in an
immunocompetent adult: A case report. J Med Case
Rep. 2009;3:78.
2. Bhatt GC, Nandan D, Singh S.
Isolated tuberculous liver abscess in
immunocompetent children – Report of two cases.
Pathog Glob Health. 2013;107: 35-37.
3. Essop AR, Moosa MR, Segal I,
et al. Primary tuberculosis of the liver- A case
report. Tubercle. 1983;64:291-3.
4. Amarapurkar DN, Patel ND,
Amarapurkar AD. Hepatobiliary tuberculosis in
western India. Indian J Pathol Microbiol. 2008;
51:175-81.
5. Chen HC, Chao YC, Shyu RY, et
al. Isolated tuberculous liver abscesses with
multiple hyperechoic masses on ultrasound: A case
report and review of the literature. Liver Int.
2003;23:346-50.
6. Zakham F, Lahlou O,
Akrim M, et al. Comparison of a DNA based PCR
approach with conventional methods for the detection
of Mycobacterium tuberculosis in Morocco. Mediterr J
Hematol Infect Dis 2012;4:e2012049.
|
|
|
 |
|

