Varicella infection is caused due to varicella zoster
virus (VZV) that belongs to family Herpesviridae and genus
Varicellovirus. Primary infection of VZV is referred to as
‘chickenpox’ and subsequent VZV reactivation as ‘herpes zoster or
shingles’ [1]. Varicella outbreaks are frequently reported from various
regions of India [2-9]. Varicella vaccine is not included in India’s
Universal Immunization Program (UIP) however; Indian Academy of
Pediatrics recommends two doses of the vaccine (http://www.iapindia.org)
at 15 months, 3-6 months apart.
Dadra and Nagar Haveli (DNH) consists of 70 different
villages situated on the western coast of India. During 2018-19, in
Silvassa block, cases of fever with skin rash were reported amongst 14
villages. A standard case definition was followed for suspected
varicella [10], and the case details were recorded in a standard data
sheet (i.e. patient details like age, gender, place, date of clinical
onset, type of rashes etc.) Overall, 247 (male; female, 1.22:1) fever
with skin rash cases (including one pregnant woman) were recorded from
14 villages, without any mortality.
Thirty three and 17 serum samples were collected from
the skin-rash cases and their close contacts, respectively. Both the
serum samples and blister swabs were available from two suspected cases,
whereas only blister swabs were available from three suspected cases.
All these sera were subjected to anti-VZV IgM and IgG antibody detection
[10]. Four blister swabs and one blister swab, respectively collected
from Velugam and Surangi villages were processed and subjected to VZV
DNA PCR [10]. PCR positive blister swabs were used for virus isolation
in Vero cells. PCR amplicons were sequenced using forward and reverse
primers, and the consensus sequence was submitted to GenBank (MK959623
to MK959627). All data were analyzed using Epi Info software version
7.2. Descriptive statistics were reported as mean and standard deviation
(SD).
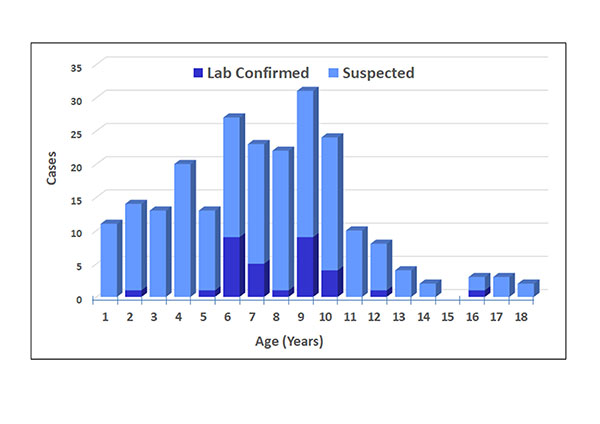
Between November, 2018 and April, 2019, 247 cases of
fever with skin-rash were reported from 14 villages of Silvassa block of
DNH with male-female ratio of 1.22:1. The mean (SD) age was 8.65 (6.48)
year with 92% (228) patients younger than 18 years. The distribution of
fever with skin-rash cases is presented in Fig. 1. Case follow-up
was done up to 25 weeks and none of the cases required hospitalization.
The initial symptoms of vomiting (n=31), appetite loss (n=203),
muscle pain (n=41) and headache (n=179) was followed by
fever and skin rashes (247). None of the cases reported pneumonia or
other complications and all the cases recovered without any further
clinical co-morbidities. Interestingly, clinical symptoms were not
reported in any of their close contacts (i.e. 12 children and 5 adults).
 |
|
Fig. 1 Age-wise distribution of suspected
and laboratory confirmed varicella infection in children below
18 years
|
Thirty three skin rash cases were confirmed by
anti-VZV IgM EIA and VZV DNA PCR and in 3 cases anti-VZV IgG EIA was
positive. Serological and molecular analysis confirmed varicella in 92%
of them. Twenty eight laboratory confirmed varicella cases (VZV IgM) had
median (IQR) onset of 10 days (8-12) (33 out of 36). Thirty six
suspected varicella cases included 35 children (and 1, 24 yrs adult) of
which 90% were (9 out of 10) females and 92.3% (24 out of 26) were
males. Of the 17 contacts, none showed laboratory confirmed varicella
but 15 contacts showed anti-VZV IgG antibodies, indicating past
exposure. The PCR amplicons (n=5) were sequenced and a consensus
gene fragment was used for sequence similarity search using BLAST (https://blast.ncbi.nlm.nih.gov/Blast.cgi),
which indicated the presence of VZV clade-1. Passaging of blister swabs
in vero cells failed to show cell cytopathic effect.
Previously, we reported varicella outbreaks in two
villages from other part of Dadar and Nagar Haveli, where a circulation
of clade-1 VZV was documented [10]. Present report confirms circulation
of a similar VZV clade.
Absence of health awareness and delayed isolation of
cases at home may have resulted in clusters at both villages.
Interestingly, majority of cases had travel history to nearby villages
and may be additional source of transmission; however, this could not be
investigated. In addition, not all cases were referred for laboratory
investigations.
Varicella is vaccine preventable disease but yet to
garner attention in India. Study emphasizes the need for more
investigations on skin rash cases to detect etiology, so as to have
better epidemiological picture of varicella in the country.
Acknowledgement: Authors thank Mr. Sarang S.
Kamble and Mr. Madhukar B. Kamble for their laboratory support. The
Authors also thank Mr. Santosh M. Jadhav for statistical assistance and
Mrs. Sumitha M. Kasibhatla for English language editing.
Ethics Clearance: NIV/IEC/Oct/2020/D-4, 28
October, 2020.
Contributors: SRV: concept and designed the
study, undertaken laboratory investigations and supervision, analyzed
data and written manuscript draft and reviewed; SMT: undertaken
field investigation, collected epidemiological data, analyzed data and
written manuscript.
Funding: None; Competing interest: None
stated.
1. Grose C, Buckingham EM, Carpenter JE, Kunkel JP.
Varicella-Zoster virus infectious cycle: ER stress, autophagic flux, and
amphisome-mediated trafficking. Pathogens. 2016;5:E67.
2. Balraj V, John TJ. An epidemic of varicella in
rural Southern India. J Trop Med Hyg. 1994;97:113-6.
3. Richard VS, John TJ, Kenneth J, et al. Should
health care workers in the tropics be immunized against varicella? J
Hosp Infect. 2001;47:243-45.
4. Paul N, Jacob ME. An outbreak of cadaver-acquired
chickenpox in a health care setting. Clin Infect Dis. 2006;43:599-601.
5. Singh MP, Singh G, Kumar A, et al. Epidemiologic
lessons: Chickenpox outbreak investigation in a rural community around
Chandigarh, North India. Indian J Pathol Microbiol. 2011;54:
772-74.
6. Sood S. Occupationally related outbreak of
chickenpox in hospital staff: A learning experience. J Clin Diagn Res.
2013;7:2294-295.
7. Singh MP, Chandran C, Sarwa A, et al. Outbreak of
chickenpox in a union territory of North India. Indian J Med Microbiol.
2015; 33:524-27.
8. Gupta SN, Gupta N, Gupta S. Concurrent multiple
outbreaks of varicella, rubeola, german measles in unvaccinated children
of co-educational mount carmel senior secondary school, Thakurdwara
Palampur of Northern Himachal, India. J Family Med Prim Care.
2015;4:117-23.
9. Meyers J, Logaraj M, Ramraj B, et al. Epidemic
varicella zoster virus among university students, India. Emerg Infect
Dis. 2018;24:366-69.
10. Vaidya SR, Tilavat SM, Kumbhar NS, Kamble MB. Chickenpox outbreak
in a tribal and industrial zone from the union territory of Dadra and
Nagar Haveli, India. Epidemiol Infect. 2018;146: 476-80.

