The novel coronavirus disease 2019
(COVID-19) was declared a pandemic by the World
Health Organization (WHO) on March 11, 2020. The
causative agent, severe acute respiratory syndrome
coronavirus-2 (SARS-CoV-2), attaches through its
viral surface spike proteins to the angiotensin
converting enzyme-2 (ACE-2) receptors on the
respiratory epithelial cells. Although several
months into the pandemic, there is a lack of clarity
regarding management of COVID-19 infection in
children. This review aims to summarize the key
clinical presentations and management of Pediatric
COVID-19 based on most pertinent available evidence.
The Medline database was searched for seminal
articles on COVID-19 presentation and management in
children less than 18 years of age. The latest
guidelines from World Health Organization (WHO) and
Ministry of Health and Family Welfare (MoHFW),
Government of India were also reviewed [1,2].
EPIDEMIOLOGY IN CHILDREN
Children account for less than 5%
of diagnosed COVID-19 infections worldwide [3]. As
per the MoHFW, 8% of the COVID-19 positive cases in
India were contributed by people below 17 years of
age [4].
Reports show a lower need for
hospital and intensive care unit (ICU) admission and
lower mortality rate (0-0.7%) in children compared
to adults [5]. This may be due to lower exposure,
strong innate immune response due to trained
immunity, healthier blood vessel endothelium,
excellent alveolar epithelium regeneration capacity
and fewer co-morbidities [6]. The community spread
of virus by children is of concern as a high rate of
asymptomatic infection is seen in younger age
groups. However, data show lower transmission rate
by children than adults [7,8].
CLINICAL FEATURES
The median age of presentation in
children ranged from 3.3-11 years in different
studies with a male preponderance [5,9,10]. When
compared to adults, majority of COVID-19 infected
children are asymptomatic with gastrointestinal and
mild respiratory manifestations being the commonest
[5,9-11]. Anosmia and ageusia are difficulty to
elicit in young children and reported less commonly
[5]. Other symptoms include lethargy, altered
sensorium, seizures, sore throat, fatigue, myalgias,
oligo-anuria, and skin rash. Severe or critical
disease (acute respiratory distress syndrome,
respiratory failure, shock, myocardial failure, and
multiorgan dysfunction) is described in less than
1-3% children [10]. Viral co-infections have been
reported in around 6% patients. Underlying
co-morbidities (underlying malignancy, nephrotic
syndrome, chronic disease of kidney, lung, or liver)
are associated in 9.9 - 42% of SARS-CoV-2 positive
children [12,13]. It is imperative to evaluate and
treat these common infections and co-morbidities as
COVID-19 may just be a bystander.
The COVID-19 disease
severity classification is presented in
Table I [1,14]. Indications for admission
include children with moderate, severe or critical
COVID-19 disease. Mild disease can be managed at
home. However, if the child has any underlying
co-morbidity or if home isolation is not feasible,
the child may managed at a COVID care centre or
hospital.
INVESTIGATIONS
All patients with moderate to
severe COVID-19 should undergo investigations as
detailed in Box I. Investigations to rule out
other possible differentials (like enteric fever,
dengue, malaria, etc.) should be done as indicated.
MANAGEMENT
Mild Cases
Mild cases should be isolated at
home, a community facility (COVID care-center) or a
health facility decided on a case-to-case basis
[1,2]. Pre-requisites for home isolation include apt
residential conditions for quarantine of patient and
family contacts, absence of co-morbidities and
presence of a caregiver with communication link to
the hospital. Strict adherence to home quarantine
guidelines is necessary [22]. Any difficulty in
breathing, grunting, inability to breast feed,
bluish discoloration of lips or face, dip in oxygen
saturation <95%, chest pain, mental confusion,
inability to arouse and reduced interaction when
awake should prompt urgent referral to a dedicated
COVID health center or hospital. Symptomatic
treatment should be given with antipyretic (Paracetamol)
for fever and pain when necessary, adequate
nutrition and rehydration, and identification and
treatment of any underlying co-morbidities or
co-infections. In children with symptomatic
respiratory tract infection, routine use of
antibiotics is not recommended except in situations
of suspected or confirmed bacterial co-infection.
Respiratory tract infection management should be
followed as per existing protocols [23].
Asymptomatic cases who are
incidentally detected like contacts of a diagnosed
case or planned for an elective surgery may be
isolated and monitored. A COVID positive status
during surgery may pose a risk for infection spread
and portend poor surgical outcome [24]. Therefore,
elective surgeries should be delayed until patients
test negative for COVID-19 [25,26].
Moderate Cases
Moderate cases should be treated
in a dedicated COVID health center or hospital with
detailed clinical history and regular assessment for
vital signs, work of breathing and oxygen saturation
(SpO2). Investigations as described in Table II
should be done at admission [1,2]. General
management should be done as stated above.
Additionally, the following may be considered [1,2].
i) Supplemental oxygen
therapy should be used for distressed breathing
or hypoxia (detailed below with management of
severe cases). Bronchodilators if required are
preferably delivered with an MDI and spacer
instead of a nebulizer.
ii) Empiric antibiotic
therapy may be given in under-five children. In
the absence of hypoxia, an oral antibiotic (amoxycillin-clavulanic
acid/azithromycin) may be added while
intravenous ceftriaxone (50-100 mg/kg/day in two
divided doses) may be started for moderate
COVID-19 cases with hypoxia or infiltrates on
chest X-ray.
iii) Chloroquine (5–10
mg/kg/day for 5-10 days) was used in children
with moderate to severe COVID disease in initial
months of the pandemic [27]. However, latest
evidence shows no role of chloroquine or
hydroxy-chloroquine in treatment of COVID-19
[28].
Close monitoring for disease
progression, repeat investigations at 48-72 hours if
needed and provision of transportation to dedicated
COVID care hospital should be available.
Severe and Critical Cases
All severe and critical COVID-19
cases should be admitted in a dedicated COVID care
hospital with detailed work-up as elucidated above.
Continuous monitoring of vitals, work of breathing
and SpO2 should be done.
i) All patients should be
started on empirical intravenous antibiotics
(third generation cephalosporins) within an hour
of arrival which should be escalated as per
clinical assessment.
ii) Aggressive
intravenous fluid resuscitation should be
avoided as it may worsen oxygenation.
iii) Experience of awake
proning in children is limited as their
tolerance may not be good and any agitation can
worsen hypoxia.
iv) Supplemental oxygen
therapy is required to maintain SpO2
³
94% while taking all precautions to minimize
aerosol generation.
The following modes of oxygen
delivery may be used:
Conventional oxygen therapy
may be given using nasal prongs/cannula,
oxygen mask or hood. Non-rebreathing mask can
provide up to 95% FiO2 at oxygen flow rate of 10 -15
L/ min and can be used for short periods initially
[29].
HHHFNC/HFNC (Heated humidified
high flow nasal canula) [30], is indicated in
patients with mild ARDS without evidence of
hemodynamic instability, altered mental status or
multi-organ failure. However, in absence of
response, consider early escalation to BiPAP/invasive
ventilation. Although, increased aerosolization risk
with HHHFNC has been speculated, the certainty of
evidence is low and it is a widely preferred option
in resource poor settings. A triple layer mask may
be used to cover the mouth and nose of the patient
over the nasal cannula to decrease aerosolization
[29].
Non-invasive Ventilation
BiPAP (Bilevel Positive
Airway Pressure): It is indicated for mild acute
respiratory distress syndrome without hemodynamic
instability, altered mental status or multi-organ
failure. However, its use is feasible only in an
older, cooperative child accepting of oronasal BiPAP
mask [29].
Bubble CPAP (Continuous
positive airway pressure) may also be used for
newborns and children with severe hypoxemia.
Invasive Ventilation
Tracheal intubation should be
performed when failure/contraindication of
BiPAP/HFNC occurs. The following specific
precautions are needed:
• Pre-oxygenate with a
non-rebreathing mask (NRM) or tight-fitting face
mask attached to a self-inflating bag with100%
oxygen for 5 minutes. Avoid bag and mask
ventilation (BMV) to limit aerosolization and if
required, use low tidal volumes.
• Follow Rapid sequence
intubation using sedation and analgesia (to
avoid cough reflex).
• Use a cuffed endotracheal
tubes (ETT)
• Ensure intubation by most
experienced person to minimize attempts and use
video laryngoscope for intubation to maintain
safe distance from patient.
• May use a plastic sheet to
cover the head, neck and chest of patient to
minimize contamination.
• Use disposable ventilator
circuits and hydrophobic viral filter between
the ventilator circuit at the expiratory end.
• Use closed suction to
minimize contact with secretion and aerosol
release.
The pediatric ARDS protocol for
management should be used. Prone ventilation
may be difficult to conduct in a child and
may unnecessarily increase the risk of infection to
the healthcare workers.
Extracorporeal membrane
oxygenation (ECMO) may be considered in patients
with continued severe hypoxemia despite maximal
ventilatory support.
Management of Shock
Standard care includes early
recognition and the initiation of antimicrobial
therapy and slow crystalloid fluid bolus within 1
hour of recognition and vasopressors for fluid
non-responsive hypotension. Further management may
be as per the Surviving Sepsis Campaign guidelines
for the management of septic shock in children [31].
Adjunctive Therapies for COVID-19
Steroids
:
Glucocorticoids may be considered for patients with
severe or critical COVID-19 disease with progressive
deterioration of oxygenation indicators, rapid
worsening on imaging and excessive activation of the
body’s inflammatory response. The recommended doses
include intravenous methylprednisolone 1 –
2mg/kg/day (maximum 80 mg) for 10 days or oral/
injectable dexamethasone 0.2-0.4 mg/kg/day OD
(maximum of 6 mg) for 5 days [1,2]. These
recommendations have been extrapolated from studies
conducted chiefly in adults. The UK-based RECOVERY
trial) reported dexamethasone to reduce mortality in
patients who required respiratory support [32]. The
proportion of children enrolled and analysed was not
clear.
Anticoagulation [17,33]:
Recommendations for use in children are listed in
Box II. Thromboprophylaxis, both mechanical
(with sequential compression devices, where
feasible) and anticoagulation are recommended. Low
molecular weight heparin (enoxaparin) 1.5 IU/kg/dose
subcutaneous twice a day for <2 months age and 1
IU/kg/dose twice a day for >2 months should be used.
Unfractionated heparin may be used for children who
are clinically unstable or have severe renal
impairment as loading dose 75-100IU/kg intravenous
in 10 min followed by initial maintenance dose of 28
IU/kg/hour for age <1 year and 20 IU/kg/hour for
1-18 years (target aPTT between 65-80 seconds).
Anticoagulation therapy may be continued till
resolution of the hypercoagulable state or
resolution of the clinical risk factors for venous
thrombo-embolism [17].
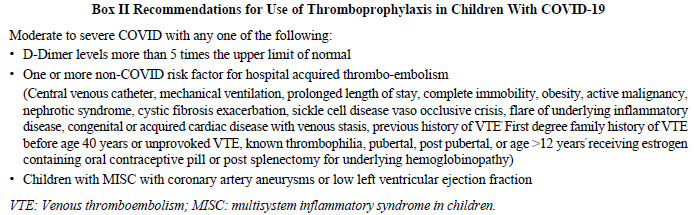 |
Thromboprophylaxis is
contraindicated in active/major bleeding, need for
emergency surgery, platelets < 20,000/mm3,
concomitant aspirin administration at doses
>5 mg/kg/d and malignant hypertension.
Remdesivir: There are no
comparative clinical data evaluating the efficacy or
safety of remdesivir for COVID-19 in pediatric
patients. Although, initial guidelines
contraindicated its use in children < 12 years, the
US Food and Drug Administration issued an Emergency
Use Authorization (EUA) to permit the use of
remdesivir for treatment of COVID-19 in hospitalized
pediatric patients [34]. As per NIH guidelines,
remdesivir is indicated only in moderate COVID-19
with supplemental oxygen requirement where it
shortens the time to recovery [34,35]. It may be
considered in severe to critical COVID-19 (high flow
oxygen device, NIV, invasive ventilation or ECMO)
with dexamethasone (expert opinion) [34]. The latest
guidelines are similar for children albeit
extrapolated from adult data and recommended as a
part of clinical trials [36]. Few case series in
children show promise [37].
For children weighing > 40 kg, a
single loading dose of 200 mg on day 1 followed by
once daily dose of 100 mg from day 2 for 5-10 days
is used. For children weighing 3.5- 40 kg, a single
loading dose of 5 mg/kg on day 1 followed by 2.5
mg/kg once daily from day 2 for 5-10 days may be
given. The contraindications for its use include
AST/ALT > 5 times upper limit of normal (ULN) and
severe renal impairment (eGFR <30mL/min/m2
or need for hemodialysis). Remdesivir should not be
used in combination with chloroquine or
hydroxychloroquine [34].
Tocilizumab (TCZ): It is a
monoclonal antibody against interleukin-6 (IL-6)
receptor which emerged as an alternative treatment
for COVID-19 patients with cytokine storm. While
initial systematic reviews show that TCZ resulted in
reduction of mortality in severe COVID-19 cases
compared to the standard treatment, the latest
trials showed no benefit [38-40]. A larger ongoing
RCT which is also enrolling children may provide
clearer answers [41]. The use of TCZ is suggested
only in context of clinical trials [34] in those
with moderate/severe disease where
oxygen/ventilation requirement is increasing after
use of steroids with extensive bilateral lung
disease on radio-imaging [2,17]. The dose of TCZ for
>30 kg is 8 mg/kg (up to maximum of 800 mg) and <30
kg is 12 mg/kg given as intravenous infusion over 1
hour once, may be repeated if required at 12-24 hrs.
Contraindications to use include
patients with HIV, those with active infections
(uncontrolled systemic bacterial/fungal),
tuberculosis, active hepatitis (total bilirubin or
AST/ALT raised > 5 times ULN), ANC < 500-2000/mm3
and platelet count <50,000-1,00,000/mm3. Recipients
should be carefully monitored for secondary
infections, neutropenia, and thrombocytopenia. All
patients should obtain a latent tuberculosis (TB)
test before TCZ therapy. If the text is positive,
treatment for tuberculosis should be started prior
to administration although, the risk for latent TB
reactivation is very compared to the benefit of
administering TCZ. Safety profile of TCZ in COVID-19
patients is yet to be understood.
Convalescent plasma therapy
(CPT): It may be considered in patients with
moderate disease who are not improving with
steroids. Few reports of its use in children with
severe COVID-19 show promise [42,43]. Special
considerations while using CPT include ABO
compatibility, neutralizing titre of donor plasma
above the specific threshold and avoidance of use in
patients with IgA deficiency or immunoglobulin
allergy. While adult trials have used doses of 4 to
13 ml/kg (usually 200 mL single dose) given slowly
over 2 hours, 2-4 mL/kg of convalescent plasma has
been used in children [43].
Other Agents Under Evaluation
Ivermectin, a potent in vitro
inhibitor of the COVID-19 causative virus
(SARS-CoV-2) with an established safety profile for
human use, was shown to be beneficial in COVID-19
[44]. A newer agent under evaluation is the
interleukin (IL)-1 inhibitor anakinra which may be
considered for immunomodulatory therapy (>4
mg/kg/day intravenous or subcutaneous) in COVID-19
with hyperinflammation. Initiation of anakinra
before invasive mechanical ventilation may be
beneficial [33]. Other potential treatments under
evaluation include interferon-beta, anti-IL-6
receptor monoclonal antibodies (sarilumab),
anti-IL-6 monoclonal antibody (siltuximab), Bruton’s
tyrosine kinase inhibitors, acalabrutinib,
ibrutinib, zanubrutinib) and Janus kinase
inhibitors (baricitinib, ruxolitinib, tofacitinib).
A recent trial has shown benefit of
baricitinib-remdesivir combination compared to
remdesivir alone in reducing recovery time in
COVID-19 patients [45]. However, there is
insufficient data for recommending use of any of
these agents in children except in the context of a
clinical trial [34].
Discharge Criteria and Follow-Up
The patient with mild to moderate
disease can be discharged after 10 days of symptom
onset and no fever or oxygen requirement for three
consecutive days with complete resolution of
symptoms prior to discharge [48]. Negative RT-PCR
before discharge is not required. Home quarantine
for 7 days post-discharge is necessary. Patients
with severe disease and immunocompromised states
(like cancer transplant recipients and HIV) should
have complete resolution of symptoms and negative
RT-PCR test report prior to discharge [48].
MULTISYSTEM INFLAMMATORY SYNDROME
IN CHILDREN (MIS-C)
MIS-C is a post-infectious
inflammatory response syndrome (characterized by
high levels of pro-inflammatory cytokines CTNF, IL-6
and IL-1
b)
following SARS-CoV-2 infection. Various diagnostic
criteria have been provided by WHO and CDC
[33]. A tiered investigational approach is
followed in patients without life-threatening
manifestations, while work-up is done simultaneously
for the sick children [33]. Patients may require
additional investigations to rule out any
co-infection/other cause of illness.
Children with life threatening
manifestations should be admitted in PICU
management. Children with acute COVID inflammation
(RT-PCR positive) with symptoms like Kawasaki
disease (KD) should receive intravenous
immunoglobulin (IVIG) (dose-2g/kg over 1-2 days) and
remdesivir if available. Children with remote COVID
infection with KD symptom overlap should receive
IVIG and aspirin (20–25 mg/kg/dose every 6 hourly or
80-100 mg/kg/day) steroids may be added. In children
with remote COVID infection with predominant
cardiovascular involvement (myocarditis/cardiogenic
shock/distributive shock) with or without KD symptom
overlap IVIG, 3-day pulse of methylprednisolone with
tapering and LMWH prophylaxis are to be considered
as disease modifying agents [46].
Sick children should receive
initial broad-spectrum antibiotics considering
symptom overlap with severe bacterial infection.
Ceftriaxone or meropenem with vancomycin or
clindamycin or teicoplanin may be used for the
sickest children. In stable patients with MIS
overlap, with mild lab abnormalities and lacking
alternate diagnosis, ceftriaxone may be given.
Metronidazole is added if gastro-intestinal symptoms
are predominant.
All children with MIS-C require
ongoing clinical monitoring while laboratory
investigations may be repeated every 24-48 hourly as
guided by the clinical condition [47].
Contributors: PKS: reviewed
literature, drafted the manuscript; UJ:
conceptualized, drafted and critically appraised the
manuscript; AD: drafted and critically appraised the
manuscript.
Funding: None; Competing
interests: None stated.
REFERENCES
1. Clinical management of
COVID-19. Interim guidance. WHO. Published 27 May
2020. Available from:
https://www.who.int/publications/i/item/clinical-management-of-covid-19.
Accessed September 18, 2020.
2. Updated Clinical Management
Protocol for COVID-19. Ministry of Health and Family
Welfare. Government of India. Published July 3,
2020. Accessed August 3, 2020. Available from:https://www.mohfw.gov.in/pdf/UpdatedClinical
ManagementProtocolforCOVID19dated03072020.pdf.
3. Wu Z, McGoogan JM.
Characteristics of and important lessons from the
coronavirus disease 2019 (COVID-19) outbreak in
China: Summary of a report of 72 314 cases from the
Chinese Center for Disease Control and Prevention.
JAMA. 2020; 323:1239.
4. Coronavirus in India: 54%
COVID-19 cases in age group 18-44 years, 51% deaths
among those aged 60 years and above. Published Sep
02, 2020. Accessed September 18, 2020. Available
from:
https://www.financialexpress.com/lifestyle/health/coronavirus-in-india-54-pc-covid-19-cases-in-age-group-18-44-years-51-pc-deaths-among-those-aged-60-years-and-above/2072525/.
5. Rabinowicz S, Leshem E,
Pessach IM. COVID-19 in the pediatric
population-review and current evidence. Curr Infect
Dis Rep. 2020;22:29.
6. Dhochak N, Singhal T, Kabra
SK, Lodha R. Pathophysiology of COVID-19: Why
children fare better than adults? Indian J Pediatr. 2020;87:537-46.
7. Rajmil L. Role of children in
the transmission of the COVID-19 pandemic: A rapid
scoping review. BMJ Paediatr Open. 2020;4:e000722.
8. Viner RM, Mytton OT, Bonell C,
et al. Susceptibility to SARS-CoV-2 infection among
children and adolescents compared with adults: A
systematic review and meta-analysis [published
online ahead of print, 2020 Sep 25]. JAMA
Pediatr. 2020; e204573.
9. Dong Y, Mo X, Hu Y, et al.
Epidemiology of COVID-19 among children in China. Pediatrics.
2020;145:e20200702.
10. Meena J, Yadav J, Saini L,
Yadav A, Kumar J. Clinical features and outcome of
SARS-CoV-2 infection in children: A systematic
review and meta-analysis. Indian Pediatr. 2020;
57:820-26.
11. Pei Y, Liu W, Masokano IB, et
al. Comparing Chinese children and adults with
RT-PCR positive COVID-19: A systematic review. J
Infect Public Health. 2020;13:1424-31.
12. Garazzino S, Montagnani C,
Donà D, et al. Multicentre Italian study of
SARS-CoV-2 infection in children and adolescents,
preliminary data as at 10 April 2020. Euro Surveill.
2020;25: 2000600.
13. Swann OV, Holden KA, Turtle
L, et al. Clinical characteristics of children and
young people admitted to hospital with covid-19 in
United Kingdom: Prospective multicentre
observational cohort study. BMJ. 2020;370:m3249.
14. Pediatric Acute Lung Injury
Consensus Conference Group. Pediatric acute
respiratory distress syndrome: Consensus
recommendations from the Pediatric Acute Lung Injury
Consensus Conference. Pediatr Crit Care
Med. 2015;16: 428-39.
15. Kosmeri C, Koumpis E,
Tsabouri S, Siomou E, Makis A. Hematological
manifestations of SARS-CoV-2 in children. Pediatr
Blood Cancer. 2020;67:e28745.
16. Katal S, Johnston SK,
Johnston JH, Gholamrezanezhad A. Imaging findings of
SARS-CoV-2 infection in Pediatrics: A systematic
review of coronavirus disease 2019 (COVID-19) in 850
patients [published online ahead of print, 2020 Jul
30]. Acad Radiol. 2020;S1076-6332:30454-2.
17. Goldenberg NA, Sochet A,
Albisetti M, et al. Consensus-based clinical
recommendations and research priorities for
anticoagulant thromboprophylaxis in children
hospitalized for COVID-19-related illness. J Thromb
Haemost. 2020;18: 3099-105.
18. Koçak G, Ergul Y, Niºli K, et
al. Evaluation and follow-up of pediatric COVID-19
in terms of cardiac involvement: A scientific
statement from the Association of Turkish Pediatric
Cardiology and Pediatric Cardiac Surgery. Anatol J
Cardiol. 2020;24:13-18.
19. Henry BM, Aggarwal G, Wong J,
et al. Lactate dehydrogenase levels predict
coronavirus disease 2019 (COVID-19) severity and
mortality: A pooled analysis. Am J Emerg Med.
2020;38:1722-6.
20. Mojtabavi H, Saghazadeh A,
Rezaei N. Interleukin-6 and severe COVID-19: A
systematic review and meta-analysis. Eur Cytokine
Netw. 2020;31:44-9.
21. Han J, Gatheral T, Williams
C. Procalcitonin for patient stratification and
identification of bacterial co-infection in
COVID-19. Clin Med (Lond). 2020;20:e47.
22. Revised guidelines for home
isolation of very mild/pre-symptomatic/asymptomatic
COVID-19 cases. Government of India Ministry of
Health & Family Welfare. Published July 2, 2020.
Available at:
https://www.mohfw.gov.in/pdf/Revised HomeIsolation
Guidelines.pdf. Accessed September 18, 2020.
23. Balasubramanian S, Rao NM,
Goenka A, Roderick M, Ramanan AV. Coronavirus
Disease 2019 (COVID-19) in Children - What we know
so far and what we do not. Indian Pediatr.
2020;57:435-42.
24. COVID Surg Collaborative.
Mortality and pulmonary complications in patients
undergoing surgery with perioperative SARS-CoV-2
infection: An international cohort study [published
correction appears in Lancet. 2020 Jun
9]. Lancet. 2020;396:27-38.
25. Chan Y, Banglawala SM, Chin
CJ, et al. CSO (Canadian Society of Otolaryngology -
Head & Neck Surgery) position paper on rhinologic
and skull base surgery during the COVID-19
pandemic. J Otolaryngol Head Neck Surg. 2020;49:81.
26. Morris M, Pierce A, Carlisle
B, Vining B, Dobyns J. Pre-operative COVID-19
testing and decolonization. Am J Surg.
2020;220:558-60.
27. Pastick KA, Okafor EC, Wang
F, et al. Review: Hydroxychloroquine and chloroquine
for treatment of SARS-CoV-2 (COVID-19). Open Forum
Infect Dis. 2020;7:ofaa130.
28. Takla M, Jeevaratnam K.
Chloroquine, hydroxychloroquine, and COVID-19:
Systematic review and narrative synthesis of
efficacy and safety [published online ahead of
print, 2020 Nov 13]. Saudi Pharm J.
2020;10.1016/j.jsps.2020.11.003.
29. Sundaram M, Ravikumar N,
Bansal A, et al. Novel Coronavirus 2019 (2019-nCoV)
Infection: Part II - Respiratory Support in the
Pediatric Intensive Care Unit in Resource-limited
Settings. Indian Pediatr. 2020;57:335-42.
30. Agarwal A, Basmaji J,
Muttalib F, et al. High-flow nasal cannula for acute
hypoxemic respiratory failure in patients with
COVID-19: Systematic reviews of effectiveness and
its risks of aerosolization, dispersion, and
infection transmission. Can J Anaesth.
2020;67:1217-48.
31. Weiss SL, Peters MJ,
Alhazzani W, et al. Surviving sepsis Campaign
International Guidelines for the Management of
Septic Shock and Sepsis-associated Organ Dysfunction
in Children. Pediatr Crit Care Med.
2020;21:e52-e106.
32. RECOVERY Collaborative Group,
Horby P, Lim WS, et al. Dexamethasone in
Hospitalized Patients with Covid-19 - Preliminary
Report [published online ahead of print, 2020 Jul
17]. N Engl J Med. 2020;NEJMoa2021436.
33. Henderson LA, Canna SW,
Friedman KG, et al. American College of Rheumatology
Clinical Guidance for Pediatric Patients with
Multisystem Inflammatory Syndrome in Children
(MIS-C) Associated with SARS-CoV-2 and
Hyperinflammation in COVID-19. Version 1 [published
online ahead of print, 2020 Jul 23]. Arthritis
Rheumatol. 2020;10.1002/art.41454.
34. COVID-19 Treatment Guidelines
Panel. Coronavirus disease 2019 (COVID-19) Treatment
Guidelines. National Institutes of Health. Available
from: https://www.covid19treatmentguide
lines.nih.gov/ Accessed October 20, 2020.
35. Beigel JH, Tomashek KM, Dodd
LE, et al. Remdesivir for the treatment of Covid-19
- final report. N Engl J Med. 2020;383:1813-26.
36. Chiotos K, Hayes M, Kimberlin
DW, et al. Multicenter interim guidance on use of
antivirals for children with COVID-19/SARS-CoV-2
[published online ahead of print, 2020 Sep 12]. J
Pediatric Infect Dis Soc. 2020;piaa115.
37. Méndez-Echevarría A,
Pérez-Martínez A, Gonzalez Del Valle L, et al.
Compassionate use of remdesivir in children with
COVID-19 [published online ahead of print, 2020 Nov
16]. Eur J Pediatr. 2020;1-6.
38. Aziz M, Haghbin H, Sitta EA,
et al. Efficacy of Tocilizumab in COVID-19: A
systematic review and meta-analysis [published
online ahead of print, 2020 Sep 12]. J Med Virol.
2020;10.1002/jmv.26509.
39. WHO SOLIDARITY Trial
Consortium, Pan H, Peto R, Karim Q, et al.
Repurposed antiviral drugs for COVID-19 – interim
WHO SOLIDARITY trial results. MedRxiv 2020.
40. Furlow B. COVACTA trial
raises questions about tocilizumab’s benefit in
COVID-19. Lancet Rheumatol. 2020;2:e592.
41. Covid-19: The inside story of
the RECOVERY trial. BMJ. 2020;370:m2800.
42. Piechotta V, Chai KL, Valk
SJ, et al. Convalescent plasma or hyperimmune
immunoglobulin for people with COVID-19: A living
systematic review. Cochrane Database Syst Rev.
2020;7:CD013600.
43. Diorio C, Anderson EM,
McNerney KO, et al. Convalescent plasma for
pediatric patients with SARS-CoV-2-associated acute
respiratory distress syndrome [published online
ahead of print, 2020 Sep 4]. Pediatr Blood Cancer.
2020;e28693
44. Padhy BM, Mohanty RR, Das S,
Meher BR. Therapeutic potential of ivermectin as add
on treatment in COVID 19: A systematic review and
meta-analysis. J Pharm Pharm Sci. 2020;23:462-9.
45. Kalil AC, Patterson TF, Mehta
AK, et al. Baricitinib plus remdesivir for
hospitalized adults with Covid-19 [published online
ahead of print, 2020 Dec 11]. N Engl J Med.
2020;10.1056/NEJMoa2031994.
46. Bhat CS, Gupta L,
Balasubramanian S, Singh S, Ramanan AV.
Hyperinflammatory syndrome in children associated
with COVID-19: Need for awareness. Indian Pediatr.
2020;57: 929-35.
47. Hennon TR, Penque MD,
Abdul-Aziz R, et al. COVID-19 associated multisystem
inflammatory syndrome in children (MIS-C)
guidelines; A Western New York approach [published
online ahead of print, 2020 May 23]. Prog Pediatr
Cardiol. 2020;101232.
48. Revised discharge policy for COVID-19.
Government of India. Ministry of Health and Family
Welfare. Published on 8 May, 2020. Accessed
September 18, 2020. Available from:
https://www.mohfw.gov.in/pdf/ReviseddischargePolicyforCOVID19.
pdf

