|
|
|
Indian Pediatr 2021;58: 430-435 |
 |
Patterns and Trends of Childhood Cancer
Incidence (0-14 Years) in Delhi, India: 1990-2014
|
|
Rajeev Kumar Malhotra, 1
Nalliah Manoharan, 1
Omana Nair, 2
SVS Deo,3 Sameer
Bakhshi,4
Gourva
Kishore Rath2
From 1Delhi Cancer Registry, and Departments of
2Radiotherapy, 3Surgical Oncology and 4Medical Oncology, Dr
BRAIRCH, AIIMS, New Delhi, India.
Correspondence to: Dr Rajeev Kumar Malhotra, Delhi Cancer
Registry, Dr. BRAIRACH, AIIMS, New Delhi, India.
Email:
[email protected]
Received: May 21, 2020;
Initial review: June 19, 2020;
Accepted: November 25, 2020.
|
|
Objectives: To
investigate the patterns and temporal trends of childhood cancer
incidence (0-14 years) in Delhi from 1990 to 2014.
Methods: The new
childhood cancer cases diagnosed between 1990 and 2014 were
extracted from the Delhi population-based cancer registry
(PBCR). Joinpoint regression analysis was performed to assess
the temporal behaviour of new childhood cancer. The magnitude of
temporal trend was assessed by estimated annual percentage
changes (EAPCs).
Results: The Delhi
PBCR registered 12,637 cases (8484 boys and 4153 girls) during
1990-2014. The overall childhood cancer was twice in boys than
girls (5.62% vs. 2.78%). The age-standardised incidence rates
(ASIRs) of childhood cancer adjusted to the WHO World standard
population distribution (year 2000) was 163 per one million in
boys and 92 per one million in girls; median age at diagnosis
being 6 and 7 years, respectively. Five-top childhood cancer
sites was leukaemia, lymphoma, central nervous system (CNS),
bone and retinoblastoma. A decreasing linear trend in proportion
of new childhood cancer cases to total all age-group cancer was
observed in both sexes during this period. The percentage
increase in childhood cancer is similar in both sexes from
1990-94 to 2010-14 (97% vs. 93%). Increasing trend in ASIRs of
childhood cancer was observed. Conclusion: The new
childhood cancer cases observed increasing trend during 1990 to
2014. Boys had nearly double the number of childhood cancer
cases than girls while population ratio of boys and girls during
the same period was 1.14:1.
Keywords: Age-standardized
incidence rate, Annual percentage change, Epidemiology.
|
C hildhood cancer
incidence is increasing worldwide; developing countries have
higher incidence and mortality as compared to developed
countries [1]. Globally top-five childhood cancer sites are
leukaemia, lymphoma, central nervous system (CNS), kidney
and liver, with boys showing a higher proportion of cancer
than girls [2,3]. Age standard incidence rate (ASIRs) in
India for childhood cancer were 91 per one million and 65
per one million in boys and girls respectively [3].
According to a recent report based on 28
population based cancer registries (PBCRs), the proportion
of new childhood cancer to total cancer varied from 0.8% -
4.7% in boys and 0.5% - 2.6% in girls during 2012-2016. This
may be due to variation in environmental exposures or
biological susceptibility within Indian regions [4]. Delhi
showed the highest proportion of childhood cancer for both
boys (4.7%) and girls (2.6%) compared to other region of the
country. Delhi observed highest ASIRs among boys (203.1 per
one million) as well as among girls (125.3 per one million)
based on 2012-2014 data. The various studies have been
conducted to study the temporal trend of different cancer
sites other than childhood cancer in Delhi [5,6]. We
examined the patterns and temporal trend of childhood cancer
in urban Delhi from 1990-2014.
METHODS
The study is based on data extracted from
Delhi PBCR, one of the oldest cancer registries of India
established in 1986, for all new childhood cancer cases
diagnosed between 1990 and 2014. The new cases of top five
childhood cancers – Leukaemia (C91-C95), Lymphoma (C81-C85,
C96), Central Nervous System (C70-C72), Bone (C40-C41), and
Retinoblastoma (C69) were summarized according to gender
into five 5-year period (1990-1994, 1995-1999, 2000-04,
2005-2010, 2010-2014). This registry fulfilled the IARC data
quality standards and the data was published in cancer
incidence in five continents volumes IX and volume X [7,8].
The international classification of disease for oncology
(ICD-O) code 9th revision was used for the period 1988-2000
and 10 th
revision was utilized for the period 2001-2014.
According to the 2011 census, the total
population of Delhi was 1,67,53,235 with 97.5% of people
living in urban areas. Out of these, 0-14 years population
was 45,65,319 and about 97.1% of 0-14 them live in urban
areas of Delhi.
The target population for 0-14 years used
in determining the incidence rates of respective years was
estimated from the 1991, 2001, 2011 census reports of India
using difference distribution method [9,10]. These estimates
were not adjusted for immigration and fertility changes over
the period due to non-availability of adequate data. ASIRs
were calculated by the direct method using WHO World
standard population distribution, year 2000 [11].
Joinpoint regression model using
joinpoint regression programme [12] was applied to assess
the magnitude of time trends on the ASIRs of top five
childhood cancers and total childhood cancer during
1990-2014 according to gender. ASIR was determined using the
formula: Number of new childhood cancer cases in a specific
age-group during a period*1000,000/Estimated population of a
specific age group during the period.
Simple linear regression was performed to
assess the trend of relative proportion of new childhood
cancer cases to all age-group cancers. The percentage
increase in top-five new childhood cancer cases was
calculated by: (childhood cancer cases during 2010-2014
minus childhood cancer cases during 1990-1994) *100
/Childhood cancer cases 1990-1994. The median age was
determined using the median formula for group data on
combined 25-years data.
The estimated annual percentage changes
(EAPCs) in cancer incidence rates was calculated by fitting
a jointpoint regression model, assuming a constant rate of
change in the logarithm of the annual ASIRs in each segment.
The significance of EAPC was tested using asymptotic t-test
and considered significant at 5% if 95% Confidence interval
(CI) of EAPC does not include zero. The connecting points of
the jointpont segment was treated as break. For 25-data
points, joinpoint software recommended a maximum 4
joinpoints. This started with a minimum zero i.e
straight line. Monte Carlo permutation test with 4499
randomly permuted data sets was applied to test the
additional requirement of joinpoint, the obtained P-value
was adjusted according to Bonferroni correction due to
multiple comparisons [13]. ASIRs show a rising trend when
the point estimate and lower limit of 95% CI are >0. In
contrast, a decreasing trend can be seen when the point
estimate and upper 95% CI are <0. Else, the ASIRs are deemed
to be stable over the time period. The multiple comparisons,
asymptotic t-test and Monte Carlo permutation test are part
of joinpoint software [12].
RESULTS
In 1990-2014, Delhi PBCR registered
12,637 new childhood cancer cases (8484 boys and 4153
girls). The proportion of childhood cancer was 4.2% relative
to total cancers of all-age groups. Childhood cancer amongst
boys relative to all age-groups cancer was almost double
than in girls (5.62% vs. 2.78%) while the ratio of
population of boys and girls was 1.14 to 1 during this
period. The combined five top childhood cancer during
1990-2014 were leukemia [C91-C95], lymphoma [C81-C85], CNS
tumors [C70-C72], bone tumors [C40-C41] and retinoblastoma
[C69] (Table I). The boys observed a similar sequence
of top-five childhood cancer during the recent three
five-year intervals. While, girls observed different
sequence, (leukemia, CNS tumors lymphoma, bone tumors and
retinoblastoma). Top five childhood cancers contributed
nearly 80% among boys and 70% among girls respectively.
Leukemia was a prominent cancer in both gender and
contributed 36.1% (approximate one-third) of total childhood
cancer cases (Table I). The proportion of childhood
cancer to total cancer of all age groups revealed a
significant linear decreasing trend in both boys and girls.
This percentage of childhood cancer decreased from 6.6% to
4.7% in boys and 3.6% to 2.6% in girls respectively from
1990 to 2014 (Suppl. Fig. 1). Median age at
diagnosis of childhood cancer for boys was 6 years and for
girls 7 years while in combined it was 6 years.
Table I Proportion of Childhood Cancer Cases During 1990-2014 in Delhi
| Type of Childhood
|
Boys |
Girls |
Total |
| Cancer |
n=8484 |
n=4153 |
n=12637 |
| Leukemia |
3127 (36.9) |
1438 (34.6) |
4565 (36.1) |
| Lymphoma |
1517 (17.9) |
376 (9.0) |
1893 (15.0) |
| Central nervous system |
997 (11.8) |
498 (12.0) |
1495 (11.8) |
| Bone |
570 (6.7) |
351 (8.4) |
921 (7.3) |
| Retinoblastoma |
434 (5.1) |
232 (5.6) |
666 (5.3) |
|
Other typesa
|
1839 (21.7) |
1258(30.3) |
3097 (24.5) |
| All values
in no. (%). aOther types of childhood cancer. |
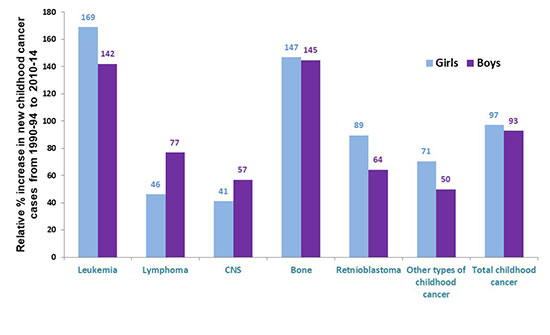
Over the period of 1990-94 to 2010-14,
the percentage increase in new childhood cancer cases was
almost similar for both the gender (97% vs. 93%). The girls
observed higher percentage change in leukemia,
retinoblastoma, and other cancers sites, while lymphoma, and
CNS tumors was more in boys during 2010-14 relative to
1990-94. The percentage increase of bone cancer was almost
similar in both genders (Fig. 1).
 |
|
Fig. 1 Comparison of relative
percentage change in top-five childhood incidence
cases from1990-94 to 2010-2014 between boys and
girls.
|
The age specific (0-4,5-9,10-14, and 0-14
year) distribution of top-five childhood cancer over the
25-year period (1990 to 2014) was similar in boys and girls
except for lymphoma which was more frequent in boys.
Retinoblastoma was more common in children <10 years.
Although girls had higher counts under five-year compared to
the remaining two five-year age groups albeit in boys under
5-year and 5-9 years age-group had similar number of cases.
The age-specific incidence rate per one million of childhood
cancer was higher in 0-4 years as compared to two subsequent
5-year intervals among both gender (Suppl. Fig. 2).
The age-period graphs for top-five
cancers as well as total childhood cancer according to
gender are included as Suppl. Fig. 3
and 4. In boys, total childhood cancer and leukemia
had an upward incidence pattern in recent two periods than
the remaining three periods in nearly all the three
childhood age groups. In girls, total childhood cancer,
leukemia and bone cancers showed increasing trend in all
childhood age groups from 2005 to 2014 (Suppl. Fig. 2
and 3). Lymphoma was more frequent in 5-9 years
age-group, bone in 10-14 years age-group, and retinoblastoma
in 0-4 year age groups among the boys, similar pattern of
these sites was observed among the girls.
Table II Age-standardized Rates and Time Trend of Five Top-Childhood Cancers
in Delhi Urban Area by Sex: 1990-2014
Cancer type
|
Age-standardized incidence rate/ million
population/yearb |
Estimated annual percentage change [EAPC(95%CI)] |
|
1990-94 |
1995-99 |
2000-04 |
2005-09 |
2010-14 |
1990-2014 (95% CI)b |
Trend-1 |
Trend-2 |
| Boys |
|
|
|
|
|
|
|
|
| Leukemia [ C91-C95] |
50.8 |
46.0 |
50.1 |
65.7 |
82.1 |
60.2 (58.0 to 62.3) |
-1.27 (-5.06 to 2.67)a
[1990 to 1999] |
4.58 (3.16 to 6.01) b
[1999-2014] |
| Lymphoma [C81-C85,C96] |
27.5 |
23.2 |
27.4 |
31.4 |
31.9 |
28.5 (27.1 to 30.0 |
1.25 (-0.006 to 2.3) a |
|
| CNS [ C70-C72] |
20.3 |
16.6 |
16.1 |
21.2 |
21.2 |
19.1 (17.9 to 20.3) |
-3.20 (-8.1 to 1.90)a
[1990-2000] |
3.10 (6.5 to 5.6)c
[2000-2014] |
| Bone [ C40-C41] |
8.3 |
8.7 |
10.1 |
12.0 |
12.8 |
10.6(9.8 to 11.5) |
2.51 (0.88 to 4.16)c |
|
| Retinoblastoma [C69] |
8.5 |
9.1 |
7.5 |
9.0 |
9.9 |
8.8(8.0 to 9.64) |
1.09 (-0.73 to 2.94) a |
|
| Other CC |
35.2 |
40.3 |
36.5 |
32.8 |
35.8 |
36.1 (34.41 to 37.7) |
0.41 (-0.53 to 1.36)a |
|
| Total |
150.5 |
143.9 |
147.8 |
172.2 |
193.6 |
163.2 (159.8 to 166.7) |
1.53 (0.87 to 2.13)b |
|
| Girls |
|
|
|
|
|
|
|
|
| Leukemia [C91-C95] |
23.8 |
29.1 |
23.23 |
34.4 |
45.0 |
32.1 (30.1 to 33.4) |
0.37 (-3.06 to 3.92) a
[1990-2004] |
7.06 (2.7 to
11.6)c[2004-2014] |
| Lymphoma [C81-C85,C96] |
9.1 |
7.4 |
7.1 |
8.3 |
9.2 |
8.0 (7.4 to 9.01) |
0.41 (-1.29 to 2.14) a |
|
| CNS [C70-C72] |
13.3 |
10.1 |
10.2 |
8.3 |
13.0 |
10.9 (9.9 to 11.9) |
-2.6(-4.7 to
-0.44)c[1990-2008] |
10.3 (-0.27 to 21.96); a
[2008-2014] |
| Bone [C40-C41] |
6.8 |
5.3 |
6.2 |
7.8 |
10.9 |
7.5 (6.7 to 8.3) |
3.2 (1.61 to 4.79) b |
|
| Retinoblastoma [C69] |
5.2 |
5.0 |
3.4 |
5.3 |
7.5 |
5.3 (4.6 to 6.0) |
1.92 (-0.76 to 4.80) a |
|
| Other CC |
30.2 |
28.4 |
27.5 |
24.1 |
30.0 |
28.0 (26.4 to 29.5) |
-0.16 (-1.32 to 1.02)a |
|
| Total |
88.3 |
85.3 |
77.7 |
88.1 |
115.6 |
91.6 (88.8 to 94.4) |
-0.99 (-2.65 to 0.71) a
[1990-2005] |
6.04 (2.87 to 9.31) d
[2005-2014] |
| b
age-standardized to the WHO World standard
population, year 2000[11] : CNS = Central Nervous
System. aP>0.05; bP<0.001; cP<0.05; dP=0.001. |
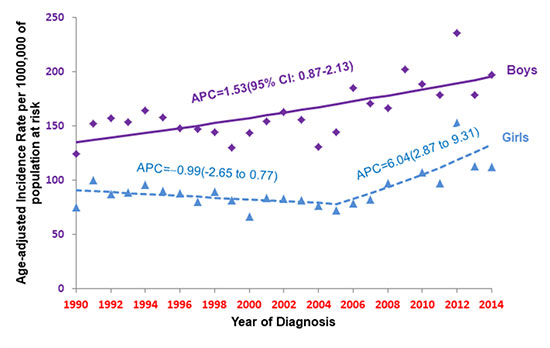
The ASIRs of childhood cancer was 163.2
per one million (95% CI:159.8-166.7) in boys and 91.6 per
one million (95% CI:88.8-94.4) in girls. (Table II).
The trend analysis showed a significant increase in ASIRs of
childhood cancer, EAPC 1.53% (95% CI: 0.87 to 2.13) in boys
and observed one break among girls, the trend remained
stable between 1990-2005, but increased more rapidly with
6.0% per year these after (Fig. 2, Table II). For
pooled data, no change in ASIRs trend was seen till 2004,
but a significant rise was observed with EAPC 4.0% per year
in recent decade (2004-2014) [data not shown].
 |
|
Fig. 2 Trend of
age-standardized (world population, per one million)
incidence rates for childhood cancer in Delhi urban
area between 1990 to 2014 (trend modelled using
joinpoint regression).
|
The childhood cancer trends varied
according to cancer site as well as by gender. In boys,
upward trends were observed for lymphoma (EAPCs= 1.25% per
year), and for bone tumors (EAPC 2.51% per year). However,
leukemia and CNS tumors observed no change between 1990 and
1999, but found a positive significant trend with EAPC of
4.6% per year and 3.1% per year from 1999 to 2014. The girls
showed a different trend than boys; one break was observed
in CNS tumors with a 2.6% decrease in EAPC from 1990 to 2007
and remained stable since then (Table II). Leukemia
also observed one break with a stable incidence trend
between 1990-2004 and a sharp upward trend in recent decade
with EAPC of 7.0% per year. Bone tumors had a significantly
rising with EAPC of 3.2% per year during 1990-2014.
Lymphoma, retinoblastoma and other childhood cancers sites
depicted a consistent flattening trend over the period.
DISCUSSION
The percentage of new childhood cancer
cases to total cancer cases were significantly decreasing in
both genders. This may due be to the falling trend of
fertility rate and growing trend of expectancy of age in
Delhi as well as in India [14]. The total fertility rate
decreased from 4.83 in 1980 to 2.3 in 2015 as per United
Nation websites [15]. In Indian urban areas, life expectancy
at birth increased from 65.4 during 1990-94 to 71.5 during
2010-2014. The life expectancy at birth in Delhi during
2010-14 was 73.5 [16].
ASIRs of childhood cancer showed an
increasing trend during 1990-2014 in boys and in girls
during 2005-2014. Our results of rising trend of new
childhood cancer cases was akin to Canada [17], Australia,
and Taiwan [18,19] (Suppl. Table I). To the best of
our knowledge, no Indian study has assessed the time trend
analysis of new childhood cancer cases, albeit one study
reported rising trend in childhood cancer among the Indian
PBCRs comparing three time periods [20]. Leukemia
contributed to 36.1% of total childhood cancer cases as also
seen in Canada [32.4%; 1992-2010], Australia [32.4%;
1983-2006], Taiwan [33.9%; 1996-2010], Estonia
[31.1%;1970-2016], Thailand [36.1%: 1990-2011].
[17-19,21-22]. Globally, the next two commonest childhood
cancers are CNS tumors with range 13.9%-22.7%, followed by
lymphoma with range 10%-11.2%, albeit in urban Delhi
lymphoma and CNS tumors account for with a percentage of
15.0% and 11.0% of all the childhood cancer cases
respectively [17-20]. However, in Chennai lymphoma and CNS
tumors account for 20% and 11% of all childhood cases
respectively [23].
ASIR for childhood cancer in Delhi was
129.8 per one million [95% CI: 127.6-132.1] from 1990-2014
which is closer to the Taiwan (125.0 per one million from
1996-2010) [19] and lower than United States (172.8 per one
million between 2007 and 2011) [24] and Australia (157.5 per
one million from 1997-2006) [18].
The etiology of childhood cancer is still
limited, some of the factors like environmental exposure,
genetic, parental smoking, higher birth weight, and high
maternal age are associated with most childhood cancers
[25,26]. A large US case-control study reported an increase
of 8% in overall childhood cancer risk for each 5-year
increase in maternal age [27]. Likewise, an increasing trend
in median marriage age was observed in India [28]. The main
reasons for increasing median age are rise in female
workforce and higher education enrolment of females
especially in urban India [28]. Indirectly, the median age
of first-time mother showed an increasing trend but exact
magnitude cannot be estimated.
The change in trends could also be
influenced due to shift in coding or registration practices
and improvement in diagnostic advancement during the period.
The immigrants might also contribute to increase in new
childhood cancer cases. Immigration in Delhi steadily
increased from 6.34 lakhs during 1961-1971 to 22.2 lakhs
during 2001-2011 [29]. However, effect of this increase on
childhood cancer cannot be ascertained due to
non-availability of data.
The main strength of Delhi PBCR is almost
complete coverage and collection high-quality data. The
Delhi PBCR data is also included in the International Agency
for Research on Cancer scientific publications [7,8].
Although Delhi PBCR collects the data of only those patients
who have been residing for at least one year in Delhi but
veracity cannot be confirmed. The projected population of
each year to calculate the ASIRs does not adjust for
immigration and fertility changes over the years which may
over-estimate the incidence rate. The subgroups of leukemia
and lymphoma trend could not be observed due to a small
number of cases. Age-period-cohort (APC) model that assess
the effect of age, effect of period, and effect of cohort on
the incidence, was not performed in the present study. The
join point analysis developed by National cancer Institute,
USA, is a robust method to assess the trend analysis
especially for cancer incidence and mortality data [12,13].
The trend of overall new childhood cancer
cases showed a significant increase especially in the latest
decade in Delhi for boys and girls. The contribution of
childhood cancer to total cases showed a decreasing trend
during this period. Compared to girls, boys had doubled
childhood cancer cases during 1990-2014. Leukemia is the
most common cancer site and contributed to one-third of
total childhood cancers during the 25-year period. The trend
and knowledge of present status of childhood cancer helps
the public health policy makers as a baseline for future
planning and allocation resources.
Note: Supplementary material related
to this study is available with the online version at
www.indianpediatrics.net
Contributors: All authors approved
the final version of manuscript, and are accountable for all
aspects related to the study.
Funding: None; Competing interest:
None stated.
|
WHAT THIS STUDY ADD?
•
There is approximate
100% increase in incidence of reported childhood
cancer cases from 1990-94 to 2010-2014 in urban
Delhi.
•
Median age at diagnosis of childhood cancer in
Delhi is 6 years.
|
REFERENCES
1. Steliarova-Foucher E, Colombet M, Ries
LAG, et al. International incidence of childhood cancer
2001-10: A population-based registry study. Lancet Oncol.
2017;18:719-31.
2. Gupta S, Howard SC, Hunger SP, et al.
Treating childhood cancer in low-and middle-income
countries. In: Gelband H, Jha P, Sankaranarayanan R,
et al. editors Cancer: Disease control priorities,
Volume 3. The International Bank for Reconstruction and
Development World Bank; 2015 Chapter 7. Accessed February
20, 2020. Available from:
https://www.ncbi.nlm.nih.gov/books/NBK343626/
3. World Health Organisation. CANCER
TODAY International agency for research on cancer. Accessed
February 20, 2020. Available from:
https://gco.iarc.fr/today/online-analysis-table.
4. Report of National Cancer Registry
Programme. National Centre for Disease Infromatics and
Research, Bengaluru, India. 2020. Accessed February
20, 2020. Available from:
https://www.ncdirindia.org/All_Reports/Report_2020/default.aspx
5. Malhotra RK, Manoharan N, Nair O, Deo
SVS, Rath GK. Trends and future burden of Tobacco related
cancers incidence in Delhi urban areas: 1998-2001. Indian J
Public Health. 2019;63:33-8.
6. Malhotra RK, Manoharan N, Nair O, et
al. Trends in Lung cancer incidence in Delhi, India
1998-2012: Age-period-cohort model and joinpoint analyses.
Asian Pac J Cancer Prev 201819:1647-54.
7. Curado MP, Edwards B, Shin HR, et al,
eds (2007). Cancer Incidence in five continents Vol. IX IARC
scientific publication no. 160: 2007. P. 229.
8. Forman D, Bray F, Brewster DH, et al.
editors. Cancer Incidence in five continents Vol. X IARC
scientific publication no. 164, IARC: 2014. P. 550.
9. Census of India, Registrar General of
India. C-13 tables single year age data. Accessed November
24, 2019. Available from:
https://www.censusindia.gov.in/2011
census/population_enumeration.html.
10. Takiar R, Shobana B. Cancer Incidence
rates and the problem of denominators - A new approach in
Indian cancer registries. Asian Pac J Cancer Prev. 2009;
10:123-6.
11. Ahmad OB, Boschi-Pinto C, Lopez
AD, Murray CJL, Lozano R, Inoue M. Age standardization of
rates: A new WHO standard. World Health Organization; 2001.
Accessed November 9, 2019. Available from:
http://www.who.int/ healthinfo/paper31.pdf
12. Joinpoint Regression Program, Version
4.8.0.1 - April 2020; Statistical Methodology and
Applications Branch, Surveillance Research Program, National
Cancer Institute.
13. Kim HJ, Fay MP, Feuer EJ, Midthune
DN. Permutation tests for joinpoint regression with
applications to cancer rates. Stat Med. 2000;19:335-51.
14. Pandey MM, Tiwari R, Choubey A.
Population dynamics in India. International Journal of
Scientific and Engineering Research. 2015;6:2106-33.
15. United Nation. Department of Economic
and social affairs population dynamics. Accessed August 15,
2020. Avail-able from:
https://www.population.un.org/wpp/
download/standard/fertility
16. Census of India, Registrar General of
India. Abridged table 2010-2014. Accessed July 10, 2020.
Available from: https:
//www.censusindia.gov.in/VitalStatistics/SRSLife Table/
17. Xie L, Onysko J, Morrison H.
Childhood cancer incidence in Canada: Demographical and
geographic variation of temporal trend (1992-2010). Health
Promot Chronic Dis Prev Can. 2018;38:79-113.
18. Baade PD, Youlden DR, Valery PC, et
al. trends in incidence of childhood cancer in Australia,
1983-2006. Br J Cancer. 2010;102:620-6.
19. Liu YL, Lo WC, Chiang CJ, et al.
Incidence of cancer in childhood aged 0-14 years in Taiwan
1996-2010. Cancer Epidemiol. 2015;39:21-8.
20. Das S, Paul DK, Kumar A, Bhakta S.
Childhood cancer incidence in India Between 2012 and 2014:
Report of a population-based cancer registry. Indian Pediatr.
2017;54:1033-36.
21. Paapsi K, Baburin A, Mikkel S.
Childhood cancer incidence and survival trends in Estonia
(1970-2016); Nationwide population Based study. BMC Cancer.
2020:30:doi.org/10.1186/212885-019-6510-7.
22. Peterson CC, Demanelis K, Rentschler
K, et al. Childhood cancer incidence and survival in
Thailand: A Compre-hensive population-based registry
analysis, 1990-2011. Pediatr Blood Cancer. 2019;66:e27428.
23. Swaminathan R, Rama R, Shanta V.
Childhood cancers in Chennai, India, 1990-2001: Incidence
and survival. Int J Cancer. 2008;122:2607-11.
24. Linabery AM, Ross JA. Trends in
childhood cancer incidence in US (1992-2004). Cancer.
2018;112:416-32.
25. Kaatsch P. Epidemiology of childhood
cancer. Cancer Treat Rev. 2010;36:277-84.
26. Eden T. Aetiology of childhood
leukaemia. Cancer Treat Rev. 2010;36:286-97.
27. Johnson KJ, Carozza SE, Chow EJ, et
al. Paternal age and risk of childhood cancer: A pooled
analysis. Epidemiology. 2009;20:475-83.
28. Park K. Demography and family
planning. In: Park’s Textbook of Social & Preventive
Medicine. Banarsidas Bhanot; 2015.P.479-519.
29. National Capital Region Planning
Board. Study on counter magnet areas to Delhi and NCR, 2008.
Chapter 2: Migration study of Delhi and NCR. Assessed March
22, 2020. Available from: http://ncrpb.nic.in/pdf_files/05_chapter%202_cma.pdf
|
|
|
 |
|

