|
|
|
Indian Pediatr 2020;57:
469-470 |
 |
Developmental Delay with Intermittent Twisting of Neck
|
|
Rangan Srinivasaraghavan and Samuel P Oommen*
Developmental Pediatrics unit, Christian Medical College and
Hospital,
Vellore, India.
Email:
[email protected]
|
|
The hallmark of cerebral palsy (CP) is the presence of pyramidal
or extra-pyramidal signs [1]. There are many disorders that can mimic CP
[2]. One such mimicking condition is high cervical cord compression due
to anomalies of the spinal cord [3].
A two-year-old boy, second
of twins born of non-consanguineous marriage, was brought with inability
to stand. He was delivered at eight months of gestation with a weight of
1.5 kg and no significant neonatal complications. His motor milestones
were significantly delayed compared to his twin and spasticity was
noticed from six months of age. The parents reported stiffness of his
neck and limbs which was more on waking up, which would decrease within
a few minutes. There were no seizures or regression of milestones. He
was diagnosed to have mixed (spastic-dystonic) cerebral palsy. His
language and social skills were age appropriate. At presentation, he was
using two- word phrases and had attained daytime bowel and bladder
control.
On examination, weight, height and head circumference
were within normal limits. There were no obvious dysmorphic features.
His upper segment to lower segment ratio was 0.92 suggestive of truncal
shortening. His vision and hearing were normal. There was hypertonia in
all the four limbs and brisk deep tendon reflexes. The plantar responses
were extensor bilaterally. Examination of the other systems was
unremarkable.
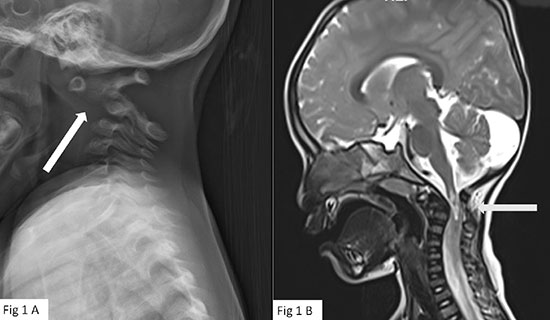 |
| Fig. 1 (a) X-ray
Cervical spine lateral view flexed position showing
widened pre-dentate space (white arrow); (b)
MRI T2 weighted image sagittal section showing
compression of the cord at C1 level (grey arrow). |
Lateral X-ray of the neck (Fig. 1a) showed anterior
dislocation of C1 vertebra. The pre-dentate space was widened
and measured 13 mm. MRI did not show any periventricular or
basal ganglia changes. MRI of the cervical spine (Fig. 1b)
(confirmed atlanto-axial dislocation (AAD) causing compressive
myelopathy at C1 level, without any other spinal malformations.
Neurosurgeon prescribed neck collar, and advised follow-up for
cervical spine stabilization. In view of the truncal shortening
and AAD, he was also advised evaluation for skeletal dysplasia,
but the parents deferred it to a later date.
Conditions
which mimic CP should be considered – when there is absence of
definite preceding perinatal insult; there is family history of
developmental delay and spasticity; there is developmental
regression or onset of new clinical signs of upper motor
involvement; and when there is associated significant ataxia,
muscle atrophy, or sensory loss [2]. Although neuroimaging is
not essential for making a diagnosis of CP, MRI brain is
abnormal in more than 80% of children with CP [4]. Current
Western guidelines recommend MRI in children suspected to have
CP [1]. The imaging not only uncovers the pathogenic patterns
responsible for the CP but can also detect structural
malformations of the brain and neuro-metabolic problems which
resemble CP [4].
Despite significant perinatal risk
factors, the inter-mittent abnormal neck stiffness warranted
meticulous examination and evaluation [3], which revealed AAD
can be idiopathic or due to traumatic, inflammatory or genetic
disorders like Down syndrome, achondroplasia, cleido-cranial
dysplasia and Morquio syndrome [4]. Neuro-logical manifestations
of congenital AAD in children result from progressive
compression of the cervico-medullary junction and present as
progressive quadri-plegia. Patients with myelopathy may go
undiagnosed for a long period because of very slow progression
of the disease process [3] and maybe mistakenly diagnosed as CP.
Trauma or sudden movement can worsen symptoms in AAD. In the
reported child, the increase in stiffness upon getting from
sleep could possibly be due to the fact that while he was lying
down, neck positioning could have caused an increase in
stiffness. Poor cervical posture during sleep could cause
increased biomecha-nical stresses on the structure of the
cervical spine and could result in cervical pain and stiffness
[5].
This case highlights compressive myelopathy as a
differential for CP, and underscores the importance of a good
history-taking in all patients, especially those labelled as
cerebral palsy.
Contributors: Both authors were involved
in clinical care, literature search and manuscript preparation.
Funding: None; Competing interest: None Stated.
References
1. Himmelmann K, Horber V, De
La Cruz J, Horridge K, Mejaski-Bosnjak V, Hollody K, et al. MRI
classification system (MRICS) for children with cerebral palsy:
Development, reliability, and recommendations. Dev Med Child
Neurol. 2017;59:57-64.
2. Appleton RE, Gupta R. Cerebral
palsy: Not always what it seems. Arch Dis Child.
2019;104:809-14.
3. Ginsberg L. Myelopathy: Chameleons
and mimics. Pract Neurol. 2017;17:6-12.
4. Jain VK.
Atlantoaxial dislocation. Neurol India. 2012;60:9-17.
5.
Lee W-H, Ko M-S. Effect of sleep posture on neck muscle
activity. J Phys Ther Sci. 2017;29:1021-4.
|
|
|
 |
|

