|
|
|
Indian Pediatr 2017;54: 413 -415 |
 |
Incomplete MillerFisher Syndrome with
Advanced Stage Burkitt Lymphoma
|
|
Zeynep Canan Özdemir,
#Yeter
Düzenli Kar, $Coşkun
Yarar, Suzan
Şaylısoy and *Özcan Bör
From Division of Pediatric Hematology, #Department
of Pediatrics, $Division of Pediatric Neurology, Department
of Radiology, and *Division of Pediatric Oncology; Eskişehir
Osmangazi University Faculty of Medicine,Turkey.
Correspondence to: Dr Zeynep Canan
Özdemir, Division of Pediatric Hematology/Oncology, Eskiºehir Osmangazi
University Faculty of Medicine, 26480, Eskipehir, Turkey.
Email: efecanan@yahoo.com
Received: June 17, 2016;
Initial review: November 03, 2016;
Accepted: February 28, 2017.
|
Background: Lymphoma-associated incomplete Miller-Fisher syndrome is
very rare. Case Characteristics: An 11-year-old boy who initially
presented with headache, left ptosis, diplopia and weakness. Neurologic
examination indicated left sided ptosis with ophthalmoplegia.
Observations: Cerebral imaging and cerebrospinal fluid examinations
were normal. Magnetic resonance imaging of the abdomen showed a mass
lesion in the ileal loops. A bone marrow biopsy showed infiltration by
Burkitts lymphoma. Message: Burkitt lymphoma may present with
incomplete Miller Fisher syndrome.
Keywords: Leukemia, Ophthalmoplegia, Ptosis.
|
|
Paraneoplastic neurological syndromes (PNS) are
rare disorders triggered by an altered immune system response to a
neoplasm. They are defined as clinical syndromes involving
non-metastatic systemic effects that accompany malignant disease [1].
PNS affect less than 0.01% patients with cancer [2]. Small-cell lung
cancer, breast cancer and ovarian cancer are the most frequent solid
tumors associated wih PNS [3]. Hematological malignancies such as
non-Hodgkin lymphoma are rarely accompanied by PNS affecting the central
and peripheral nervous systems [1]. There are some reports on the
association of non-Hodgkin lymphoma and PNS [2-6], but Miller-Fisher
Syndrome (MFS) is extremely rare [6].
Case Report
The patient was an 11-year-old boy who was
hospitalized in our emergency department with complaints of headache,
left ptosis, diplopia and weakness that started within the previous two
days. Neurologic examination indicated unilateral left ptosis with
ophthalmoplegia. Fundus examination and deep tendon reflexes were
normal. Complete blood count, peripheral blood smear and serum
electrolyte results were normal. Serology results for Hepatitis A, B and
C; cytomegalovirus; Epstein Barr virus; parvovirus; and human
immunudeficiency virus were negative. Chest X-ray, cranial
magnetic resonance imaging (MRI), cranial magnetic resonance angiography
and orbital computed tomography (CT) results were normal. Cerebrospinal
fluid (CSF) results were: protein 22 mg/dL, glucose 71 mg/dL, and no
malignant cells. Brucella and lyme serology results were negative. The
oligoclonal band analysis was negative for multiple sclerosis. CSF
paraneoplastic panel (anti-amphiphysin, anti-CV2.1, anti-Ma2/Ta,
anti-RI/ANNA-2, anti-Yo/PCA-1, anti-Hu/ANNA-1, anti-RECOVERIN and
anti-SOX1 antibodies) results were negative. We planned to
administer one dose of 1 g/kg intravenous immunoglobulins (IVIG) in view
of initial diagnosis of incomplete MFS. Only 50% of the targeted dose
could be administered because patient experienced severe abdominal pain.
There was no improvement in ptosis and eye movements. Physical
examination showed a 3-4 cm mobile mass in the right lower abdominal
quadrant. Lactate dehydrogenase was 1092 U/L and amylase was 496 U/L. An
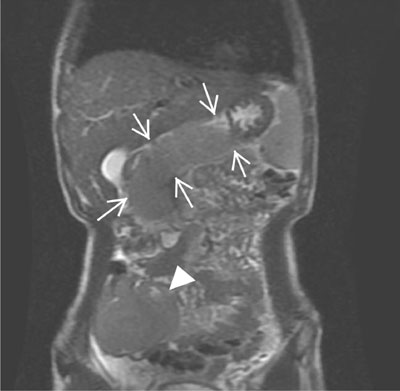
abdominal MRI revealed diffuse pancreatic involvement and a mass lesion
of 7×5 cm in the ileal loops at the lower right quadrant (Fig.
1). Lumbar and dorsal MRI revealed involvement in the L3-L4 and
T3-T8 vertebral bodies and leptomeningeal dissemination in the spinal
cord along the thoracic vertebrae. Fluorodeoxyglucose-positron emission
tomography showed intense uptake foci on both humeri, the vertebral
column, pelvic bones, and both femurs and proximal tibias, indicating
malignant involvement. Bone marrow aspirate revealed lymphoblasts
containing cytoplasmic vacuoles at a rate of 30%. A bone marrow biopsy
revealed CD20, PAX5, bcl6 and CD34, and TDT-negative infiltration of
Burkitt lymphoma in 30% of the bone marrow. Thus, bone marrow
involvement in Burkitt lymphoma was confirmed, and a diagnostic of
Burkitt leukemia was made. Chemotherapy was started and the patients
symptoms resolved completely after two cycles of chemotherapy (Fig.
1b).
 |
|
Fig. 1 Axial abdominal magnetic resonance imaging
showing diffuse pancreatic involvement (arrows) and a mass
lesion in the ileal loops (arrowhead).
|
Discussion
MFS is typically characterized by a triad of ataxia,
areflexia and ophthalmoplegia, which is considered to be a variant of
Guillain Barré Syndrome. The annual incidence of MFS is 0.09
cases/100.000 population [7]. Diplopia is the most common initial
symptom in MFS, and it arises because of acute onset of external
ophthalmoplegia. Most patients with MFS exhibit bilateral, relatively
symmetrical ophthalmoplegia, but the condition can also be unilateral
[7]. Although most published reviews define MFS strictly as an acute
monophasic illness featuring the clinical triad of ataxia, areflexia and
ophthalmoplegia, it can present with only one or two of these features
[8]. In our patient, sudden onset ptosis and ophthalmoplegia were
consistent with this syndrome.
The differential diagnosis of MFS includes myasthenia
gravis, botulism, brainstem stroke, infective conditions (listeriosis,
tuberculosis, brucellosis, Lyme disease, herpes simplex virus,
EpsteinBarr virus), autoimmune (multiple sclerosis, sarcoidosis,
Behçets disease, systemic lupus erythematosus), malignancy (lymphoma,
paraneoplastic syndrome), and basal meningitis [9]. In our patient,
extensive diagnostic work-up excluded all other conditions. Several
pathogenetic mechanisms of neuropathy associated with lymphoma have been
suggested. These include direct invasion of lymphoma cells, metabolic
and infectious processes, vascular impairment, and immunological
mechanisms as in paraneoplastic neuropathy [10]. MFS in the form of
multiple cranial neuropathy, ataxia and areflexia has been reported in
patients with B-cell lymphoma [3]. Association of Burkitt lymphoma with
GBS and multiple cranial neuropathy is also reported, but in these
patients, symptoms could be explained by nerve invasion by the tumor
[4,5]. There is an earlier report of in a patient
of Burkitt lymphoma who presented with renal and hepatic involvement
[6]. In this patient, increased levels of protein, but no antibodies,
were found in the CSF [6].
It is not possible to detect antibodies in all patients with
paraneoplastic syndrome. As our patient neither had leptomeningeal
involvement level nor the imaging examinations could explain the cranial
nerve involvement, the possibility of a paraneoplastic syndrome was more
likely. Lack of improvement with IVIG and complete resolution after
chemotherapy also supported a diagnosis of PNS secondary to malignancy.
In conclusion, children may rarely present with
symptoms of PNS secondary to malignancy. In children diagnosed with
incomplete MFS, hematological malignancies should be suspected.
Contributors: ÖZC, DKY, BÖ: reviewed the
literature and wrote the paper; DKY, ÖZC, YC: collected the data; ŞS:
assessed the radiologic finding.
Funding: None; Competing interest: None
stated.
References
1. Bishay RH, Paton J, Abraham V. Variant
Guillain-Barré syndrome in a patient with Non-Hodgkins lymphoma. Case
Rep Hematol. 2015;2015:979237.
2. Lisak RP, Mitchell M, Zweiman B, Orrechio
E, Asbury AK. GuillainBarré syndrome and Hodgkins disease: Three cases
with immunological studies. Ann Neurol. 1977;1: 72-8.
3. Usmani N, Bhatia R, Ikpatt OF, Sharma KR. Diffuse
large B-cell lymphoma presenting as Miller Fisher syndrome. Muscle
Nerve. 2012;45:138-43.
4. Zuk E, Nowacki P, Fabian A. Guillain-Barre
syndrome in patients with Burkitts lymphoma and type 2 diabetes
mellitus. Folia Neuropathol. 2001;39:281-4.
5. Pal L, Valli ER, Santosh V, Menon A,
Veerendrakumar M, Nagaraja D, et al. Disseminated Burkitts
lymphoma presenting as multiple cranial nerve palsies. Indian J Cancer.
1995;32:116-20.
6. Gentile S, Messina M, Rainero I, Lo Giudice R, De
Martino P, Pinessi L. Miller Fisher syndrome associated with Burkitts
lymphoma. Eur J Neurol. 2006;13:430.
7. Smith J, Clarke L, Severn P, Boyce R. Unilateral
external ophthalmoplegia in Miller Fisher syndrome: Case report. BMC
Ophthalmol. 2007;7:7.
8. Snyder LA, Rismondo V, Miller NR. The Fisher
variant of Guillain-Barre´ syndrome (Fisher Syndrome). J
Neuro-Ophthalmol. 2009;29:312-24.
9. Talebi M, Farzi MA, Bavil H. A case of Miller
Fisher syndrome with unusual features: Normal muscle stretch reflexes
and facial palsy and dramatic response to IVIG. J Neurol Stroke.
2016;4:00131.
10. Kelly JJ, Karcher DS. Lymphoma and peripheral neuropathy: A
clinical review. Muscle Nerve. 2005;31: 301-13.
|
|
|
 |
|

